Prediabetes Treatment Guidelines
Learn more about prediabetes in this guide. Access free Prediabetes Treatment Guidelines for better patient education.


What is prediabetes?
Prediabetes is a significant health concern characterized by elevated blood sugar levels. A person with prediabetes will present with an average blood glucose above normal ranges but below the threshold for a type 2 diabetes diagnosis. This condition represents an increased risk of developing type 2 diabetes and heightened susceptibility to heart disease and stroke.
Timely detection and treatment of prediabetes is crucial in preventing diabetes, though more than 80% of individuals with prediabetes are unaware of their condition (Centers for Disease Control and Prevention, 2021). Detecting prediabetes and implementing appropriate treatment strategies and lifestyle changes can significantly improve health outcomes.
Effective management of prediabetes significantly reduces the risk of developing type 2 diabetes and its associated complications. Additionally, people with prediabetes should present to their physician for regular diabetes screening. Utilizing evidence-based treatment strategies for prediabetes helps to prevent disease progression and improve holistic well-being.
Prediabetes Treatment Guidelines Template
Prediabetes Treatment Guidelines Example
Causes, diagnosis, and outcomes of prediabetes
The pathology of prediabetes involves two interrelated mechanisms: insulin resistance and impaired glucose tolerance. Insulin resistance occurs when cells become less responsive to insulin, hindering glucose uptake. Impaired glucose tolerance refers to diminished glucose processing, resulting in prolonged periods of elevated blood sugar after meals.
Risk factors for these types of physiological dysfunction include genetic predisposition, sedentary lifestyles, excessive calorie consumption, and obesity or high body mass index. Dietary habits have a significant influence, with diets high in refined carbohydrates, sugars, and saturated fats increasing the risk of prediabetes.
Additional risk factors include hormonal imbalances, age-related changes in metabolism and lifestyle habits, certain medications, and underlying health conditions (such as polycystic ovary syndrome (PCOS), gestational diabetes, and metabolic syndrome) that may exacerbate these mechanisms, further predisposing individuals to prediabetes.
Treatment strategies attempt to combat these factors to restore metabolic functioning and prevent disease progression. Type 2 diabetes involves chronic hyperglycemia, placing patients at heightened risk of microvascular and macrovascular complications, as well as cardiovascular disease (e.g., coronary artery disease, myocardial infarction, and peripheral vascular disease.
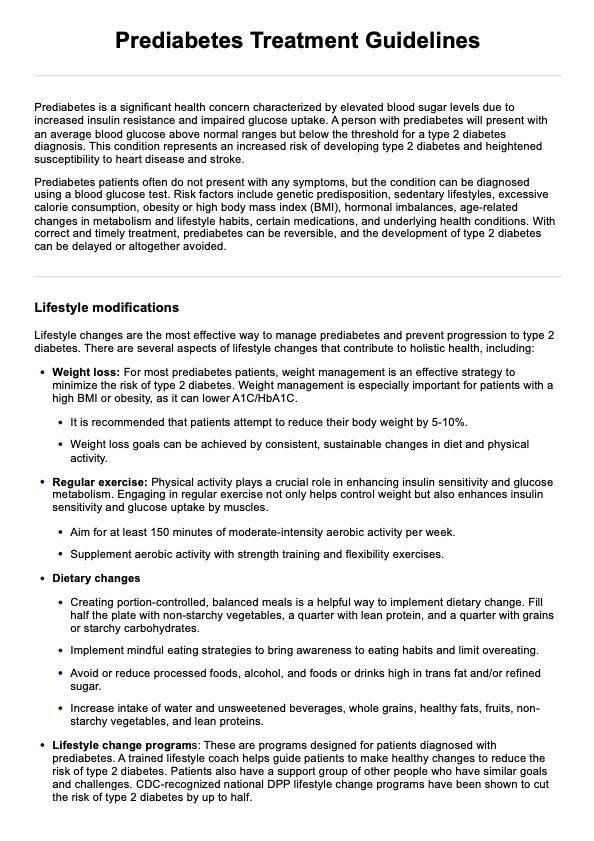
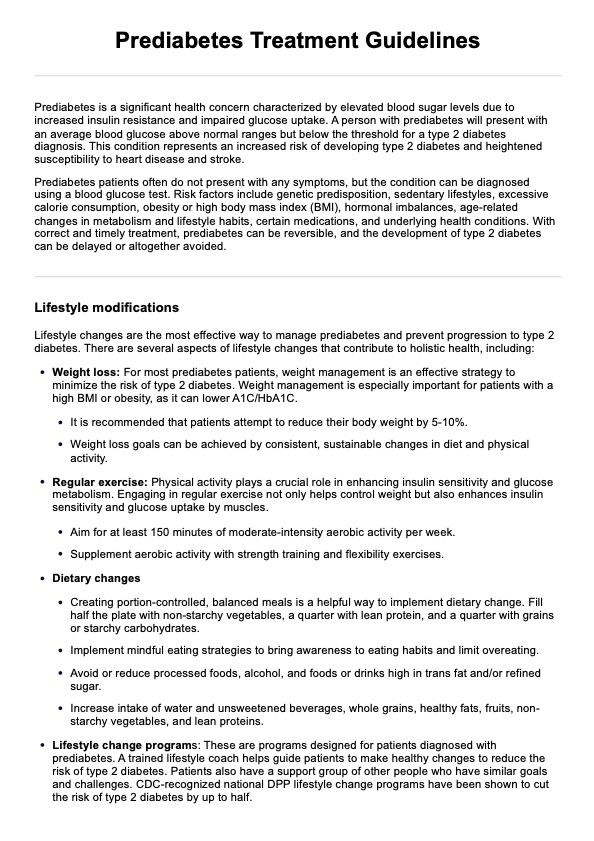
Prediabetes Treatment Guidelines
There are a variety of effective treatment approaches and lifestyle modifications available for prediabetes management. Our comprehensive Prediabetes Treatment Guidelines are designed to support healthcare providers in communicating these strategies to their patients. Here's an overview of each intervention:
Dietary changes
A balanced and nutritious diet is central to prediabetes management. Prioritizing whole foods such as fruits, vegetables, whole grains, and lean proteins promotes stable blood sugar levels and supports overall health. Reducing the intake of refined carbohydrates and processed or sugary foods and beverages is essential in preventing blood glucose spikes.
