Spinal Accessory Nerve Test
Discover how to conduct a Spinal Accessory Nerve Test with our comprehensive guide and example. Download a free PDF from Carepatron for reference.


What is the spinal accessory nerve?
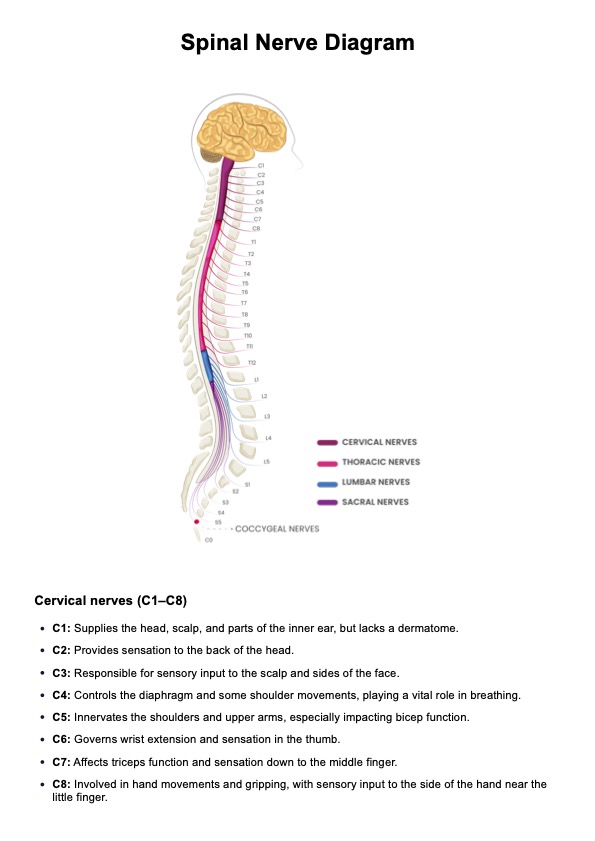
The spinal accessory nerve, also known as Cranial Nerve XI (CN XI) or the accessory nerve, plays a pivotal role in the intricate network of nerves within the human body. Originating from the medulla oblongata and the upper cervical spinal cord, this nerve is unique in that it has both cranial and spinal components.
The cranial part of the spinal accessory nerve emerges from the medulla oblongata, the lowermost part of the brainstem. It then courses through the skull, working with the vagus nerve (Cranial Nerve X) before descending.
Simultaneously, the spinal component of the nerve takes root in the upper cervical spine (specifically, the spinal cord segments C1 to C5). These fibers exit the spinal cord, forming the spinal accessory nerve, and travel to join the cranial component.
The spinal accessory nerve is primarily a motor nerve responsible for controlling specific muscles involved in head and shoulder movements. It innervates the sternocleidomastoid and trapezius muscles, crucial for the rotation and tilting of the head, as well as the elevation, retraction, and depression of the shoulders.
Beyond its mechanical functions, the spinal accessory nerve is integral to maintaining proper posture, enabling us to carry out daily activities that involve head and neck movements. Its role in facilitating coordinated muscle actions emphasizes its significance in sustaining optimal musculoskeletal function.
Purpose of the cranial nerve XI
Cranial Nerve XI, commonly called the spinal accessory nerve, is a multifaceted component of the intricate network of cranial nerves and spinal nerves within the human body. Functioning as a crucial player in the central nervous system (CNS) and the peripheral nervous system (PNS), its purpose is primarily motor, orchestrating movements vital for head and shoulder coordination.
Cranial Nerve XI is distinct in that it possesses both cranial and spinal components. The cranial part collaborates closely with the vagus nerve (Cranial Nerve X) during its course through the skull. This unique integration exemplifies the interconnected nature of cranial nerves and highlights the importance of coordinated functions within the CNS.
Simultaneously, the spinal component of the accessory nerve originates in the upper cervical spinal cord, spanning segments C1 to C5. This segmental connection illustrates the integration of spinal nerves into the broader cranial nerve system. The spinal accessory nerve's primary purpose is to control specific muscles, namely the sternocleidomastoid and trapezius muscles, which are pivotal for head and shoulder movements.
