Sensory processing disorder (SPD) is typically diagnosed by an occupational therapist who conducts a thorough evaluation of the individual’s sensory responses and behavior. This may include administering a sensory processing disorder test, which helps identify any difficulties in processing sensory input. The occupational therapist will also review the individual's medical history and developmental background to rule out other conditions. While SPD is not formally recognized as a medical diagnosis in all diagnostic systems, when sensory processing difficulties significantly impact daily life, it can lead to a sensory processing disorder diagnosis. In children, SPD is often assessed alongside conditions like autism spectrum disorder, as the two can co-occur.
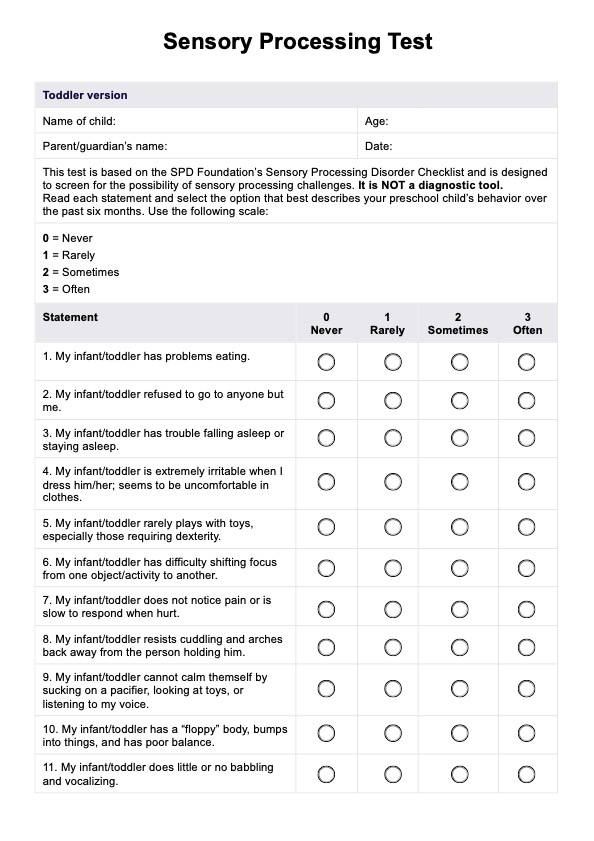
Sensory Processing Disorder Test
Learn how sensory processing disorder works. Download a free Sensory Processing Disorder Test for your clients.
Sensory Processing Disorder Test Template
Commonly asked questions
To assess for sensory processing disorder (SPD), healthcare professionals, particularly occupational therapists, use a variety of tools and assessments. This may include standardized sensory processing disorder tests to measure how an individual responds to different sensory inputs, such as touch, sound, or movement. Observations of behavior in different settings are also crucial, as well as interviews with parents, caregivers, or the individual themselves. Additionally, the occupational therapist will evaluate how sensory challenges impact everyday tasks and functioning.
Sensory processing disorder (SPD) can feel overwhelming, as individuals may experience heightened sensitivity or an underreaction to sensory stimuli. For example, someone with SPD may feel intense discomfort or anxiety from certain textures, sounds, or lights that others may find neutral. This sensory overload can lead to irritability, restlessness, and difficulty focusing. Individuals may also avoid certain situations or environments, such as crowded spaces or loud noises, due to the overwhelming sensory input. In children with SPD, these sensory challenges can affect emotional regulation and lead to behavioral issues, sometimes making it difficult to distinguish from conditions like autism spectrum disorder.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











