Healthcare professionals perform skin allergy tests by exposing the skin to suspected allergens through methods like skin prick tests, intradermal tests, or patch tests. Reactions such as redness, swelling, or wheal formation indicate possible allergen sensitivity.
Allergy Skin
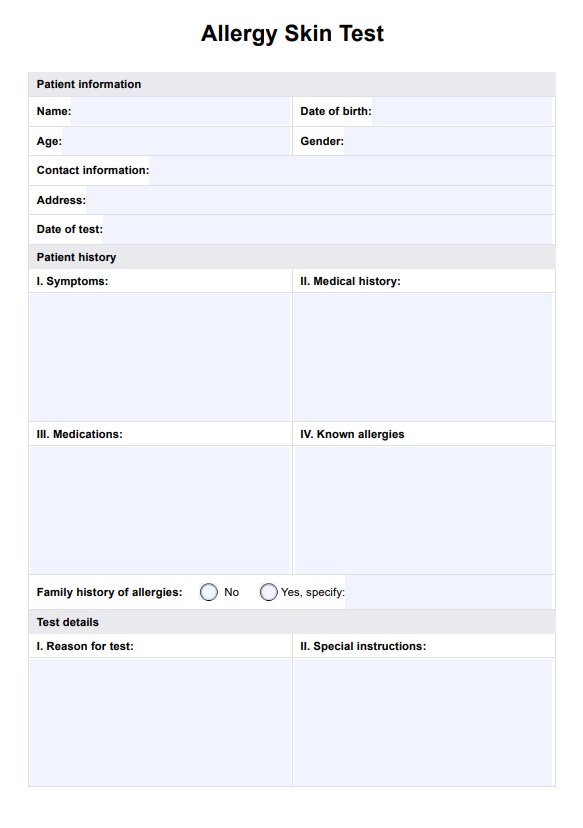
Get our free Allergy Skin Test PDF to assess and diagnose patient allergy reactions properly.
Use Template
Allergy Skin Template
Commonly asked questions
Allergy skin tests cause minimal discomfort, often described as a slight pinch or mild itching at the test site. The sensations are typically brief and subside shortly after the procedure.
Skin allergy testing is generally accurate, with skin prick tests offering high sensitivity and specificity for immediate allergic reactions. However, false positives and negatives can occur, so results should be interpreted alongside a patient’s medical history and clinical presentation.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











