Pressure Ulcer Nursing Care Plan
Use this guide to create pressure ulcer and injury nursing care plans to deliver superior care and prevention.


What is a Pressure Ulcer Nursing Care Plan template?
A Pressure Ulcer Nursing Care Plan is a structured guide used by healthcare professionals to assess, diagnose, and manage the care of individuals at risk for or suffering from pressure ulcers. This care plan aims to prevent pressure ulcers and ensure appropriate treatment for existing ulcers, promoting healing and preventing complications such as infection.
Pressure injuries, also referred to as bedsores or pressure ulcers, represent a prevalent issue within the healthcare sector. They occur due to prolonged pressure on a specific skin area without relief. The National Pressure Injury Advisory Panel (NPIAP) defines a pressure injury as localized skin and underlying tissue damage, typically occurring over a bony prominence or associated with medical or other devices (2019). Individuals who are bedridden, use wheelchairs, or have limited mobility are at greater risk of pressure ulcer development. Pressure ulcers can cause intolerable levels of pain and discomfort for the patient and may lead to infection, sepsis, and potentially fatal outcomes.
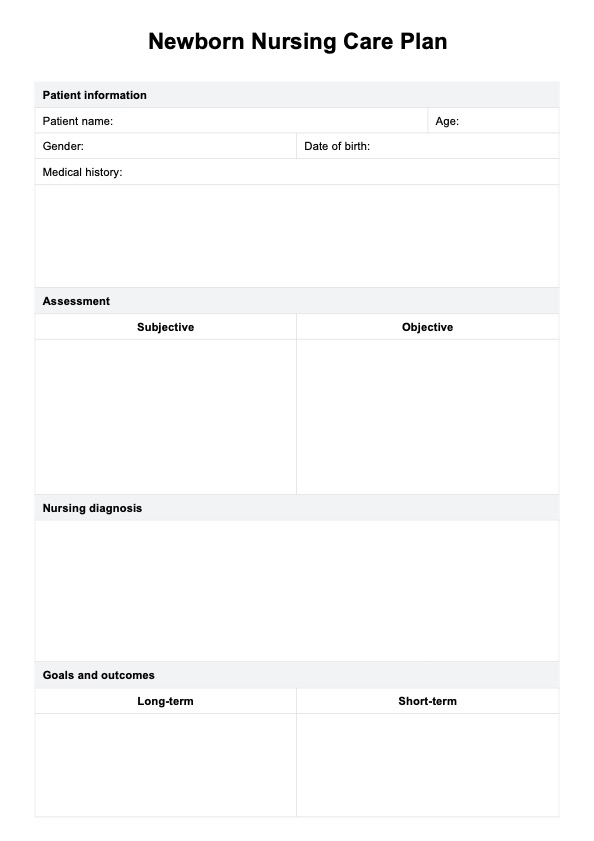
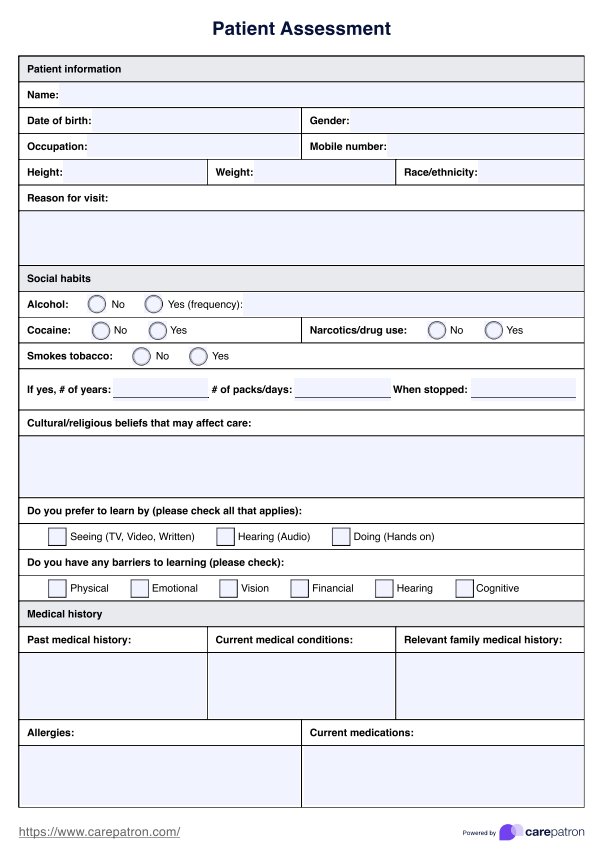
