Osteoarthritis Treatment Guidelines
Learn about the management of osteoarthritis, treatments, causes, and care strategies. Access tips for managing symptoms and improving quality of life in our guide.


What is osteoarthritis?
Osteoarthritis (OA) is a progressive joint condition marked by the deterioration of cartilage, the resilient material that cushions the ends of bones in the joints. This degeneration results in joint pain, stiffness, and impaired mobility, often affecting the knees—including the patellofemoral region—hips and hands. As the condition advances, it can lead to symptomatic hip osteoarthritis and patellofemoral knee OA, significantly impacting daily activities and overall quality of life.
Osteoarthritis symptoms
Osteoarthritis, a prevalent form of arthritis, presents a range of symptoms that can progressively impact an individual's physical function and quality of life. The hallmark signs of this degenerative joint disease include:
- Morning joint-related stiffness: Individuals often experience stiffness in their joints after periods of inactivity, which is especially noticeable upon waking. This stiffness typically lasts for a short duration but can significantly affect the ability to perform morning routines comfortably.
- Activity-related joint pain: Engaging in activities or simple movements can exacerbate pain in the affected joints. This pain is directly related to joint use and tends to increase with activity intensity, often leading to a need for rest and relief measures.
- Reduced function and mobility: As osteoarthritis progresses, the wear and tear on joint cartilage can decrease joint mobility. This reduction in movement capability can hinder daily tasks, such as walking, climbing stairs, or opening jars, and may lead to avoiding activities once enjoyed.
- Swelling and tenderness: Affected joints may exhibit swelling due to inflammation, making them tender to the touch. This symptom can further limit movement and contribute to discomfort.
- Joint deformity: In advanced cases, the continuous degradation of joint structures can result in visible changes to the joint's appearance, often manifesting as knobby enlargements in the fingers or an altered knee joint shape.
- Crepitus: A common symptom in osteoarthritis patients is the sensation or sound of grating, popping, or cracking within the joint during movement. This phenomenon, known as crepitus, is due to the rough surfaces of the joints moving against each other.
- Reduced quality of life: Beyond the physical symptoms, osteoarthritis can lead to psychological and emotional distress. Chronic pain and reduced functionality can affect mental health, leading to feelings of frustration, depression, and anxiety, further exacerbating the disease's impact on well-being.
Addressing these symptoms through a comprehensive treatment plan is crucial for managing osteoarthritis. Early intervention, lifestyle modifications, and medical treatment can help slow the progression of the disease, alleviate pain, and improve overall quality of life.
Osteoarthritis causes and risk factors
Osteoarthritis (OA) emerges from a complex interplay of factors contributing to joint cartilage degeneration. The causes intertwine genetic predispositions, which influence susceptibility to OA, with metabolic and biochemical processes that can deteriorate joint health. Biomechanical factors, such as alignment and mechanical stress on joints, also play a critical role in the disease's development.
Risk factors further delineate the likelihood of developing OA, including aging, which naturally diminishes joint resilience and cartilage thickness. Obesity significantly increases the stress on weight-bearing joints, accelerating cartilage wear. History of joint injury or trauma, including sports injuries or accidents, can precipitate the onset of OA, as damaged joints are more susceptible to degeneration. Additionally, occupations or activities that involve repetitive joint use can exacerbate the wear and tear on cartilage, leading to OA.
Understanding these causes and risk factors is essential for early identification, preventive measures, and targeted treatment of osteoarthritis, aiming to mitigate its impact and preserve joint function and quality of life.