The sternocleidomastoid muscle, innervated by the spinal accessory nerve, facilitates the rotation and tilting of the head. On the other hand, the trapezius muscle, another primary recipient of its fibers, contributes to the elevation, retraction, and depression of the shoulders. This intricate control over muscles associated with these movements highlights the importance of the spinal accessory nerve in maintaining a full range of head and shoulder functions.
Beyond its specific motor functions, Cranial Nerve XI plays a pivotal role in sustaining proper posture, a fundamental aspect of daily life. Its influence on head and shoulder movements is essential for various activities, from simple tasks to complex physical actions.
Spinal Accessory Nerve Test Template
Spinal Accessory Nerve Test Example
What happens when the spinal accessory nerve is damaged?
The spinal accessory nerve, critical for controlling specific muscles in the head and shoulder region, can face damage due to various factors. When the spinal accessory nerve is compromised, it can have distinct consequences, affecting motor functions and overall musculoskeletal coordination.
Impaired control of sternocleidomastoid and trapezius muscles
Damage to the spinal accessory nerve may impair control over the sternocleidomastoid and trapezius muscles. These muscles, crucial for head and shoulder movements, may exhibit weakness or limited functionality. Individuals may experience difficulty turning or tilting their heads and may notice a reduced ability to elevate, retract, or depress their shoulders.
Sternocleidomastoid muscle weakness
The sternocleidomastoid muscle, innervated by the spinal accessory nerve, is particularly susceptible to damage. Weakness in this muscle can manifest as challenges in rotating and tilting the head. Patients may struggle with simple tasks such as looking over their shoulders or tilting their heads sideways, impacting activities that require a wide range of head movements.
Trapezius muscle dysfunction
Damage to the spinal accessory nerve can also affect the trapezius muscle, leading to dysfunction in the shoulder region. Individuals may experience difficulty lifting their shoulders, retracting them backward, or depressing them downward. This dysfunction can notably impact posture and may result in discomfort or pain in the neck and shoulder areas.
Altered coordination with cranial nerves
As part of the intricate cranial nerve system, the spinal accessory nerve collaborates with others, including the vagus nerve. Damage to the spinal accessory nerve may disrupt this coordination, potentially leading to broader issues in the nervous system. Altered communication between cranial nerves can have cascading effects, affecting various motor and sensory functions.
Impact on daily activities and quality of life
Ultimately, damage to the spinal accessory nerve can significantly impact an individual's daily activities and overall quality of life. Simple tasks like turning the head to look at something or lifting the shoulders can become challenging. The broader implications on musculoskeletal coordination emphasize the importance of promptly diagnosing and addressing spinal accessory nerve damage.
What is the Spinal Accessory Nerve Test?
The spinal accessory nerve test is a diagnostic procedure designed to assess the functionality of the spinal accessory nerve (Cranial Nerve XI), a crucial player in controlling specific muscles involved in head and shoulder movements. This test is particularly valuable in neurological examinations, aiding healthcare professionals in identifying potential issues with the spinal accessory nerve and associated musculoskeletal functions.
The objective of the test
The primary objective of the spinal accessory nerve test is to evaluate the integrity and functionality of the accessory nerve's cranial and spinal components. This includes assessing the coordination between the spinal accessory nerve and other cranial nerves, such as the vagus nerve, during specific motor tasks.
Components of the test
The cranial nerve test typically involves examining the strength and coordination of the sternocleidomastoid and trapezius muscles, both innervated by the spinal accessory nerve. During the evaluation, the healthcare professional observes the patient's ability to perform certain movements, such as turning the head, tilting the head sideways, elevating and depressing the shoulders, and retracting the shoulders backward.
Testing procedure
The healthcare provider may instruct the patient to perform various head and shoulder movements while applying resistance. For example, patients may be asked to turn their heads against resistance or lift their shoulders against the applied force. The examiner carefully observes the range of motion, strength, and coordination during these tasks.
Clinical significance
The cranial nerve exam is especially relevant in cases where there are suspicions of nerve damage or neurological disorders affecting the spinal accessory nerve. It aids in diagnosing conditions that may compromise the proper functioning of the sternocleidomastoid and trapezius muscles, such as nerve injuries, compression at the jugular foramen, or vascular issues related to the internal carotid artery.