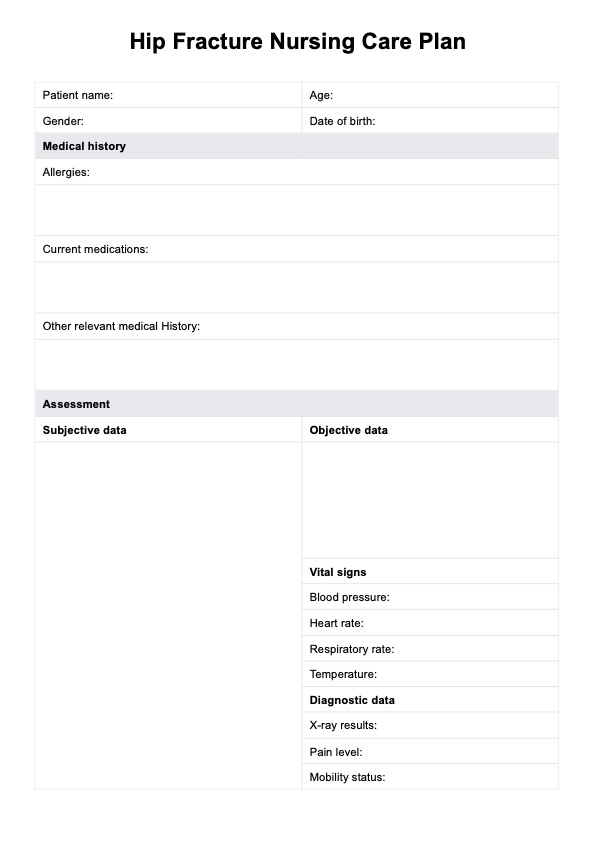
The plan includes detailed information about the patient's medical history, skin assessments, diagnosis of pressure injuries, goals (both short- and long-term), nursing interventions, rationales, and evaluation. It helps healthcare professionals create personalized care strategies that address the unique needs of each patient, ensuring comprehensive care and recovery.
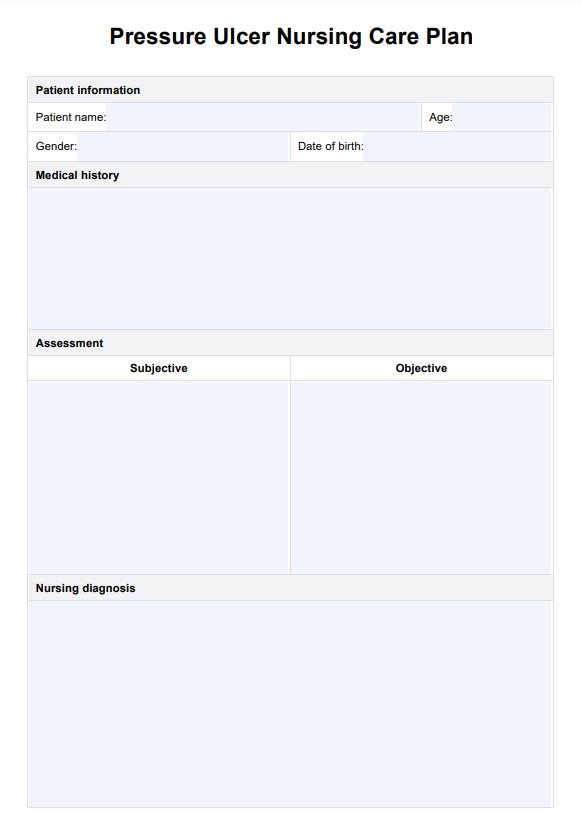
Pressure Ulcer Nursing Care Plan Template
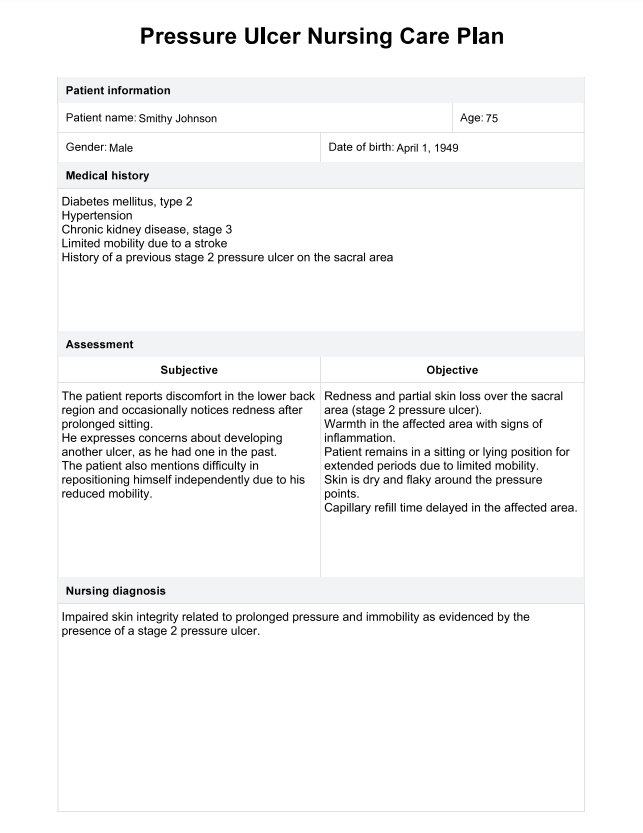
Pressure Ulcer Nursing Care Plan Example
How to use our Pressure Ulcer Nursing Care Plan template
This Pressure Ulcer Nursing Care Plan template provides healthcare professionals with organized fields for documenting patient care and progress, ensuring that care plans are tailored to individual needs. Here’s a step-by-step guide on how to use the template:
Step 1: Access the template
To begin, click the “Use template” button to open the template in the Carepatron app, where you can customize it according to your organizational requirements or write in additional sections or branding. Alternatively, click the “Download” button to save a PDF copy that can be printed and filled out manually.
Step 2: Assess the patient
Perform a thorough pressure ulcer risk assessment by evaluating the patient’s medical history, skin condition, and any other factors contributing to pressure injuries. Use the NPIAP staging system to categorize any existing pressure ulcers and record these details in the "Assessment" section.
Step 3: Establish a nursing diagnosis
Formulate a nursing diagnosis based on the patient’s risk factors and current condition. Document this diagnosis in the designated section, taking into account impaired skin integrity, risk for infection, and risk for impaired peripheral tissue perfusion.
Step 4: Set goals and outcomes
Outline the short-term and long-term goals for the patient’s recovery. Goals should focus on preventing further tissue damage, promoting healing, and improving mobility. For example, you might aim for the wound to show signs of healing within two weeks, or for the patient to maintain adequate nutrition and hydration to support skin integrity.
Step 5: Implement nursing interventions
Develop and document nursing interventions that focus on relieving pressure, improving circulation, and ensuring proper wound care. Use interventions such as frequent repositioning, applying Negative Pressure Wound Therapy (NPWT), providing skin care, and managing nutrition. Explain these interventions to the patient and their caregivers, ensuring that they understand the importance of these actions in their recovery.