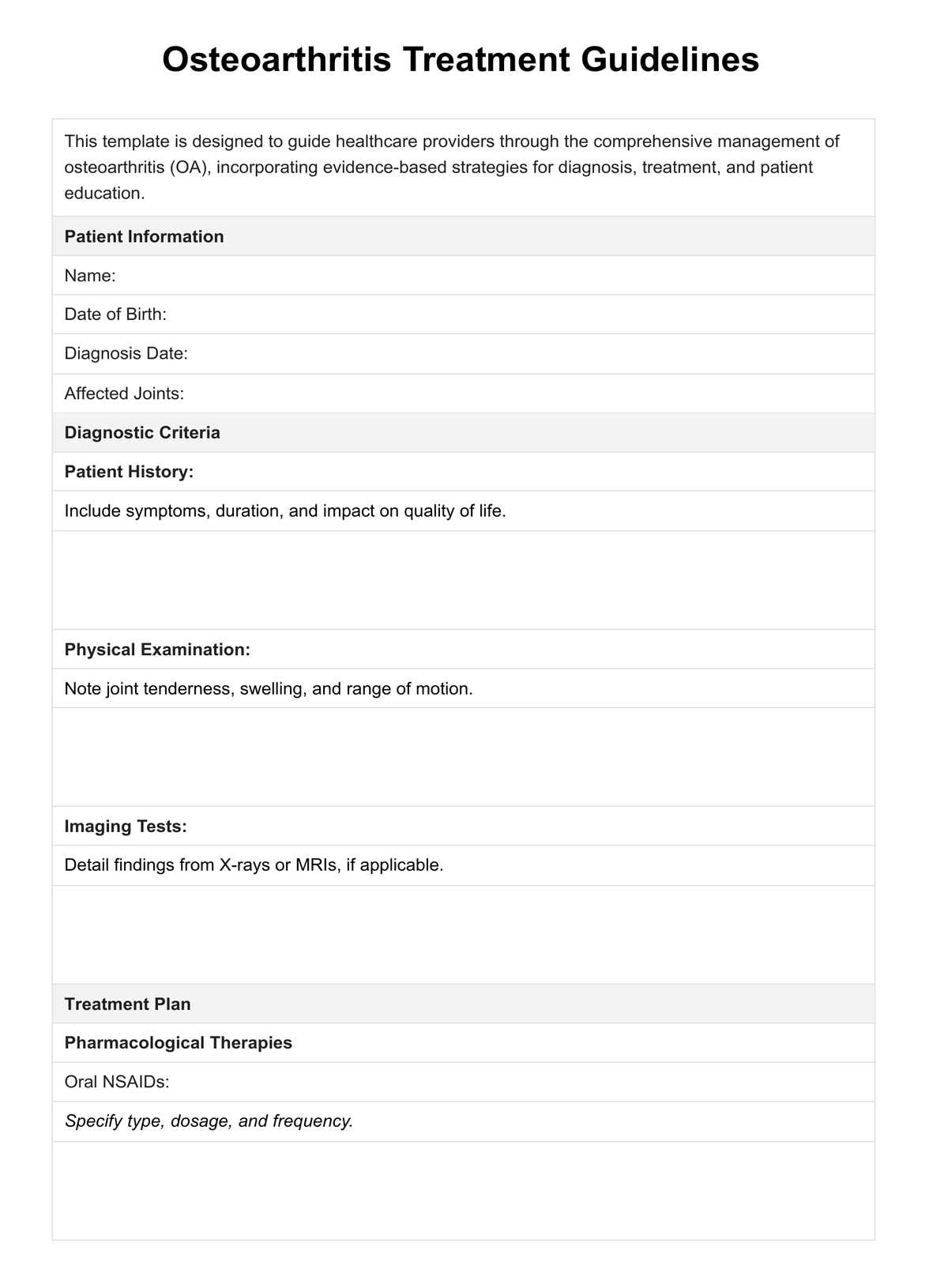
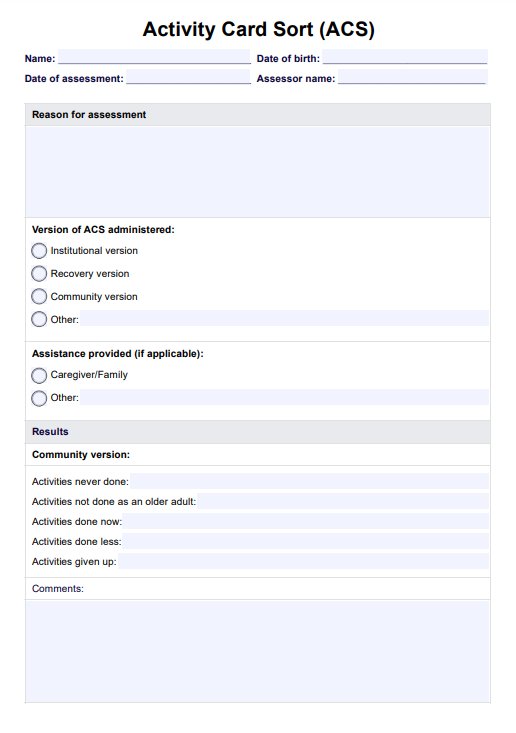
Osteoarthritis Treatment Guidelines Template
