PCOS Blood Test
Explore comprehensive blood tests for diagnosing Polycystic Ovary Syndrome (PCOS). Revise the essential tests to confirm PCOS and rule out other disorders.


Polycystic ovary syndrome: an introduction
Polycystic ovary syndrome (PCOS) is a hormonal disorder common among women of reproductive age. Women with PCOS may have infrequent or prolonged menstrual periods or excess male hormone (androgen) levels. The ovaries may develop numerous small collections of fluid (follicles) and fail to release eggs regularly.
The exact cause of PCOS is unknown, but it's believed to involve a combination of genetic and environmental factors. Insulin resistance, where the body's cells do not respond typically to insulin, is frequently seen in PCOS. Excess insulin might increase androgen production, causing difficulty with ovulation.
Symptoms include irregular periods, polycystic ovaries (visible via ultrasound), and elevated androgen levels, which can manifest as excess facial and body hair (hirsutism), acne, and hair loss.
PCOS is associated with an increased risk of developing health problems in later life, such as type 2 diabetes, hypertension, heart disease, and endometrial cancer. While no cure exists, treatment focuses on managing individual symptoms and may include lifestyle changes, medication, and surgery.
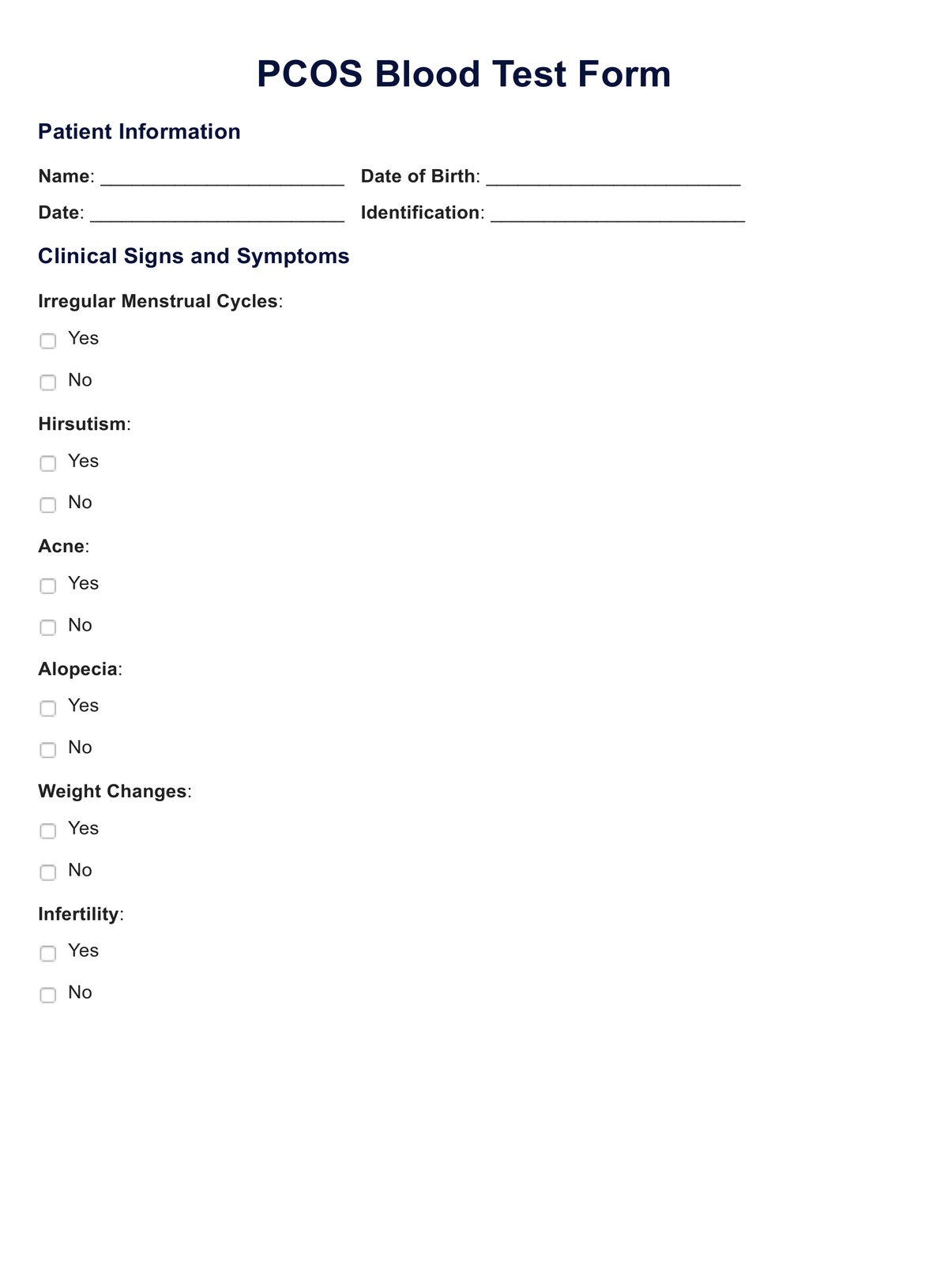
PCOS Blood Test Template
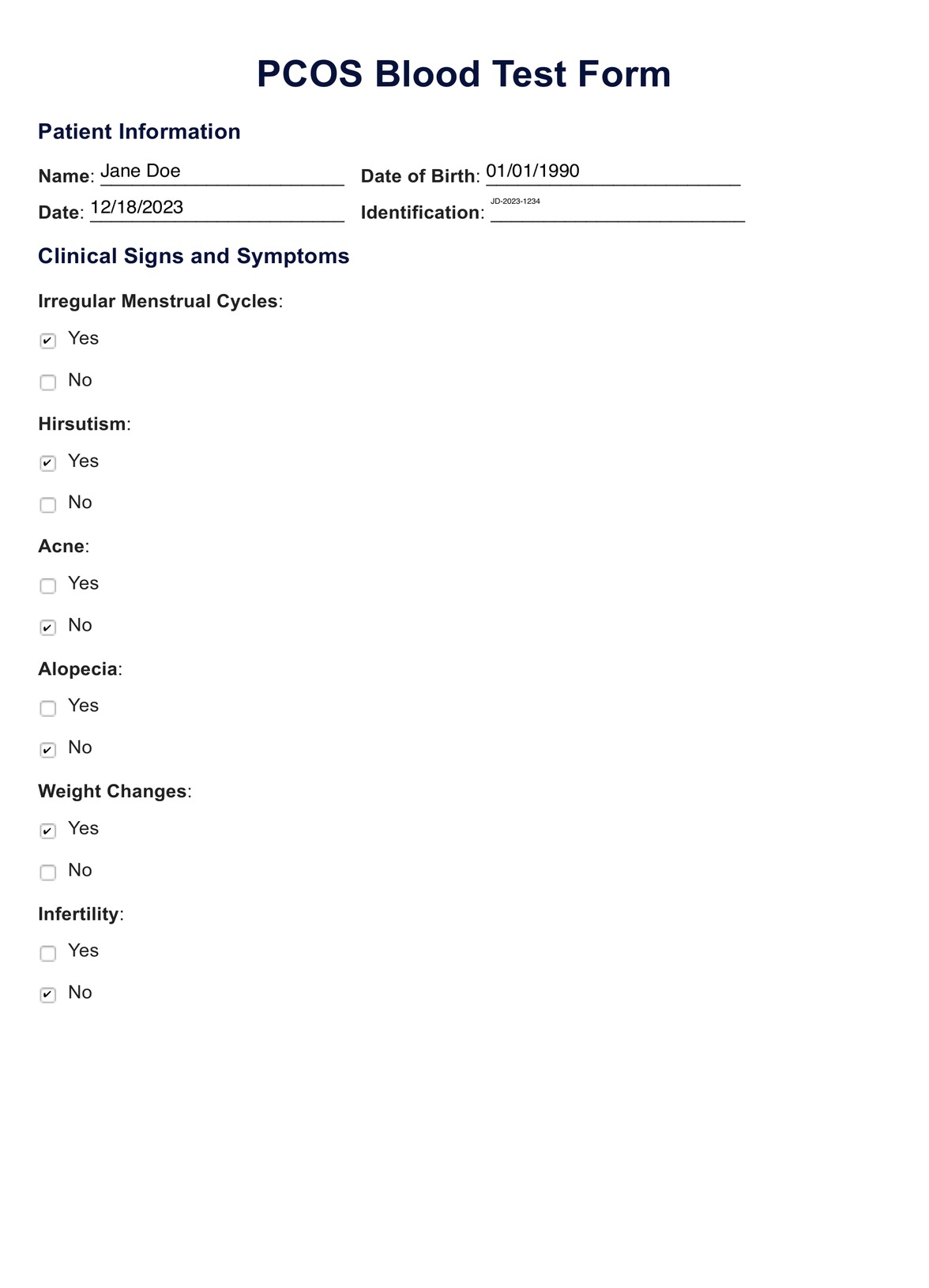
PCOS Blood Test Example
Diagnosing PCOS
Diagnosing Polycystic Ovary Syndrome (PCOS) can be a complex process, as there is no single test that definitively confirms the condition. Instead, healthcare providers use a variety of methods to diagnose PCOS, following the Rotterdam criteria, which require two of the following three findings:
- Irregular or absent menstrual cycles: This indicates anovulation or irregular ovulation, which can suggest PCOS when other conditions are ruled out.