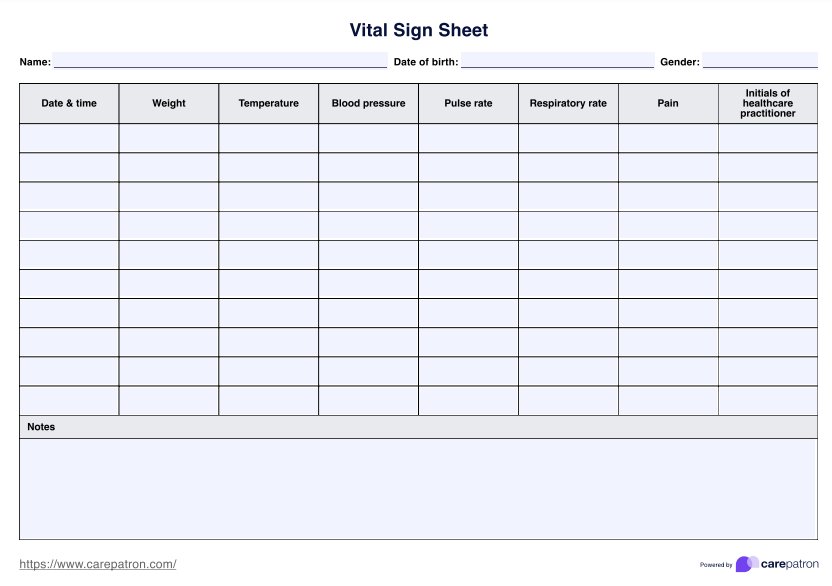
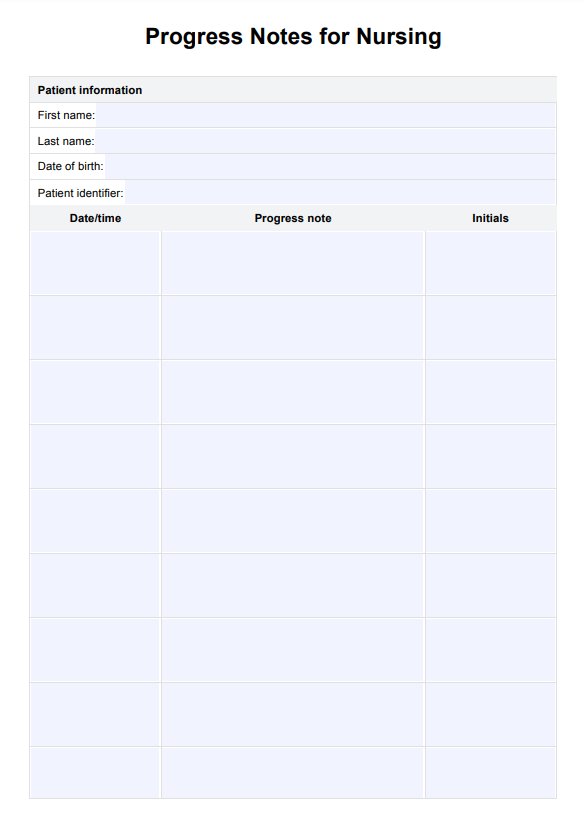
Step 6: Evaluate and adjust care plan
Continuously evaluate the patient’s progress through regular assessments and document the results in the “Evaluation” section. If necessary, adjust the care plan based on the patient’s response to treatment, healing progress, and overall health condition.
What you need to know about pressure ulcers
A pressure injury manifests as localized skin damage where tissues experience compression between bony areas and firm surfaces like a mattress. These injuries result from pressure and friction, shearing forces, and moisture. The applied pressure constricts small blood vessels, leading to compromised tissue circulation, and this decrease in blood flow induces tissue hypoxia, eventually causing cell death.
