Nursing Postpartum Assessment
Discover the importance of Postpartum Nursing Care and create effective assessments with our handy free guide!


The importance of postpartum nursing care
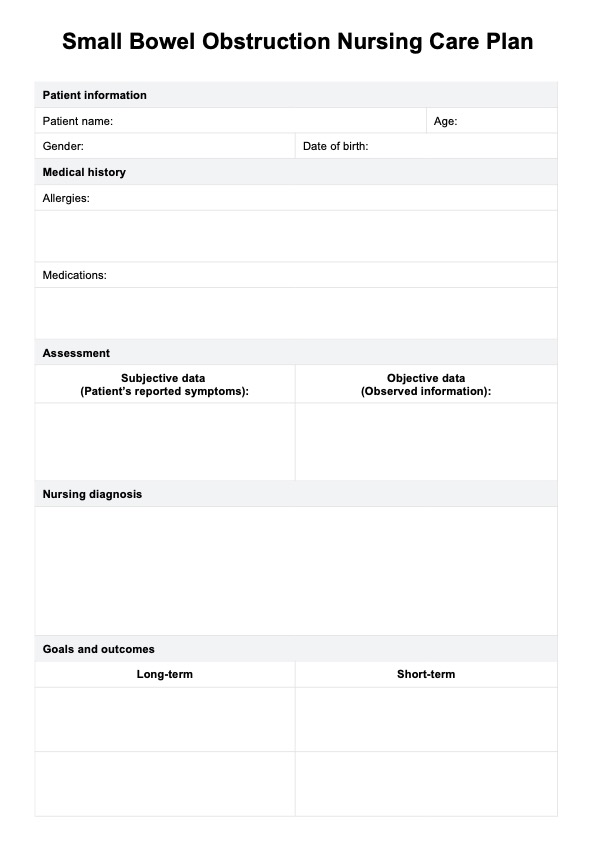
Postpartum nursing care is critical to ensuring the health and well-being of both the mother and the newborn after delivery. A thorough postpartum nurse assessment helps identify any immediate or long-term health concerns. The postpartum nursing assessment focuses on monitoring the mother’s physical recovery, especially after a vaginal birth, and assessing the emotional state of the postpartum women. Nurses perform a postpartum assessment of the mother, checking for abnormal findings like excessive blood flow or perineal pain, which could signal complications.
One vital component of this care is identifying and addressing mental health concerns, such as postpartum depression and postpartum blues, which can significantly affect a mother’s recovery. Early detection allows for further assessment and timely intervention. Additionally, postpartum patients are monitored for potential complications, such as deep vein thrombosis, which can arise from prolonged immobility.
During the postpartum examination, nurses may also check for signs of infection, sometimes recommending antibiotic therapy if needed. For patients recovering from a vaginal birth, proper attention to healing is crucial to prevent further complications. By providing comprehensive care, nurses help ensure that any abnormal findings are addressed quickly, promoting a smoother recovery for both mother and baby. The assessment is key to safeguarding long-term health and well-being during the postpartum period.