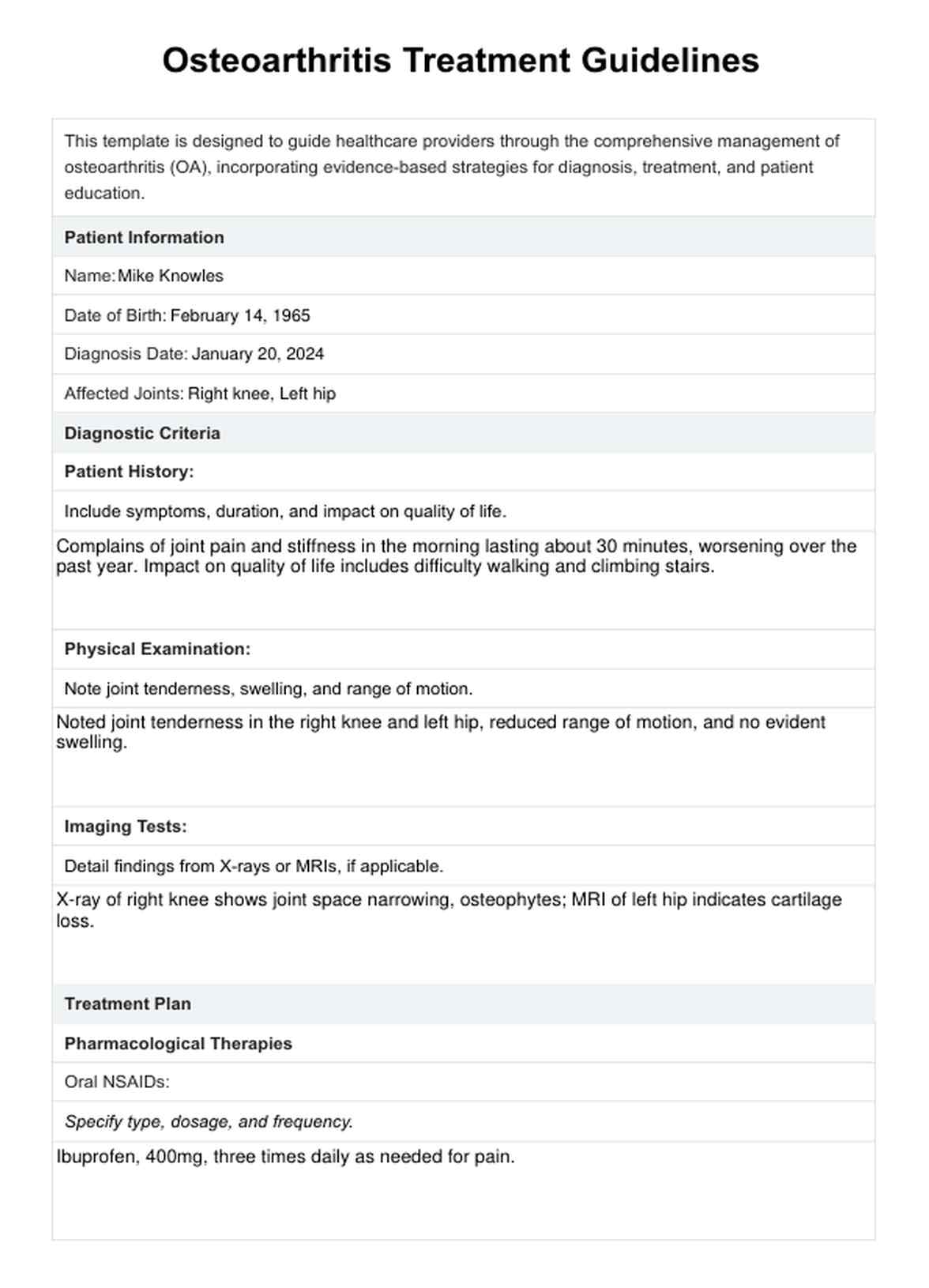
Osteoarthritis Treatment Guidelines Example
How do healthcare professionals diagnose osteoarthritis?