While terms like decubitus ulcer, pressure sore, and pressure ulcer have traditionally been used interchangeably, the NPIAP has recommended "pressure injury" as the preferred term since open ulceration doesn't always occur. These injuries can appear as unbroken skin or an open sore, causing discomfort (Kirman & Geibel, 2022).
A pressure injury is often defined within healthcare settings in the following system:
- Stage 1 pressure injury: Nonblanchable erythema of intact skin
- Discoloration of the skin that doesn't turn white when pressed
- Stage 2 pressure injury: Partial-thickness skin loss with exposed dermis
- Stage 3 pressure injury: Full-thickness skin loss
- Stage 4 pressure injury: Full-thickness skin and tissue loss
Apart from these stages, there are two more categories:
- Unstageable pressure injury: Obscured full-thickness skin and tissue loss
- Deep pressure injury: Persistent non-blanchable deep red, maroon, or purple discoloration
The weight of an individual against a surface applies pressure to the skin, soft tissue, muscles, and bones, often surpassing the capillary filling pressure of 32 mm Hg. Pressure injuries are prevalent among patients in both acute and chronic care settings. Estimates suggest that around one million pressure injuries occur in the United States. Older adults admitted to acute care hospitals for non-elective orthopedic procedures face an elevated risk of these injuries compared to other hospitalized patients. Annually, approximately 60,000 individuals die from complications arising from pressure injuries (Kirman & Geibel, 2022).
Pressure ulcer nursing diagnoses
While pressure injuries can be identified and categorized through the stages outlined above, further nursing intervention is required past the assessment point. Early detection and action taken on signs of tissue damage through regular and routine assessment, nutritional intervention, skin care product use, and decreasing the time of tissue exposure to pressure through regular position changes and relief means, such as dressings and props, are all key aspects of pressure ulcer nursing care plans.
Impaired skin integrity
Pressure injuries represent localized soft tissue damage commonly observed in older adults, individuals with restricted mobility, those confined to beds or chairs, post-injury or surgery, and clients with compromised nutrition. These conditions reduce the skin and underlying tissue's ability to withstand forces that can harm them, leading to potential damage to the skin and circulation if pressure, friction, or shear persists. The instigation of this nursing care plan will be evidenced by skin lesions and ulcers and redness on bony prominences. Goals of care for this plan may include the expectation of the client to be free of or display improvement in wound and tissue healing, and instigate and follow through with techniques that prevent skin breakdown and promote healing. To reach these goals of care, intervention may include:
- Inspecting the patient's skin routinely.
- Focusing on common pressure points during skin assessment.
- Assessing for the presence of medical devices that could cause pressure.
- Assessing the skin for signs of possible tissue damage.
- Determining the stage of the pressure injury.
- Assessing nutritional status and initiating corrective measures, as indicated.
- Encouraging adequate fluid intake.
- Maintaining strict skincare and hygiene.
- Changing position frequently in the chair and bed.
Risk for infection
Inadequate treatment or complications, such as infections, can hinder the healing process of pressure injuries. The application of unsuitable therapies corresponding to the ulcer's stage can lead to treatment delays in patients experiencing worsening tissue damage. While pressure injuries are frequently observed, interdisciplinary management and implementing essential preventive and therapeutic strategies can mitigate these injuries and their associated complications. The goals of care for the patient should lead to them being free of infection, achieving timely wound healing, a good level of education and understanding around the patient exposure and risk factors, and knowledge and instigation of measures that prevent or reduce future infection risk. To reach these goals of care, nursing intervention may include:
- Assessment of signs and symptoms of systemic infection. Monitor temperature routinely.
- Observation of the wound, noting the presence of drainage and inflammation.
- Recording risk factors for the occurrence of infection.
- Instruct the client or family members in techniques to prevent the spread of infection.