Regular exercise
Physical activity plays a crucial role in enhancing insulin sensitivity and glucose metabolism. Regular exercise not only helps control weight but also enhances insulin sensitivity and glucose uptake by muscles. Aim for at least 150 minutes of moderate-intensity aerobic activity per week, supplemented with strength training and flexibility exercises.
Weight management
Weight loss is a cornerstone of prediabetes management for individuals who are overweight or obese. A 5-10% weight loss can significantly improve insulin sensitivity and metabolic parameters. Sustainable portion control, mindful eating, and regular physical activity can facilitate gradual, healthy weight loss.
Medication
In some cases, medication therapy may be warranted to complement lifestyle modifications and reduce the risk of disease progression. Metformin is commonly prescribed to improve insulin sensitivity and glucose tolerance.
Monitoring and follow-up
Regular monitoring and follow-up are essential components of prediabetes management to assess treatment efficacy and ensure adherence to therapeutic interventions. Monitoring blood glucose levels regularly allows for timely adjustments to treatment plans and helps track progress toward glycemic targets.
How does the template work?
Our Prediabetes Treatment Guidelines template provides a structured framework for documenting prediabetes treatment plans. Here's a step-by-step guide:
Step 1: Access the template
Access the Prediabetes Treatment Guidelines by clicking the "Use template" button in the Carepatron app or by searching for it in Carepatron's free template library.
Step 2: Make treatment recommendations
Refer to the template to outline the recommended treatments for the patient. To promote compliance, ensure they have adequate education about why each has been recommended.
Step 3: Create a treatment strategy
Work with the patient to create a comprehensive treatment strategy encompassing each intervention in the guideline that is relevant to them. It is helpful to provide the patient with a copy of the Prediabetes Treatment Guidelines handout they can reference throughout the treatment process.
Step 6: Monitoring and follow-up
Schedule follow-up assessments to monitor treatment progress. This may involve regular blood glucose monitoring, periodic reassessment of treatment goals, and adjustments to the treatment plan as needed.
Reference
Centers for Disease Control and Prevention (2021, December 21). Prediabetes - Your chance to prevent Type 2 diabetes. https://www.cdc.gov/diabetes/basics/prediabetes.html#:~:text=What%20Is%20Prediabetes%3F
Commonly asked questions
While lifestyle modifications are the cornerstone of prediabetes management, medication such as metformin may be prescribed for individuals at high risk of developing type 2 diabetes mellitus.
The first line of treatment for prediabetes involves lifestyle modifications, such as dietary changes, regular exercise, and reducing body weight to improve insulin sensitivity and prevent disease progression. The American Diabetes Association provides nutrition guidelines for preventing and managing diabetes.
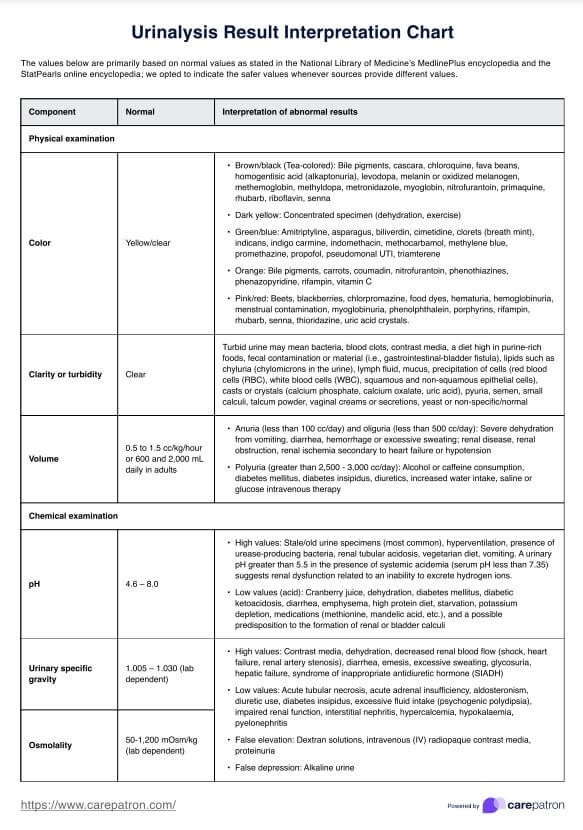
Diabetes diagnosis typically involves measuring blood glucose levels (such as blood glucose tests, A1C tests, or oral glucose tolerance tests) to determine if they are outside normal ranges. For example, a fasting plasma glucose level of 100-125 mg/dl typically indicates prediabetes.