Ineffective Airway Clearance Nursing Care Plan
Ineffective airway clearance can hinder breathing and oxygenation. Discover effective nursing care plans and interventions to enhance patient respiratory health.


What is ineffective airway clearance
Ineffective airway clearance is defined as the inability to effectively clear secretions or obstructions from the respiratory tract. This can impede a patient's ability to deep breath or maintain adequate oxygenation and increase airway resistance. This condition is noted in an ineffective airway clearance, which can lead to difficulty breathing and, if unaddressed, may cause complications such as decreased oxygen saturation and airway obstruction.
Ineffective airway clearance can be triggered by several factors, including:
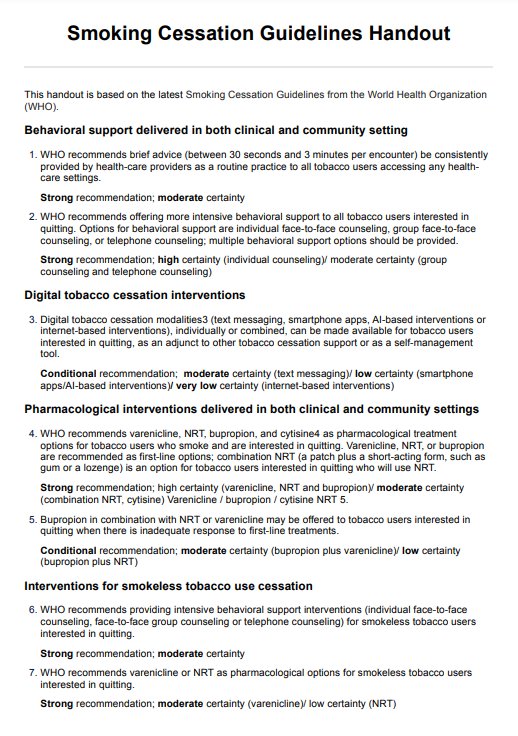
- Smoking or smoke inhalation
- Chronic obstructive pulmonary disease (COPD)
- Asthma
- Respiratory infections
- Sedation from anesthesia
- Paralysis resulting from stroke or spinal cord injury
- Neuromuscular disorders
- Presence of artificial airways
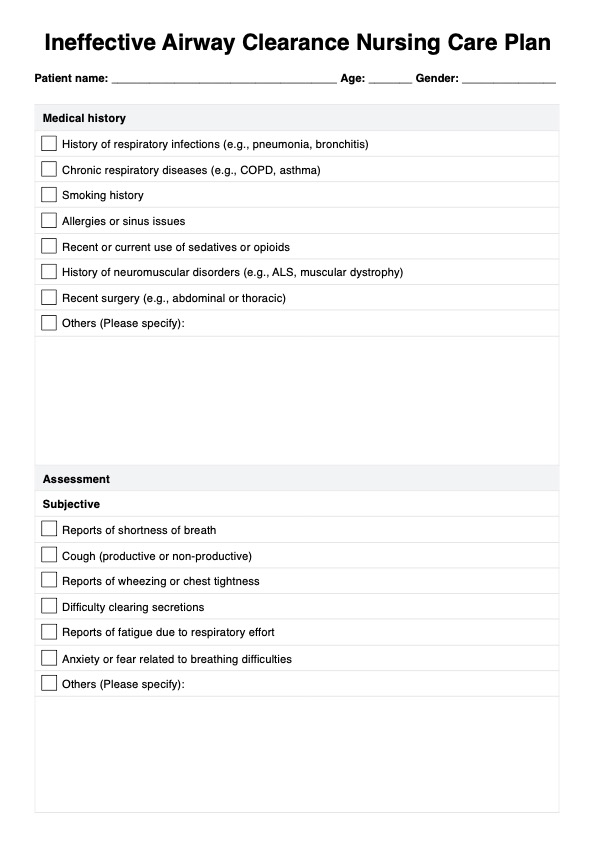
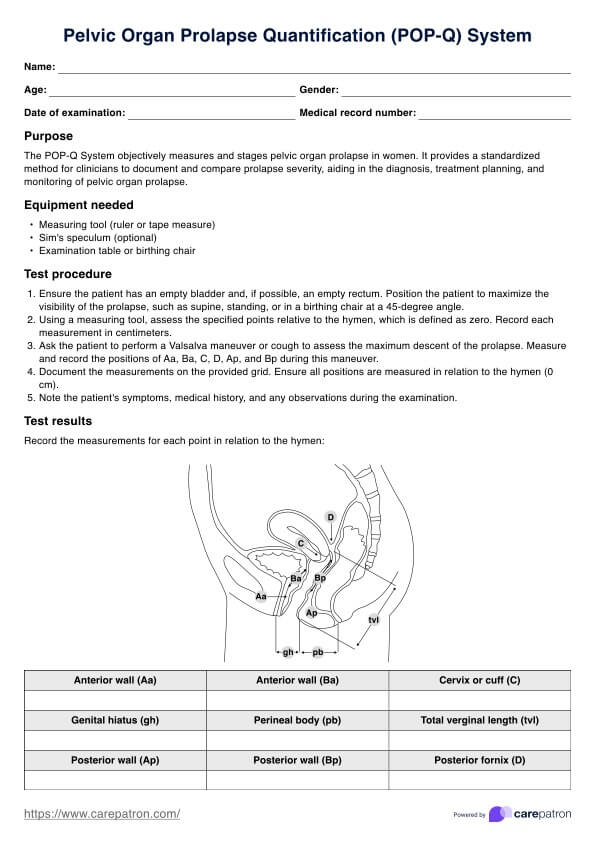
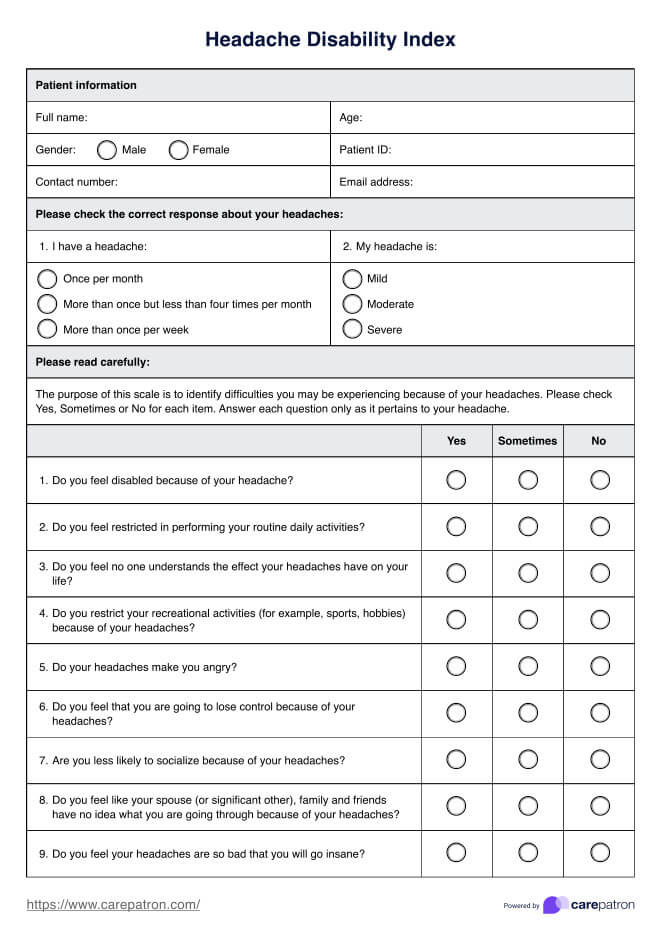
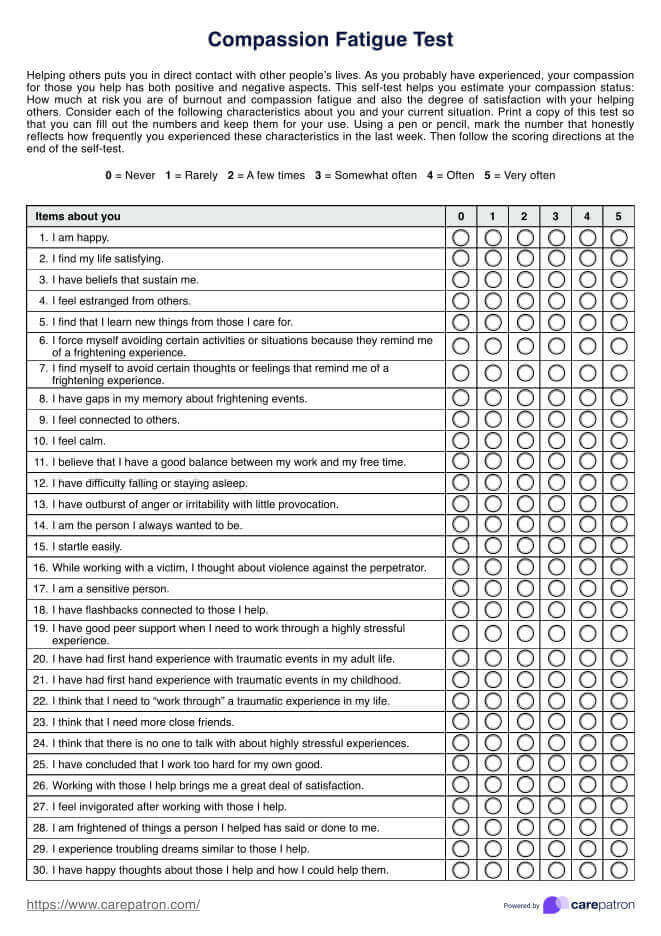
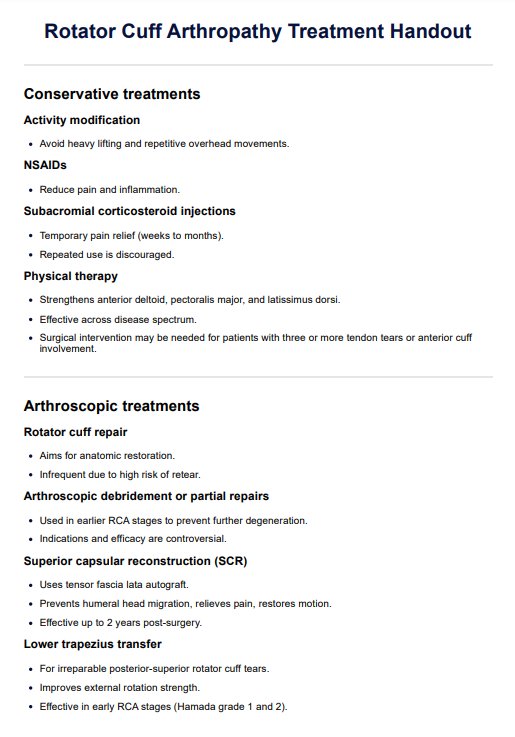
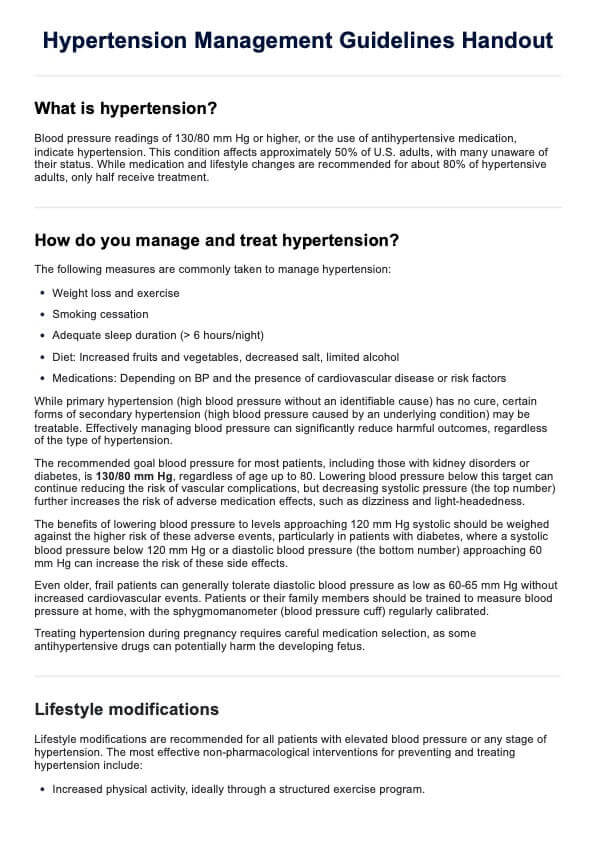
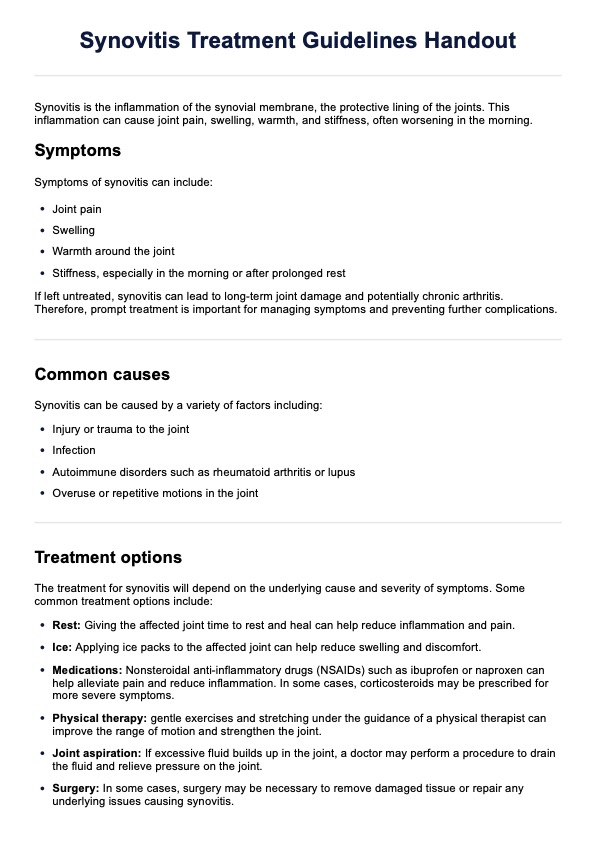
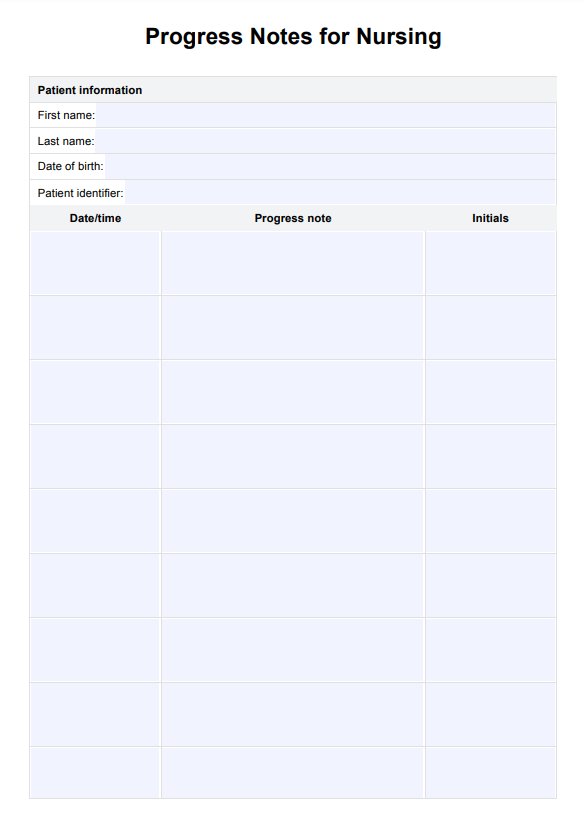
Ineffective Airway Clearance Nursing Care Plan Template
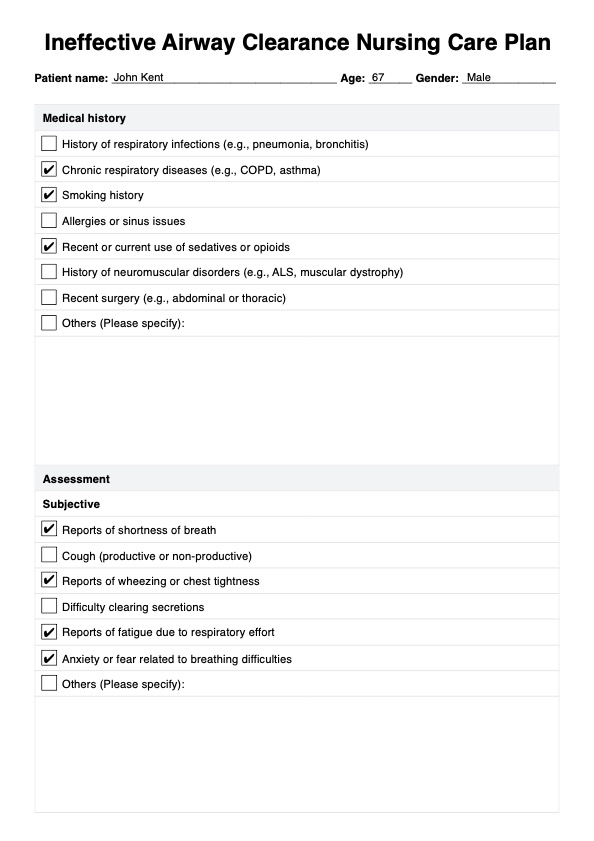
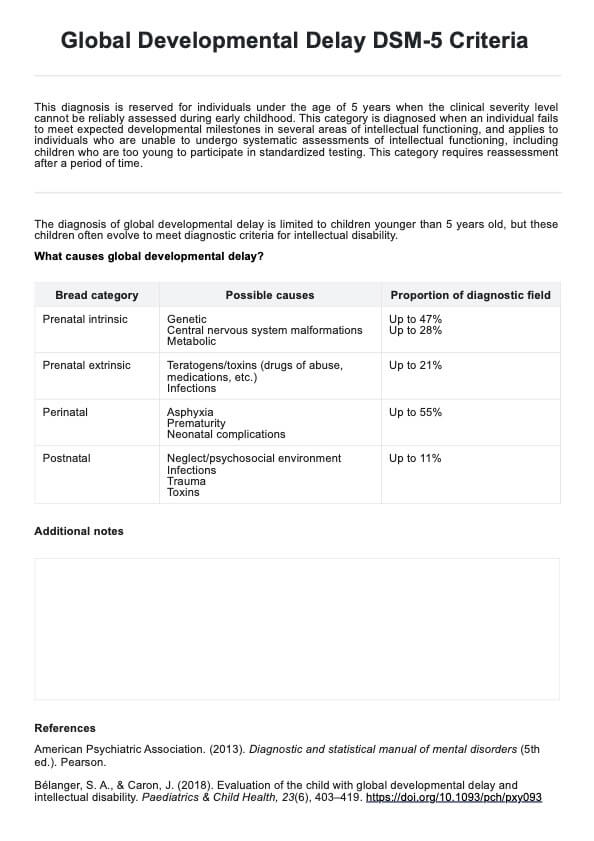
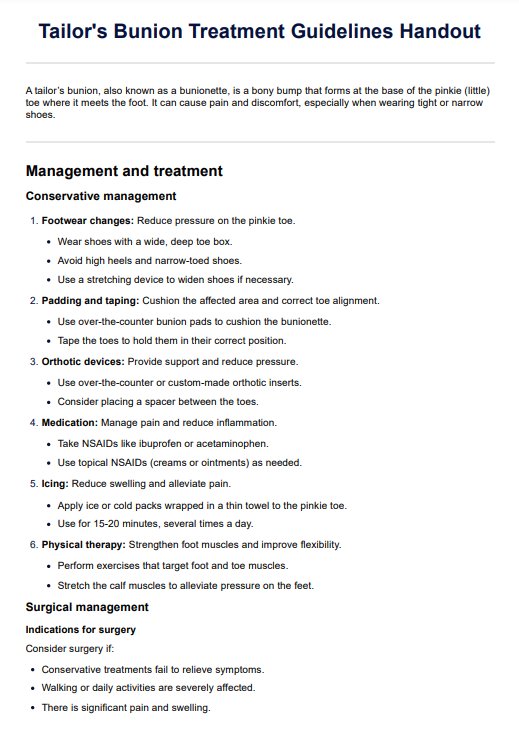