- Clinical or biochemical signs of Hyperandrogenism: This may manifest as excess facial or body hair, severe acne, or male-pattern baldness. Biochemical signs involve elevated levels of androgens in the blood.
- Polycystic ovaries visible on ultrasound: The presence of numerous cyst-like structures around the edge of the ovaries.
The diagnosis process may include:
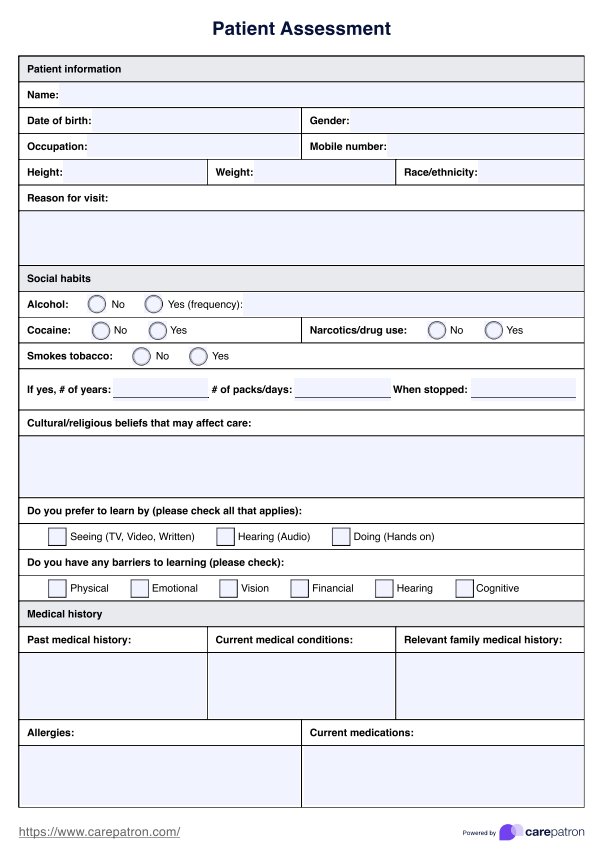
- Medical history review: A healthcare provider will look for symptoms such as menstrual irregularities, weight changes, acne, hair growth patterns, and fertility issues.
- Physical examination: This may include an assessment of signs of excess hair growth, acne, and other signs of androgen excess.
- Blood tests: These are used to check hormone levels, which can include luteinizing hormone (LH), follicle-stimulating hormone (FSH), total and free testosterone, sex hormone-binding globulin (SHBG), and others. Blood tests can also screen for insulin resistance and elevated cholesterol levels.
- Ultrasound: An ultrasound can visualize the ovaries to check for the presence of multiple cysts and evaluate the endometrium's thickness.
It is also important to exclude other conditions that can cause similar symptoms, such as thyroid disease, elevated prolactin levels, or non-classic congenital adrenal hyperplasia. This is typically done using additional blood tests.
Once other conditions are ruled out, and the criteria for PCOS are met, a diagnosis can be made. Treatment often focuses on symptom management, including lifestyle modifications and medications to regulate the menstrual cycle, manage metabolic concerns, and address any fertility issues. Regular monitoring and adjustments to the treatment plan are typically necessary to manage the condition effectively over time.
When are PCOS blood tests taken?
Blood tests for Polycystic Ovary Syndrome (PCOS) can be taken at any time, but there are specific considerations to keep in mind to ensure the accuracy of some hormone levels:
- Menstrual cycle timing: If a woman has regular menstrual cycles, it's often recommended to perform hormone tests in the early follicular phase, usually between days 2 and 5 of the menstrual cycle, as this is when baseline hormone levels like Follicle Stimulating Hormone (FSH) and Luteinizing Hormone (LH) can be most accurately assessed.
- Fasting state: Tests such as fasting glucose and fasting insulin levels are typically performed after an overnight fast.
- No requirement for timing: Some tests, like testosterone, sex hormone-binding globulin (SHBG), and thyroid function tests, may not require specific timing within the menstrual cycle and can be taken at any point.
- Special circumstances: For tests such as the 24-hour urinary-free cortisol or the dexamethasone suppression test, the healthcare provider will give specific instructions on when to take the test.
It's also important to note that if a woman does not have regular menstrual periods, which is common in PCOS, the timing of the blood tests can be more flexible. However, healthcare providers may still look for a window of opportunity when the hormone levels most likely reflect the woman's baseline state.
Ultimately, the timing for PCOS blood tests should be guided by a healthcare provider, who can offer the best advice based on the individual's symptoms and the specific tests being ordered. They may also advise avoiding certain activities or medications that could influence hormone levels before testing.
