Write a good nurse chart by including crucial details and ensuring clarity and objectivity. Use the SOAP format (Subjective, Objective, Assessment, Plan) to comprehensively document normal findings, nursing interventions, and appropriate interventions. This approach helps provide comprehensive care in a hospital setting and supports effective communication with healthcare professionals.
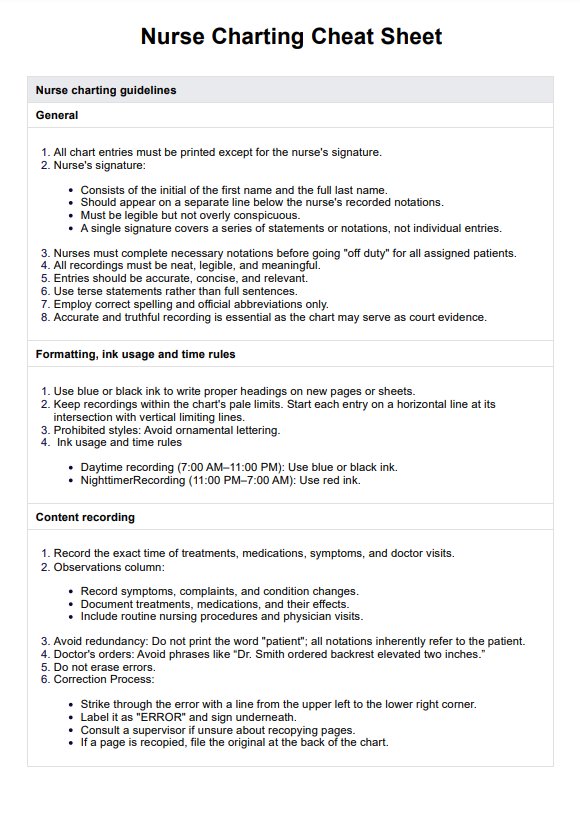
Nurse Charting Cheat Sheet
Streamline your documentation with our Nurse Charting Cheat Sheet. Download the free PDF here.
Use Template
Nurse Charting Cheat Sheet Template
Commonly asked questions
You can chart faster in nursing by focusing on crucial details and prioritizing essential information, such as changes in cardiac output or responses to IV solutions. Use approved shorthand and electronic charting systems to document efficiently while maintaining accuracy.
The four types of nursing documentation include:
- SOAP notes: Structured to include subjective and objective data, assessments, and plans for optimal care.
- Narrative notes: Provide a detailed account of patient status and nursing interventions in a story-like format.
- Nursing assessment flowcharts: Focus on recording normal findings and deviations in a quick and organized way.
- Problem-oriented medical records: Document specific concerns, nursing considerations, and solutions to ensure comprehensive care.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











