Lupus Diagnosis Criteria
Access Carepatron's free Lupus Diagnosis Criteria PDF and understand key clinical indicators and support accurate assessments with essential resources.


What is lupus?
Lupus is a chronic autoimmune disease that causes the immune system to attack healthy tissues, leading to widespread inflammation (National Institute of Arthritis and Musculoskeletal and Skin Disease, 2022). Systemic lupus erythematosus (SLE) is the most common form, affecting multiple organs, including the central nervous system, skin, joints, kidneys, and blood cells.
Cutaneous lupus erythematosus primarily affects the skin (Kole & Ghosh, 2009). The disease can lead to blood disorders, including anemia and leukopenia, by targeting red blood cells and white blood cells. Some patients develop lupus anticoagulant, increasing the risk of clotting. Mixed connective tissue disease may overlap with lupus (Sapkota & Al Khalili, 2020), and blood tests are essential for diagnosing active SLE disease and assessing severity.
Types
Lupus is classified into several types based on organ involvement and disease characteristics. As mentioned,ystemic lupus erythematosus is the most common (Vaillant et. al., 2023), affecting multiple systems, including the kidneys, skin, and heart. Discoid lupus erythematosus (DLE) is a form of cutaneous lupus erythematosus that causes discoid lesions and scarring (.
Drug-induced lupus mimics SLE but resolves after stopping the triggering medication. Neonatal lupus occurs in newborns due to maternal antibodies. Some cases overlap with other autoimmune disorders, such as systemic sclerosis. Identifying the correct type through a blood test and meeting diagnostic criteria is essential for proper management.
Symptoms
Lupus symptoms vary but commonly include joint pain, fatigue, and chest pain from pleuritis or pericarditis. Neurologic symptoms, such as seizures and cognitive dysfunction, can indicate active lupus. Pulmonary hypertension and interstitial lung disease may develop, leading to respiratory issues.
Skin manifestations like discoid lesions and photosensitivity are frequent in cutaneous lupus erythematosus. Blood abnormalities, including anemia and thrombocytopenia, are diagnosed via antinuclear antibody testing and other blood tests. Disease severity fluctuates, with periods of remission and flare-ups that require ongoing monitoring.
Risks
Lupus increases the risk of cardiac disease, kidney dysfunction, and clotting disorders. Lupus anticoagulant raises the likelihood of thrombosis, leading to complications such as stroke or deep vein thrombosis. Chronic inflammation may cause permanent organ damage, particularly in the kidneys and cardiovascular system.
Pulmonary hypertension can arise from long-term lung involvement, while interstitial lung disease affects breathing capacity. Coexisting autoimmune disorders, such as systemic sclerosis, further complicate management. Physicians must assess active lupus progression through blood tests and imaging to prevent severe complications.
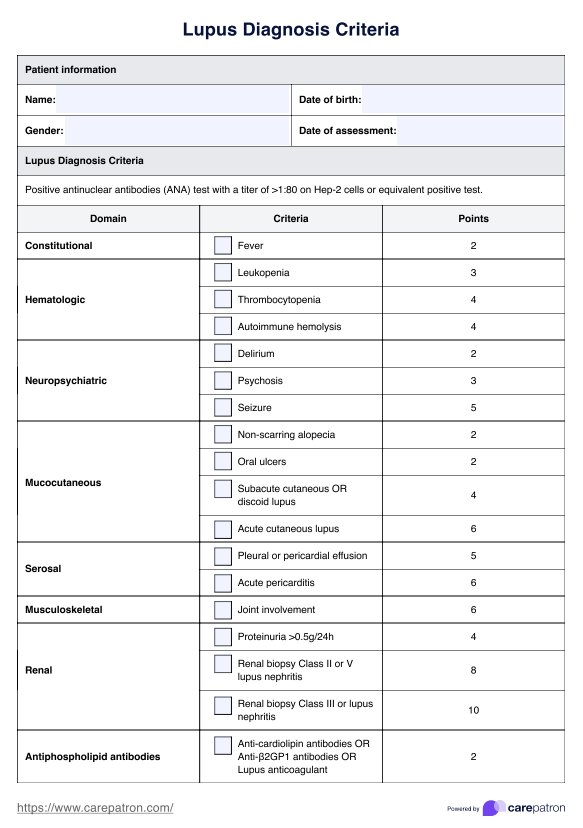
Lupus Diagnosis Criteria Template
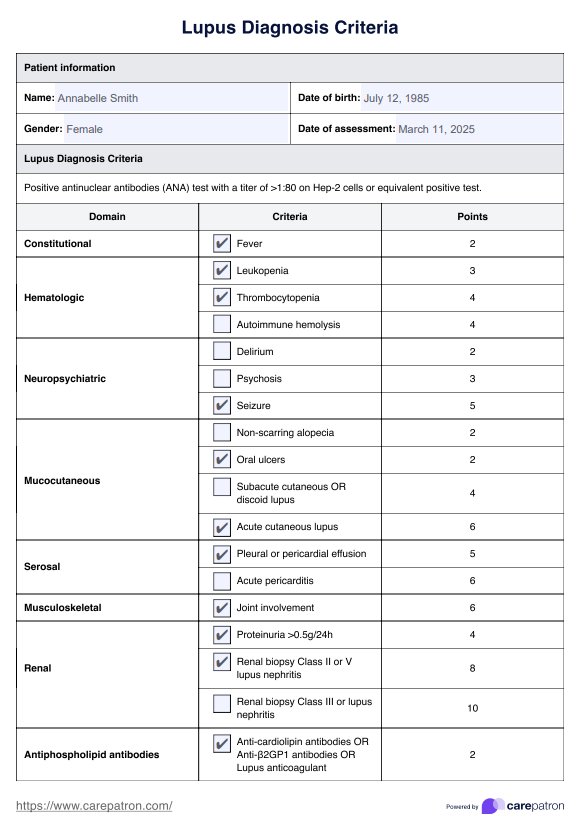
Lupus Diagnosis Criteria Example
What is the Lupus Diagnosis Criteria?