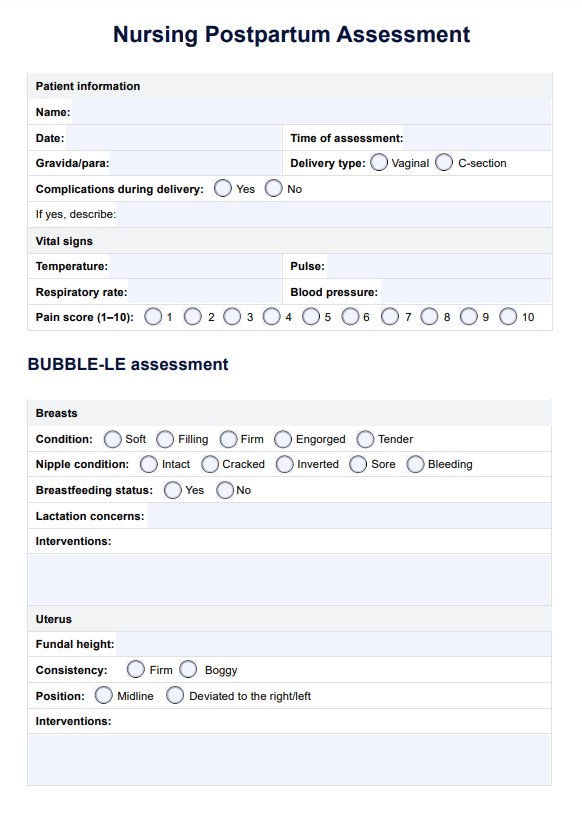
Nursing Postpartum Assessment Template
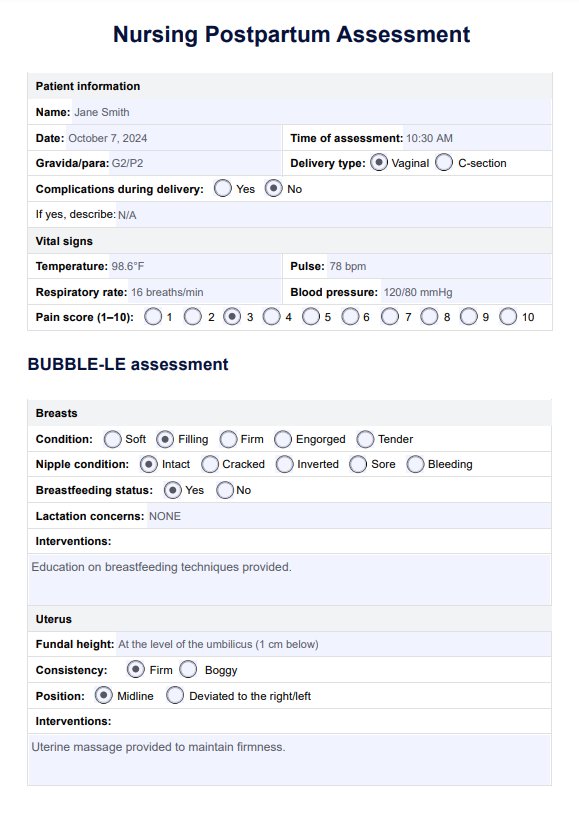
Nursing Postpartum Assessment Example
What is the BUBBLE-LE postpartum assessment?
The BUBBLE-LE assessment is a routine postpartum assessment done by healthcare professionals to evaluate the physical and emotional recovery of a woman after childbirth. This acronym stands for Breasts, Uterus, Bowel, Bladder, Lochia, Episiotomy (or perineum), Legs, and Emotional status, focusing on the primary areas of postpartum health that need to be monitored in the days and weeks after delivery. Here's what each component entails for a nursing postpartum assessment:
- Breasts: Assess for signs of engorgement, mastitis, or nipple soreness, especially in breastfeeding mothers, ensuring nipples are intact. Breasts should be soft and non-tender in the first few postpartum days, with some fullness as milk comes in but no intense pain. Encourage proper breastfeeding techniques or educate on managing engorgement for non-breastfeeding mothers.
- Uterus: Palpate the uterus to check for firmness and proper positioning, ensuring it is firm and descending into the pelvis each day. A firm, midline uterus is normal; a boggy uterus may indicate uterine atony, a risk for hemorrhage. If not firm, perform fundal massage and encourage early ambulation and breastfeeding to promote uterine contraction.
- Bowel: Assess bowel sounds, inquire about flatus and bowel movements, and check for constipation or hemorrhoids. Normal bowel sounds should be present, and the mother should pass gas and have a bowel movement within a few days postpartum. Encourage hydration, fiber-rich foods, and early ambulation, with stool softeners if necessary.