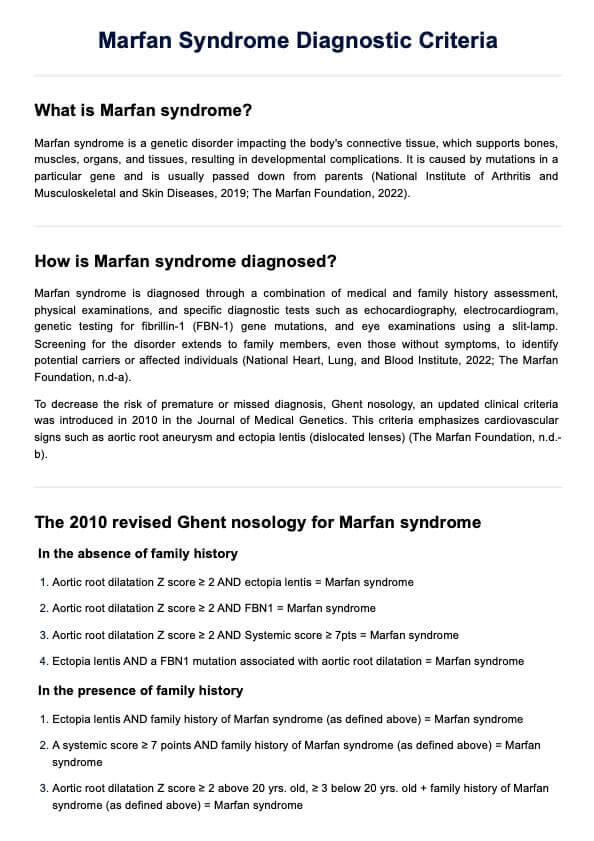
Ineffective Airway Clearance Nursing Care Plan Example
What is Ineffective Airway Clearance Nursing Care Plan Template
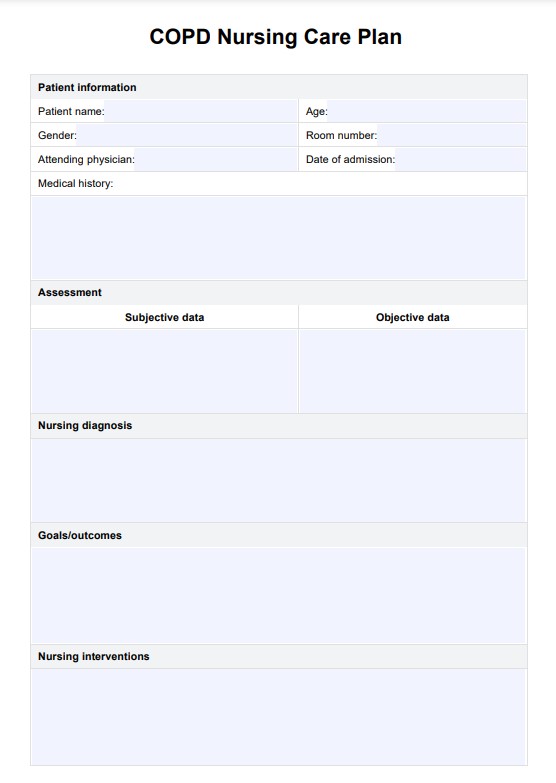
An Effective Airway Clearance Nursing Care Plan Template is essential for nurses to manage patients with compromised respiratory function, such as those with COPD, asthma, or post-surgical respiratory challenges like tracheostomy. This template guides nurses from the initial assessment of respiratory status—including breathing patterns, lung sounds, and risk factors—to diagnosis, helping to create a personalized care plan.
The care plan includes specific goals to improve oxygenation, lung capacity, and patient comfort. It also outlines targeted interventions, such as