Healthcare professionals employ a multi-faceted approach to diagnose osteoarthritis, beginning with a detailed review of the patient's medical history and a physical examination to identify hallmark symptoms such as joint stiffness, pain, and reduced mobility. These initial steps are crucial for understanding the nature and extent of the condition.
Imaging tests like X-rays are commonly used to further evaluate the structural changes in the joints, revealing details such as cartilage loss, bone spurs, and joint space narrowing. Magnetic Resonance Imaging (MRI) may also be utilized in certain cases to provide more detailed images of both bone and soft tissues, offering insights into the severity of the disease not always visible on X-rays. This comprehensive diagnostic process enables healthcare providers to accurately identify osteoarthritis and tailor a treatment plan to the individual's needs.
Treatment guidelines
The clinical practice guidelines for managing osteoarthritis (OA) are centered around a holistic and integrated care approach tailored to patients' needs. These guidelines incorporate diagnostic strategies, treatment modalities, and patient education to ensure comprehensive care.
- Diagnostic protocols: Early and accurate diagnosis through patient history, physical examination, and imaging techniques like X-rays and MRIs. These methods help determine the severity and extent of joint damage.
- Integrating pharmacologic and non-pharmacologic treatments: A balanced approach combining pharmacologic treatments, like NSAIDs, with non-pharmacologic therapies, such as physical therapy and weight management, to address pain and mobility issues.
- Emphasis on self-management and education: Encouraging patient engagement in self-management programs enhances self-efficacy in managing OA symptoms and fosters a proactive approach toward health.
- Use of supportive therapies: Recommendations for supportive interventions, including knee braces and assistive devices, to alleviate pain and improve joint function.
- Personalization of care plans: Tailoring treatment plans to the individual's specific symptoms, lifestyle, and health status, emphasizing regular monitoring and adjustments based on patient response.
These guidelines are designed to be dynamic, evolving with new research and clinical insights. Healthcare providers are encouraged to utilize these guidelines in conjunction with their clinical judgment and patient preferences to optimize the management of OA.
How does our Osteoarthritis Treatment Guidelines template work?
Begin by downloading our Osteoarthritis Treatment Guidelines template to streamline the management and treatment of osteoarthritis. This resource is meticulously designed to incorporate a holistic approach to diagnosis and care tailored for healthcare professionals.
Step 1: Download our template
Secure immediate access to our comprehensive template, an invaluable roadmap for effectively addressing the management of knee osteoarthritis.
Step 2: Explore treatment recommendations
Within the template, you'll find an array of recommended treatments ranging from pharmacologic options, such as oral and topical NSAIDs, to non-pharmacologic strategies, including physical therapy and self-efficacy programs.
Step 3: Review diagnostic methods and tests
The template outlines essential diagnostic techniques and imaging tests, like X-rays and MRIs, which are vital for assessing joint damage and confirming an osteoarthritis diagnosis.
Step 4: Utilize ICD and CPT codes
Our template includes relevant ICD and CPT codes related to knee osteoarthritis for easy documentation and billing, ensuring accurate and efficient patient record management.
Step 5: Personalize with additional comments
Ample space is provided for adding notes, observations, or customizing treatment plans, allowing for a patient-centered approach to care.
By integrating these elements, our template simplifies the clinical process and enhances the quality of care for patients with knee OA or knee osteoarthritis.
Common treatments for osteoarthritis
The management of osteoarthritis involves a multifaceted approach tailored to alleviate pain, reduce inflammation, and enhance joint function. Here are some effective treatments commonly utilized:
- Topical and Oral Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): These topical and oral NSAIDs are cornerstone treatments for osteoarthritis, offering significant relief from pain and swelling by reducing inflammation within the affected joints.
- Topical capsaicin: Derived from chili peppers, capsaicin cream works by depleting the nerve cells of substance P, a chemical involved in conveying pain signals to the brain, thereby diminishing joint pain.
- Knee braces: Specially designed braces can provide valuable support to unstable joints, particularly in the knees, helping to evenly distribute weight away from the damaged parts of the joint, thus relieving pain and enhancing mobility.
- Self-management programs: These programs are crucial in educating patients about their condition, teaching them strategies for pain management, and promoting lifestyle modifications that can help manage symptoms and improve quality of life.