- Bladder: Evaluate voiding patterns, check for bladder distention or urinary retention, and inquire about discomfort during urination. The mother should void within 6-8 hours postpartum without retention or pain. Encourage frequent emptying of the bladder, and if the mother has difficulty voiding, catheterization may be required.
- Lochia: Monitor the color, amount, consistency, and odor of lochia, which should transition from red (rubra) to pink (serosa) to white (alba) over several weeks. Lochia should gradually decrease in amount; sudden increases or foul-smelling discharge are abnormal. Educate the mother to report excessive bleeding or large clots, which could indicate hemorrhage.
- Episiotomy/Perineum: Inspect the perineum for swelling, bruising, and healing, and check for infection. Healing should be evident with minimal discomfort and no excessive swelling or infection. Apply ice packs or warm sitz baths for pain relief and stress the importance of maintaining proper hygiene.
- Legs: Examine the legs for signs of deep vein thrombosis (DVT), such as warmth, redness, swelling, or calf pain. There should be no swelling, redness, or tenderness in the legs. Early ambulation and leg exercises are recommended to promote circulation and reduce the risk of DVT.
- Emotional status: Assess the mother’s emotional well-being, mood, and bonding with her baby during newborn care, asking about feelings of sadness, anxiety, or being overwhelmed, which may indicate postpartum depression. Some "baby blues" are common, but prolonged or severe sadness should be monitored. Provide emotional support, and if signs of depression appear, refer to mental health professionals.
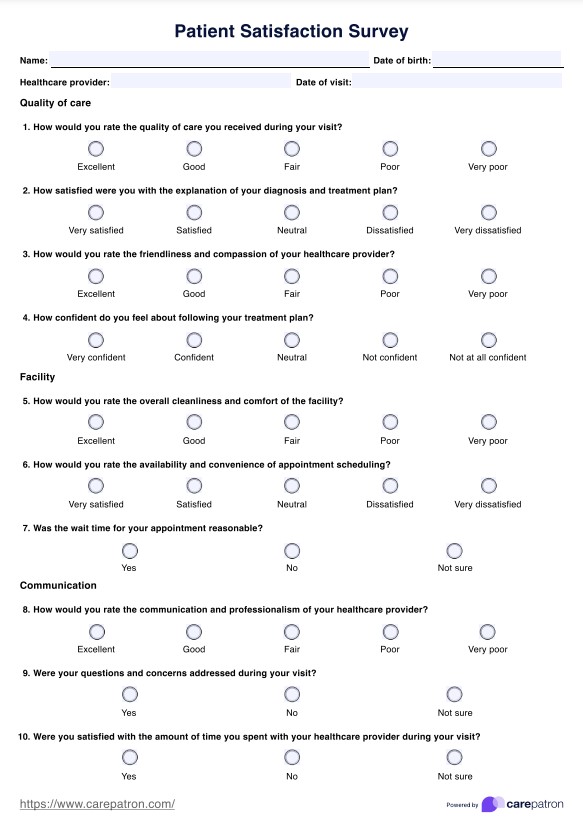
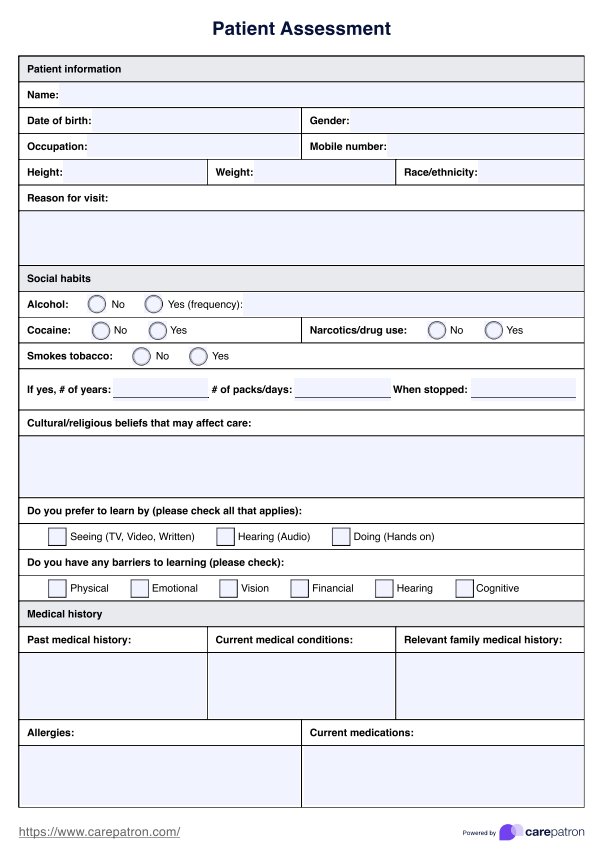
How does our Postpartum Nursing Care Assessment template work?
