Rheumatoid arthritis (RA) is an autoimmune disorder where the immune system mistakenly attacks the body's joints, causing inflammation, pain, and potential joint damage.
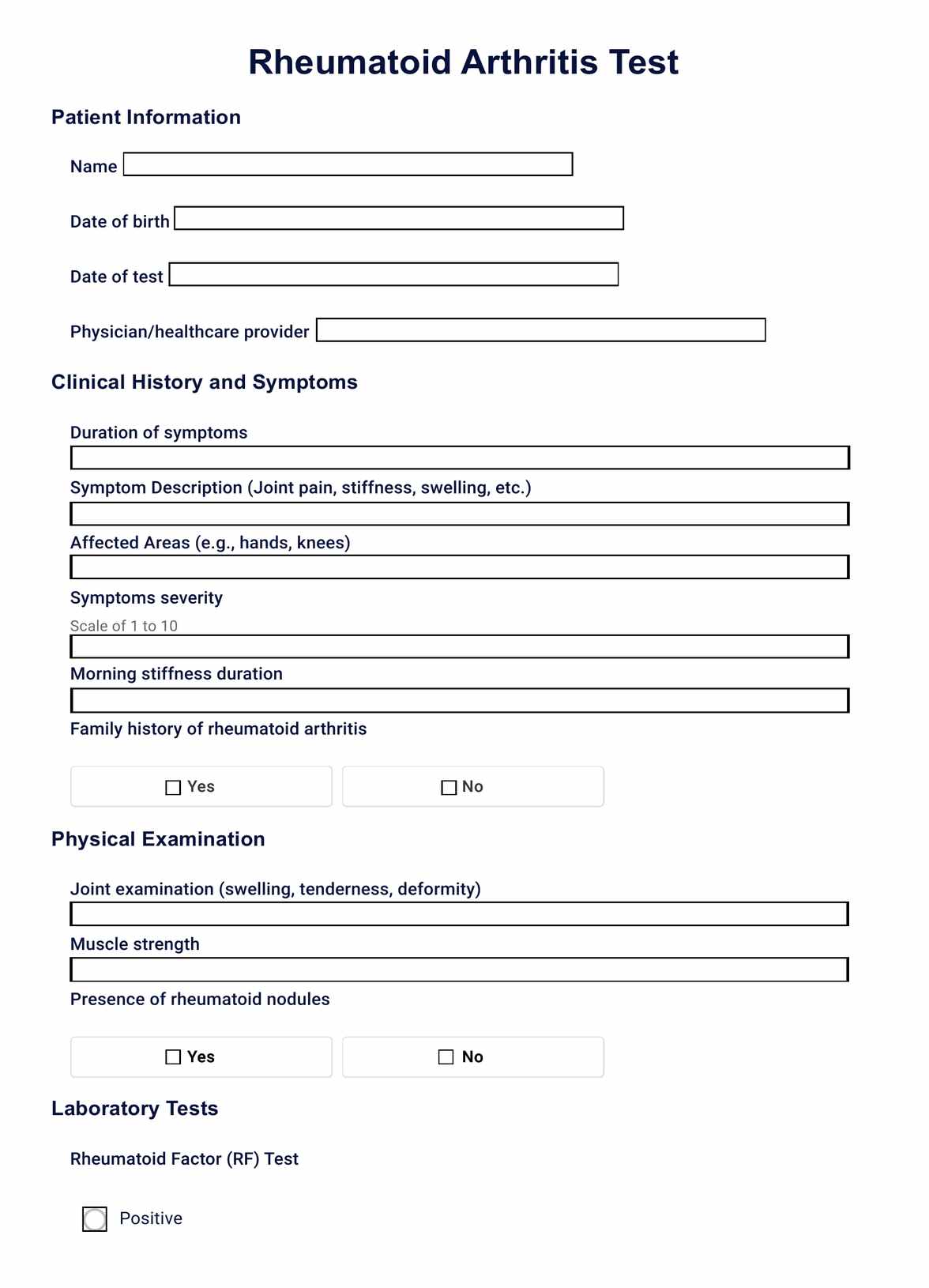
Rheumatoid Arthritis Test
Explore our comprehensive guide on Rheumatoid Arthritis testing, including diagnosis methods, blood and imaging tests, and treatment strategies.
Use Template
Rheumatoid Arthritis Test Template
Commonly asked questions
RA is diagnosed through a combination of physical examinations, patient history, blood tests (like rheumatoid factor and anti-CCP), and imaging tests such as X-rays, MRI, or ultrasound.
Common blood tests include the rheumatoid factor (RF) test, anti-cyclic citrullinated peptide (anti-CCP) test, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) test.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