- Intra-articular corticosteroid injections: Administered directly into the joint space, these injections offer rapid relief from acute pain and inflammation, particularly during flare-ups of osteoarthritis.
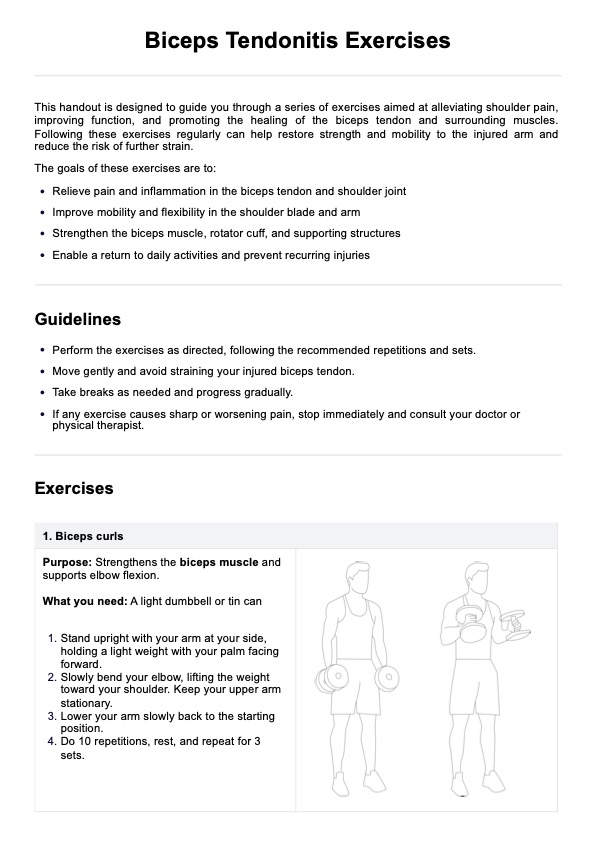
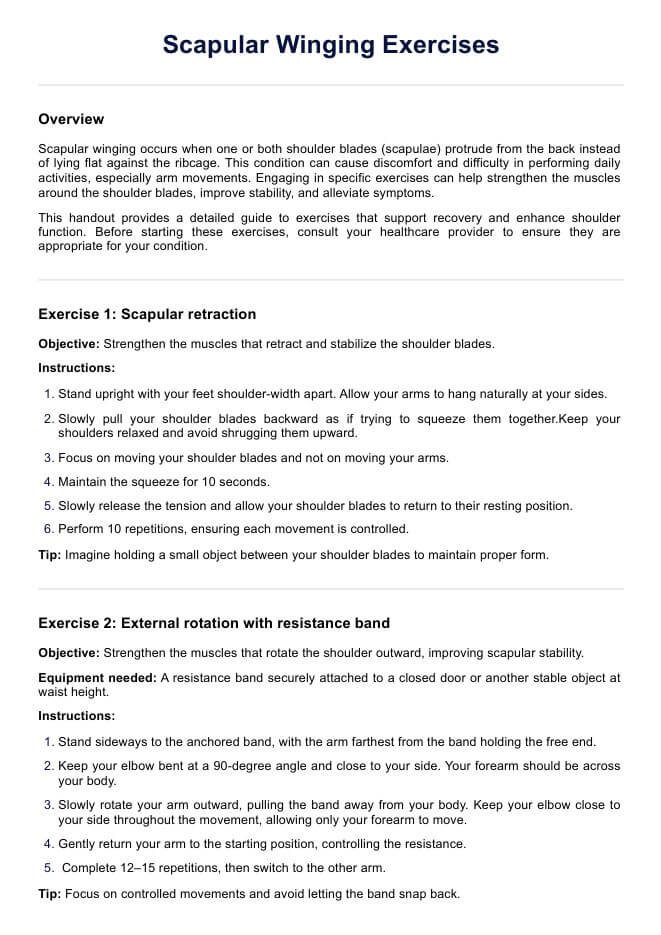
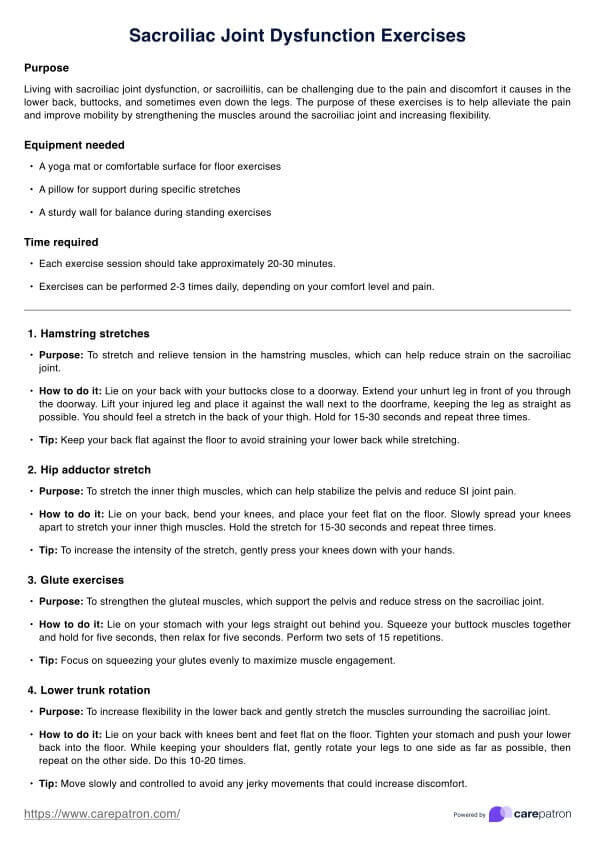
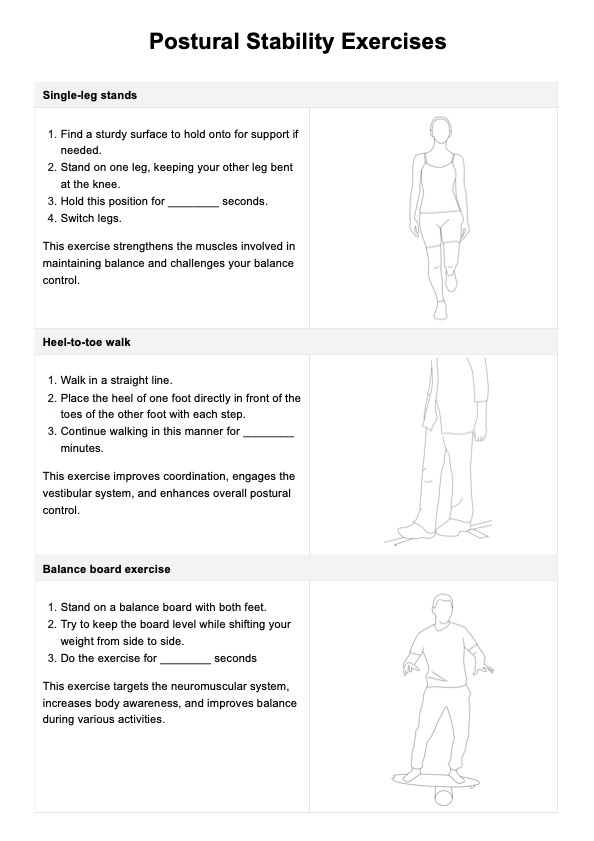
- Physical therapy: Tailored exercise programs designed by physical therapists can significantly improve joint strength, flexibility, and overall function while providing strategies to protect the joints during daily activities.
Together, these treatments form the backbone of osteoarthritis management, aiming not only to alleviate the immediate symptoms but also to maintain joint health and prevent further deterioration. Individuals with osteoarthritis need to work closely with their healthcare provider to determine the most appropriate treatment plan based on their specific needs and condition severity.
Commonly asked questions
Chronic stress can significantly worsen osteoarthritis symptoms, intensifying pain and diminishing physical functionality. Effective stress management techniques are crucial for enhancing individuals' overall well-being and life quality with OA.
A nutritious diet can play a pivotal role in managing osteoarthritis. Anti-inflammatory foods like fruits, vegetables, and omega-3-rich fish can help reduce joint inflammation and improve pain. Maintaining a healthy weight also reduces stress on the joints, alleviating symptoms.
While excessive or improper exercise can strain the joints, regular, moderate activity benefits OA patients. It strengthens the muscles around the joints, increases flexibility, and can help reduce pain and stiffness. Choosing low-impact exercises and consulting a healthcare provider for a personalized exercise plan is important.

.jpg)