The steps of a PCOS blood test
1. Consultation with healthcare provider:
- Discuss symptoms and medical history.
- A physical examination may be conducted.
- A healthcare provider will determine which blood tests are needed.
2. Scheduling the test:
- Blood tests are scheduled according to the menstrual cycle if the patient has regular periods, usually during the early follicular phase (days 2-5).
- If periods are irregular or absent, the healthcare provider will advise on timing.
- Fasting tests are typically scheduled in the morning to facilitate overnight fasting.
3. Preparation for the test:
- Fasting for 8-12 hours may be required for specific tests such as glucose and lipid profiles.
- Avoiding exercise or stress before the test may be advised, as these can affect hormone levels.
- Patients may need to discontinue certain medications or supplements only after consulting with a healthcare provider.
4. During the test:
- A blood sample is drawn from a vein, usually in the arm.
- This process takes just a few minutes.
5. After the test:
- No special care is needed post-blood draw, but some people might need to rest briefly if they feel lightheaded.
- Resume normal activities and diet unless otherwise directed by the healthcare provider.
6. Receiving results:
- The blood samples are sent to a laboratory for analysis.
- Results may take a few days to weeks, depending on the tests.
7. Follow-up:
- Discuss results with the healthcare provider.
- If PCOS is confirmed, further discussion on treatment and management will follow.
- Additional tests or follow-ups may be scheduled to monitor the condition.
Throughout the process, the healthcare provider will provide specific instructions tailored to the individual's health status and the tests performed. It’s important to follow these instructions closely to ensure accurate test results.
Interpreting the results
The results of a PCOS blood test can indicate a variety of hormonal imbalances and metabolic issues commonly associated with the syndrome. Here's what might be found:
- Elevated androgen levels: High levels of androgens, such as testosterone, can be a sign of PCOS.
- Irregular insulin levels: Insulin resistance is common in PCOS, so fasting insulin levels may be higher than usual.
- Cholesterol and triglycerides: These might be elevated, indicating a risk of cardiovascular disease.
- LH to FSH ratio: A higher than average ratio may indicate PCOS.
- Elevated prolactin: This can be a sign of other health issues that mimic PCOS symptoms.
- Low SHBG: Sex hormone-binding globulin might be lower in women with PCOS.
- Anti-müllerian hormone (AMH): Levels may be higher in women with PCOS.
- An abnormal glucose tolerance test can indicate a predisposition to diabetes.
Next steps: How to manage PCOS
After receiving the results, the management of PCOS typically involves a combination of lifestyle changes, medication, and potentially surgery. Here’s what the management plan may include:
Lifestyle modifications:
- Weight management: Losing even a small amount of weight can help regulate the menstrual cycle and improve symptoms of PCOS.
- Diet: A balanced diet low in refined carbohydrates and fiber can help manage insulin levels.
- Exercise: Regular physical activity can help lower blood sugar levels and improve insulin resistance.
Medications:
- Hormonal birth control: To regulate menstrual cycles and reduce androgen levels.
- Metformin: To improve insulin resistance.
- Anti-androgens: To reduce unwanted hair growth and acne.
- Fertility medications: If pregnancy is desired, medications can help stimulate ovulation.
Monitoring:
- Regular check-ups to monitor symptoms and adjust treatment as necessary.
- Regular screening for complications such as diabetes, high cholesterol, and hypertension.
Specialist referral:
- Endocrinologists can offer specialized care for hormonal imbalances.
- Reproductive specialists can assist with fertility concerns.
- Dermatologists can help manage skin-related symptoms.
Surgical procedures:
- In some cases, a surgical procedure known as ovarian drilling is performed to induce ovulation.
Mental health support:
- Counseling or support groups for emotional support, as PCOS can affect mental well-being.
Alternative therapies:
- Acupuncture and herbal supplements have been explored, but discussing these with a healthcare provider before starting is important.
It is essential to tailor the management of PCOS to the individual's symptoms, life stage, and fertility goals. Regular follow-up with a healthcare provider is crucial for monitoring the condition and adjusting the treatment plan.
Commonly asked questions
In PCOS, male hormones (androgens) are often elevated. Blood tests measuring hormones like total testosterone can help diagnose PCOS. Normal androgen levels usually rule out PCOS, as higher-than-normal levels of these hormones characterize the condition.
A healthcare provider assesses clinical signs of PCOS during a physical exam, such as excess body hair, acne, and body mass index (BMI). They may also check blood pressure, as high blood pressure can be associated with PCOS. A pelvic ultrasound might look for enlarged ovaries or fluid-filled sacs (cysts).
Yes, birth control pills are commonly prescribed in PCOS to regulate menstrual cycles and lower levels of male hormones. They can help manage symptoms like acne and hirsutism and contribute to the normalization of the female reproductive system.