Risk for impaired peripheral tissue perfusion
Applying pressure to soft tissue exceeding the pressure levels in the blood vessels supplying that area can lead to ischemia and swelling (edema), ultimately resulting in pressure injuries. The skin tends to withstand pressure better than muscle, occasionally masking more profound tissue damage. Prolonged pressure, approximately double the closing pressure of capillaries, maintained for 2 hours, causes irreversible ischemic harm to the tissue (Ricci et al., 2017). The instigation of this care plan is of value for people with impaired mobility, under anesthesia, or who suffer from advanced dementia, whereby sensation detection may not be present. The patient's care goals are met when there is sufficient tissue perfusion and no signs of edema or necrotic tissue formations. Meeting these goals of care can be done through the following interventions:
- Assessing for the presence of peripheral vascular/arterial diseases.
- Monitoring the client's blood glucose levels routinely. Assess for peripheral neuropathy.
- Monitoring the client's vital signs.
- Repositioning or turning the patient every 2 hours.
- Utilization of special support surfaces for pressure reduction such as foam, air, or gel-filled mattress overlays.
When to use the Pressure Ulcers Nursing Care Plan Template
A pressure ulcer nursing care plan is typically employed when a patient has or is at risk of developing pressure ulcers. These care plans are crucial in various scenarios:
Existing pressure ulcers
When a patient already has pressure ulcers, a care plan is devised to manage and treat the existing wounds. It includes strategies for wound care, infection prevention, pain management, and promoting healing.
Prevention
For individuals at risk of pressure injury development due to immobility, limited sensation, or other factors, a preventive care plan is essential. This plan focuses on reducing pressure, such as repositioning schedules, using specialized cushions or support surfaces, maintaining skin integrity, and ensuring proper nutrition and hydration.
Hospitalized patients
In healthcare facilities, especially hospitals and long-term care settings, care plans are used to monitor and prevent pressure ulcers in patients with limited mobility or extended bed rest. Nurses and healthcare professionals follow these plans to prevent the occurrence of ulcers during hospital stays.
Home care settings
Patients receiving care at home, particularly those with limited mobility or chronic conditions, benefit from pressure ulcer care plans. These plans help caregivers and family members understand preventive measures and wound care techniques to manage and prevent ulcers.
The care plan's primary goal is to prevent the development of pressure ulcers or manage existing ones effectively, ensuring the patient's comfort, promoting healing, and reducing the risk of complications. Nurses and healthcare professionals tailor these plans to individual patient needs and regularly assess and adjust them based on the patient's condition and response to treatment.
References
European Pressure Ulcer Advisory Panel, National Pressure Injury Advisory Panel, & Pan Pacific Pressure Injury Alliance. (2019). Prevention and Treatment of Pressure Ulcers/Injuries: Clinical Practice Guideline. EPUAP/NPIAP/PPPIA.
Kirman, C. N., & Geibel, J. (2022). Pressure Injuries (Pressure Ulcers) and Wound Care: Practice Essentials, Background, Anatomy. EMedicine. https://emedicine.medscape.com/article/190115-overview#a5
Ricci, J. A., Bayer, L. R., & Orgill, D. P. (2017). Evidence-Based Medicine: The Evaluation and Treatment of Pressure Injuries. Plastic and Reconstructive Surgery, 139(1), 275e286e. https://doi.org/10.1097/prs.0000000000002850
Commonly asked questions
The primary nursing goals for bed sores are to promote wound healing, prevent further skin breakdown, relieve pain, and educate the patient on preventive measures. These goals focus on maintaining skin integrity and minimizing the risk of infection.
Nursing interventions for a pressure ulcer include repositioning the patient every two hours, using specialized support surfaces (e.g., foam or air-filled mattresses), ensuring proper nutrition and hydration, providing negative pressure wound therapy for advanced ulcers, and maintaining strict hygiene practices to prevent infection.
Nursing management can prevent developing pressure injuries by conducting regular skin assessments, repositioning patients frequently to relieve pressure, maintaining proper hygiene, using pressure-relieving devices, and ensuring adequate nutrition and hydration to support skin health.