Multiple sclerosis (MS) is believed to be an autoimmune disorder where the body's immune system mistakenly attacks its tissues, specifically the myelin sheath in the central nervous system. The exact cause is unknown, but it's thought to involve a combination of genetic susceptibility and environmental factors, such as viral infections and possibly vitamin D deficiency.
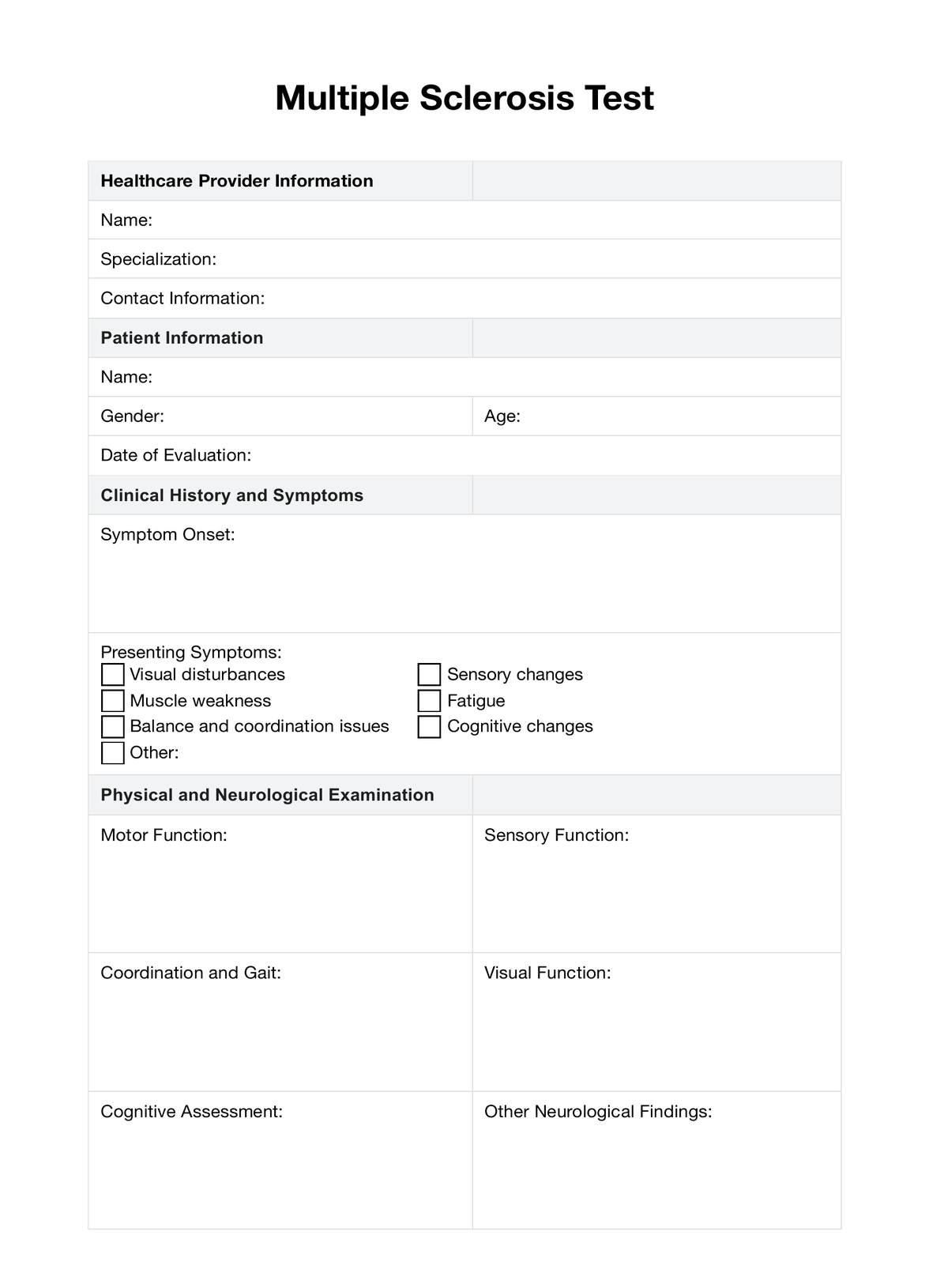
Multiple Sclerosis Test
Discover the symptoms, causes, diagnosis, and treatment options for Multiple Sclerosis and understand comprehensive care approaches.
Multiple Sclerosis Test Template
Commonly asked questions
Currently, there is no known way to prevent Multiple Sclerosis. Since the exact cause of MS is not fully understood, prevention strategies are challenging to develop. However, ongoing research focuses on better understanding of risk factors, which may eventually lead to preventive measures.
While MS is not directly inherited, having a family member with MS can increase an individual's risk of developing the disease. The risk in the general population is about 1%, but it rises to approximately 2-5% for those with a close relative (parent or sibling) who has the disease. This suggests a genetic predisposition can be a factor, although it's not the sole cause of MS.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