Carepatron’s Postpartum Nursing Care Assessment template is designed to help healthcare professionals streamline their assessments of new mothers. By using this tool, practitioners can ensure thorough monitoring of patients during the postpartum period, improving both care and outcomes. Below is a step-by-step guide on how to use the template effectively.
Access the template
To get started, users can find the Postpartum Nursing Care Assessment template within this guide. Simply download or access it through Carepatron’s platform, allowing you to begin using the tool right away in your clinical practice.
Review the template content
Once accessed, review the template to familiarize yourself with its sections. The template is organized to cover essential areas of the acronym BUBBLE-LE. It also has fields for vital signs like blood pressure, respiratory rate, and pain level for a thorough evaluation.
Add necessary information and observation
As you evaluate the patient, input the relevant observations. Accurately recording this data ensures a comprehensive postpartum assessment of the mother and informs necessary next steps.
Discuss next steps with patient
After completing the assessment, discuss the findings with the patient. Address concerns like perineal pain or foul-smelling lochia, offer reassurance, and inform them of what to expect in the next phase of their recovery.
Postpartum physiologic changes
During the postpartum period, a woman’s body undergoes several significant changes as it recovers from pregnancy and childbirth. It’s essential for healthcare providers to monitor these changes as well as risk factors closely during the immediate postpartum period to ensure a safe and healthy recovery. Below are the key physiologic changes that can occur:
- Uterine cramping: As the uterus contracts to return to its pre-pregnancy size, uterine cramping is a common occurrence, especially after a vaginal delivery.
- Vaginal bleeding: Normal vaginal bleeding, known as lochia, occurs as the body sheds the lining of the uterus. However, excessive bleeding may indicate postpartum hemorrhage and requires immediate attention.
- Foul-smelling lochia: A foul-smelling lochia can be a sign of infection and should be addressed promptly during postpartum care.
- Uterine tenderness: Persistent uterine tenderness may also signal infection or other complications.
- Bladder distention: A distended bladder can impair uterine contraction, leading to increased blood loss. Proper bladder function should be restored to prevent complications.
- Bowel function: Constipation or delayed bowel function is common after childbirth and requires monitoring.
- Lower extremities: Swelling or pain in the lower extremities could be a warning sign of pulmonary embolism or other circulation issues.
- Chest pain and panic attacks: Emotional and physical stress in the postpartum period may lead to symptoms like chest pain or panic attacks, which should not be ignored.
Commonly asked questions
The immediate assessment of a mother after delivery involves checking vital signs, monitoring for postpartum hemorrhage, and assessing uterine tone and vaginal bleeding to ensure stable recovery. Using Carepatron's Postpartum Nursing Care Assessment template can help healthcare providers streamline this critical evaluation.
Nursing assessments during the postpartum period include monitoring the mother's physical recovery, such as uterine cramping, bladder distention, and perineal pain, while also assessing emotional well-being for signs of postpartum depression. Carepatron’s assessment template helps track these key areas effectively for better patient outcomes.
The 5-5-5 rule advises postpartum women to rest in bed for 5 days, stay around the house for another 5 days, and slowly resume activities over the next 5 days.