airway suctioning, bronchodilators, chest physiotherapy, positioning techniques, prescribed medications, and breathing exercises. Regular evaluation ensures that the care plan is responsive to the patient’s changing needs, promoting effective and patient-centered respiratory care.
How does it work?
Here are the steps involved in using the Ineffective Airway Clearance Nursing Care Plan Template:
Step 1: Nursing assessment of the patient
The initial step involves comprehensively evaluating the patient's respiratory status. This includes observing lung sounds and the breathing pattern, noting any cough or secretions, and assessing signs of respiratory distress like cyanosis or using accessory muscles for breathing.
Step 2: Diagnosis
Based on the assessment, the nurse identifies an inneffective airway clearance nursing diagnosis or nursing diagnoses related to ineffective airway clearance. These diagnoses could include but are not limited to, altered breathing patterns, increased respiratory rate, or the presence of adventitious lung sounds.
Step 3: Planning
In this phase, the nurse sets realistic, measurable goals tailored to the patient's condition. Goals may include improving airway patency, enhancing the effectiveness of the cough mechanism, or reducing the risk of respiratory infections.
Step 4: Intervention
The nurse then outlines specific interventions to address the airway clearance issues. These interventions could involve suctioning to clear secretions, administering bronchodilators or mucolytic agents, providing chest physiotherapy, teaching effective coughing techniques, and ensuring proper positioning to facilitate breathing.
Step 5: Evaluation
The final step is a continuous process where the nurse regularly assesses the patient's progress toward the set goals. This includes re-evaluating the respiratory status, monitoring the effectiveness of the interventions, and making necessary adjustments to the care plan.
When would you use this template?
The Ineffective Airway Clearance Nursing Care Plan Template is invaluable in nursing interventions in various clinical settings, particularly where patients grapple with respiratory challenges. Its application is wide-ranging and critically important in ensuring that patients with compromised respiratory function receive comprehensive and targeted nursing care.