Diagnosing lupus is challenging due to its diverse symptoms and its ability to mimic other conditions. To aid in diagnosis, healthcare practitioners rely on established criteria. In 2019, the European League Against Rheumatism (EULAR) and the American College of Rheumatology (ACR) introduced updated classification criteria for systemic lupus erythematosus. The EULAR/ACR criteria offer a specificity of 93.4% and a sensitivity of 96.1%, improving diagnostic accuracy (Vaillant et al., 2023).
The EULAR/ACR 2019 classification criteria for SLE emphasize a weighted, point-based system that requires at least one positive antinuclear antibody (ANA) test at a titer of ≥1:80 as an entry criterion. Once this criterion is met, additional clinical and immunological criteria are assessed, with a total score of ≥10 indicating a classification of SLE. The criteria are categorized into seven clinical domains and three immunological domains, each assigned weighted scores based on their specificity for lupus.
How does our Lupus Diagnosis Criteria template work
Carepatron’s Lupus Diagnosis Criteria template streamlines the diagnostic process by providing a structured, evidence-based approach. The following steps outline how to effectively integrate this template into clinical practice for accurate lupus assessment and patient care.
Step 1: Access the diagnosis template
To begin, click the “Use template” button to access the Lupus Diagnosis Criteria template directly through Carepatron. This will guide you to the platform, where you can download and integrate it into your workflow. The template is designed to standardize assessments, ensuring consistency in diagnosing systemic lupus erythematosus.
Step 2: Use the template in patient assessment
During consultation, input patient information and clinical findings into the template. Evaluate symptoms, laboratory results, and blood test abnormalities, such as antinuclear antibody positivity or lupus anticoagulant presence. The structured scoring system helps determine whether the patient meets the diagnostic criteria, aiding in a comprehensive and objective assessment.
Step 3: Discuss findings and diagnosis with the patient
Once the assessment is complete, review the calculated score and clinical evidence. If active lupus is indicated, explain the findings, focusing on neurologic symptoms, discoid lesions, and organ involvement. Clearly communicate uncertainty if additional testing is required, ensuring the patient understands the diagnostic process and potential implications of their results.
Step 4: Provide further patient education and next steps
Following diagnosis, educate the patient on their condition, emphasizing lupus triggers, symptom monitoring, and lifestyle considerations. If the Lupus Diagnosis Criteria score is inconclusive, recommend further testing, such as repeat blood tests or imaging. Collaborate on a management plan, including referrals to specialists if cardiac disease or pulmonary hypertension is a concern.
Benefits of using this criteria template
The Lupus Diagnosis Criteria template improves efficiency in diagnosing SLE patients by standardizing clinical findings and ensuring accuracy. Given that lupus affects multiple organ systems, this structured approach helps differentiate it from other autoimmune diseases like rheumatoid arthritis. The template systematically evaluates antinuclear antibodies, c-reactive protein, and hematologic abnormalities, aiding in early identification of renal disorders and systemic complications.
It also facilitates a clear assessment of skin rashes, nasal ulcers, and reactions to sun exposure, ensuring a comprehensive review of early disease manifestations. By integrating these objective measures, medical professionals can enhance clinical diagnosis accuracy and streamline workflows.
References
Kole, A. K., & Ghosh, A. (2009). Cutaneous manifestations of systemic lupus erythematosus in a tertiary referral center. Indian Journal of Dermatology, 54(2), 132–136. https://doi.org/10.4103/0019-5154.53189
National Institute of Arthritis and Musculoskeletal and Skin Diseases. (2022, October). Systemic lupus erythematosus (lupus). National Institutes of Health. https://www.niams.nih.gov/health-topics/lupus
Sapkota, B., & Al Khalili, Y. (2020). Mixed connective tissue disease. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK542198/
Vaillant, A. A. J., Goyal, A., Bansal, P., & Varacallo, M. (2023, August 4). Systemic lupus erythematosus. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK535405/
Commonly asked questions
Lupus is identified through clinical findings such as skin rashes, nasal ulcers, joint pain, and organ involvement, along with laboratory markers like antinuclear antibodies and c-reactive protein levels. A confirmed diagnosis requires meeting established diagnostic criteria, including a combination of symptoms, hematologic abnormalities, and immunologic tests.
The four main types of lupus are systemic lupus erythematosus (SLE), cutaneous lupus erythematosus, drug-induced lupus, and neonatal lupus. SLE patients experience multi-organ involvement, while cutaneous lupus primarily affects the skin, and drug-induced lupus resolves after stopping the triggering medication.
Lupus has no cure, but early disease detection and targeted management can control symptoms and prevent complications. Treatment focuses on suppressing the immune response, reducing inflammation, and addressing organ-specific damage, such as renal disorders and hematologic abnormalities.
Lupus is diagnosed based on clinical diagnosis supported by laboratory tests, including antinuclear antibodies, c-reactive protein, and hematologic abnormalities. The Lupus Diagnosis Criteria template standardizes assessments by evaluating clinical findings, symptoms, and test results to confirm SLE patients meet diagnostic thresholds.