Differentiating the spinal portion
To specifically assess the spinal portion of the accessory nerve, the examiner may conduct additional tests, such as applying resistance to shoulder shrugging. This helps isolate the spinal component's function, providing a more detailed understanding of its integrity.
How to conduct the test?
Conducting the spinal accessory nerve test requires a systematic approach to assess the functionality of the spinal accessory nerve and associated muscles. Below are the steps to complete the test:
Patient positioning
Ensure the patient is comfortably seated or standing in an upright position. Adequate visibility of the patient's head and shoulders is essential for accurate observation during the test.
Explanation and demonstration
Before initiating the test, explain the procedure to the patient. Demonstrate each movement you will be assessing, emphasizing the importance of following instructions and providing maximal effort during the test.
Cranial nerve nursing assessment
The cranial nerve nursing assessment is where nurses instruct the patient to turn their head to one side against resistance. Place one hand on the side of the patient's face, applying gentle resistance while they attempt to turn their head. Observe for strength, smoothness of movement, and any signs of weakness.
Head tilting
Ask the patient to tilt their head sideways (ear to shoulder) against resistance. Use your hand to provide resistance on the opposite side of the head. Next, evaluate the patient's ability to maintain the tilt and resistance encountered.
Trapezius muscle assessment
There are two steps in testing the trapezius muscle: shoulder shrugging and shoulder retraction and depression.
- Shoulder shrugging: Assess the strength of the trapezius muscle by instructing the patient to elevate their shoulders against resistance. Apply downward pressure on the shoulders while the patient attempts to lift them.
- Shoulder retraction and depression: Check the patient's ability to retract and depress their shoulders. Ask them to pull their shoulders backward against resistance and then push them downward against the applied force.
Interpretation and documentation
Based on the observed movements, assess the strength, coordination, and overall performance of the sternocleidomastoid and trapezius muscles. Document any abnormalities, weakness, or signs of dysfunction, and consider further diagnostic measures if needed.
Next steps
After undergoing a Spinal Accessory Nerve Test, individuals can anticipate a sequence of steps that will aid in the interpretation of results and guide potential follow-up actions:
Results review and analysis
After completing the test, healthcare professionals will meticulously review and analyze the results. This involves assessing the strength, coordination, and overall performance of the sternocleidomastoid and trapezius muscles. A detailed examination will help identify any abnormalities, weakness, or signs of dysfunction associated with the spinal accessory nerve.
Consultation with healthcare provider
Individuals are advised to schedule a consultation with their healthcare provider upon receiving the test results. This step is crucial for obtaining a comprehensive explanation of the findings, discussing potential concerns, and gaining insights into the overall health and well-being implications.
Development of a treatment plan
In the event of identified issues or abnormalities, healthcare providers will collaborate with individuals to formulate a tailored treatment plan. This plan may include physical therapy, exercises to enhance muscle strength or other interventions to address specific concerns related to the spinal accessory nerve.
Ongoing monitoring and follow-up
The journey doesn't conclude with the initial consultation. Continuous monitoring and follow-up appointments may be recommended to track progress, assess the effectiveness of interventions, and make any necessary adjustments to the treatment plan. Regular check-ins ensure a proactive approach to maintaining optimal neurological health.
You can leverage this cranial nerve exam template and cranial nerve test to improve diagnostic accuracy and patient care. This resource provides a detailed framework for assessing each of the twelve cranial nerves, ensuring comprehensive and systematic evaluations.
Commonly asked questions
To test for spinal accessory nerve damage, healthcare professionals conduct a spinal accessory nerve test, assessing the strength and coordination of the sternocleidomastoid and trapezius muscles. Impaired movements during head rotation, tilting, and shoulder actions may indicate potential nerve damage.
Identifying spinal accessory nerves involves neurological examinations and imaging studies such as magnetic resonance imaging (MRI). Skilled healthcare professionals assess the nerve's integrity through clinical evaluations, focusing on the patient's ability to perform specific head and shoulder movements.
Accessory nerve function is assessed through the spinal accessory nerve test, evaluating the strength and coordination of the sternocleidomastoid and trapezius muscles. Healthcare professionals observe the patient's ability to perform controlled head rotations, tilts, and various shoulder movements against resistance to determine the nerve's functionality.