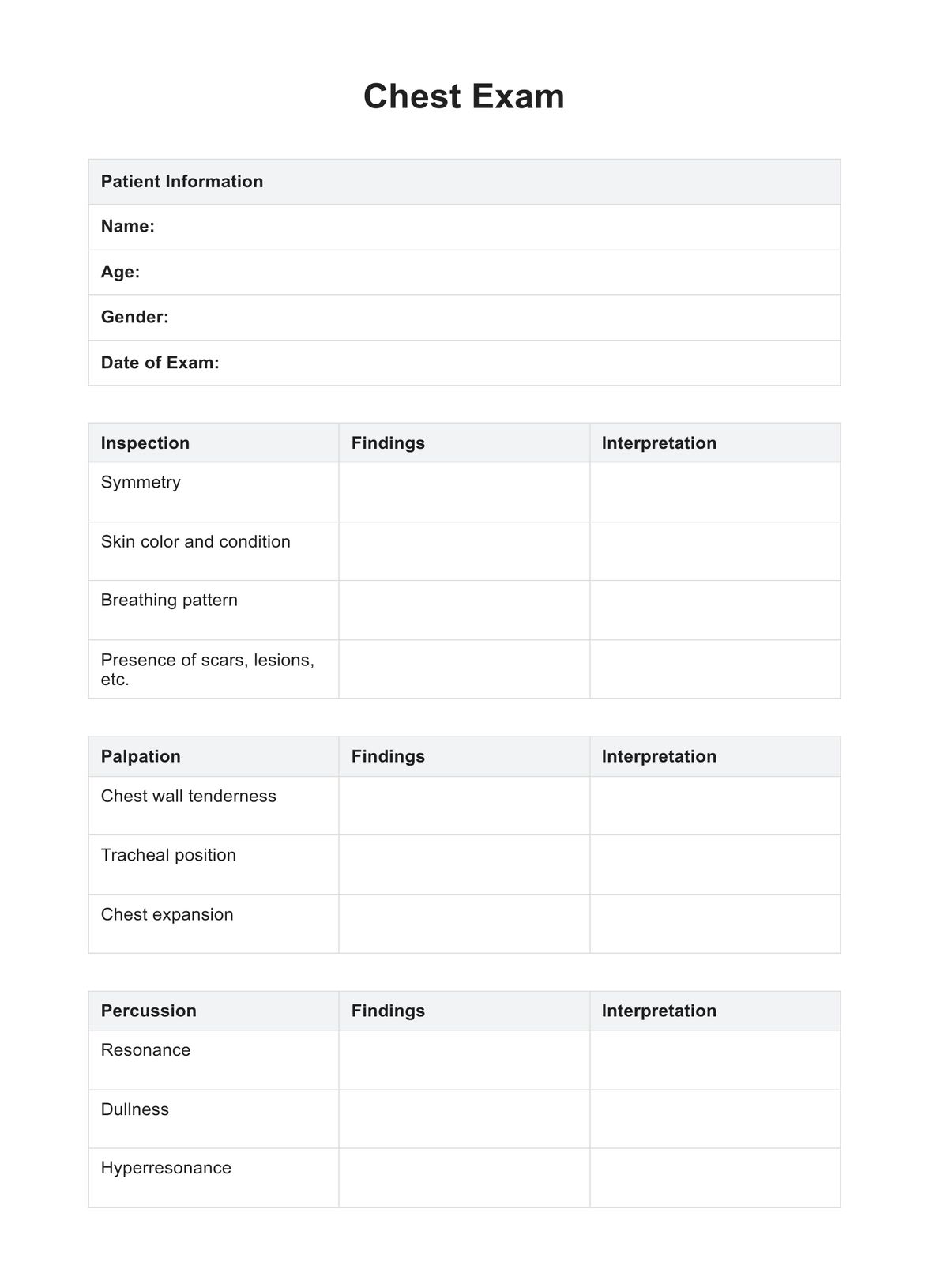
The chest pain workup involves a systematic approach to identify the underlying cause of discomfort. It typically includes a detailed patient history, physical examination, electrocardiogram (ECG or EKG), blood tests, and imaging studies, such as chest X-rays, to ensure a comprehensive assessment.
Chest Pain Workup
Learn about the comprehensive workup for chest pain, including diagnostic tests and evaluations. Download a free PDF example for reference.
Chest Pain Workup Template
Commonly asked questions
The 3 P's of chest pain refer to Provocative factors, Palliative factors, and associated Symptoms. Understanding what provokes or alleviates chest pain, along with noting associated symptoms, assists healthcare providers in forming a clearer diagnostic picture during the assessment.
Key tests for chest pain include an electrocardiogram (ECG or EKG) to assess heart function, blood tests to check for cardiac enzymes and other indicators, and imaging studies like CT scans or chest X-rays. These tests aid in differentiating between cardiac and non-cardiac causes, guiding an accurate diagnosis and appropriate treatment.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