- Chronic respiratory conditions: This template is extensively used for patients with chronic respiratory diseases like COPD, asthma, or cystic fibrosis. In these cases, the template helps systematically manage the chronic nature of these conditions, focusing on reducing exacerbations and maintaining optimal lung function.
- Acute respiratory illnesses: In acute respiratory conditions such as pneumonia, bronchitis, or acute respiratory distress syndrome (ARDS), the template is a guide for managing sudden and severe respiratory impairments. It aids in outlining urgent care strategies and monitoring their effectiveness.
- Postoperative care: Post-surgical patients, especially those undergoing thoracic or abdominal surgery, often require meticulous respiratory monitoring and care. The template assists in planning postoperative interventions to prevent complications like atelectasis or pneumonia.
- Patients with tracheostomies or mechanical ventilation: For individuals with tracheostomies or those on mechanical ventilation, the template provides a structured approach to managing and monitoring airway clearance, ensuring airway patency, and preventing infections.
- Neurological conditions impacting respiration: In conditions like Guillain-Barré syndrome or severe neuromuscular disorders, where respiratory muscles are affected, this template is crucial in planning and executing care strategies to maintain airway clearance.
- Emergency and intensive care: In emergency and ICU settings, the template is vital for managing patients with life-threatening respiratory conditions, providing a framework for rapid assessment and intervention.
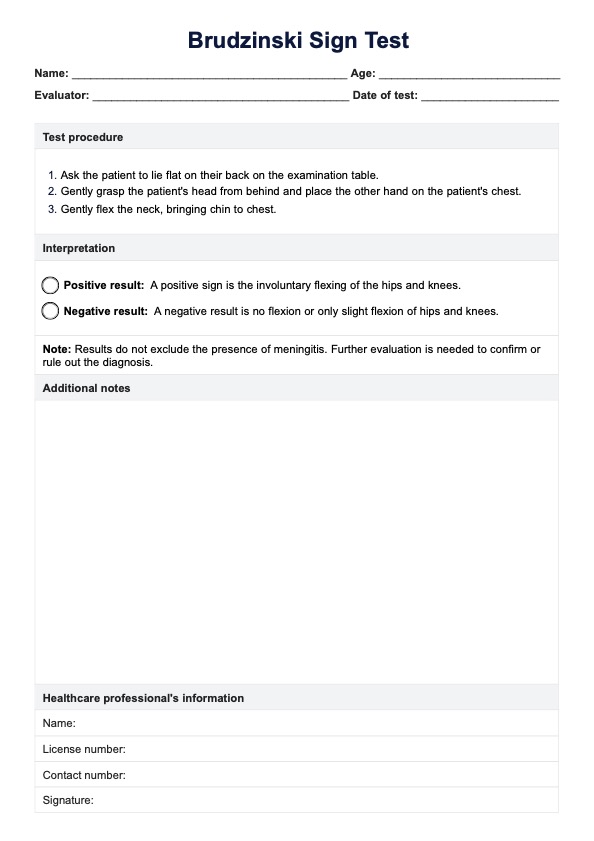
Nursing diagnosis and care planning
When developing a nursing diagnosis for ineffective airway clearance, nurses must assess the unique causes and clinical manifestations of airway obstruction or secretion buildup in each patient.
Key expected outcomes for patients with an ineffective airway clearance diagnosis include:
- Maintaining a patent airway: The primary goal is to achieve a clear airway, which can be supported through suctioning, positioning, and hydration. These actions help prevent airway blockages and ensure the patient can breathe more freely.
- Demonstrating effective coughing and secretion clearance: A critical outcome is for the patient to develop the ability to cough effectively and clear secretions independently. Nurses may employ techniques such as chest physiotherapy, deep breathing exercises, and education on coughing techniques to facilitate this process.
- Exhibiting normal breath sounds and respiratory patterns: The return of clear, unobstructed breath sounds and a stable respiratory pattern signals effective airway clearance. Nurses monitor respiratory rate, rhythm, and lung sounds to assess for improvements, while treatments may include respiratory medications and techniques like pursed lip breathing to enhance respiratory function.
- Maintaining oxygen saturation within normal limits: Keeping oxygen saturation at a healthy level is essential for adequate oxygenation. This is achieved by addressing underlying causes of airway obstruction and, when necessary, using supplemental oxygen.
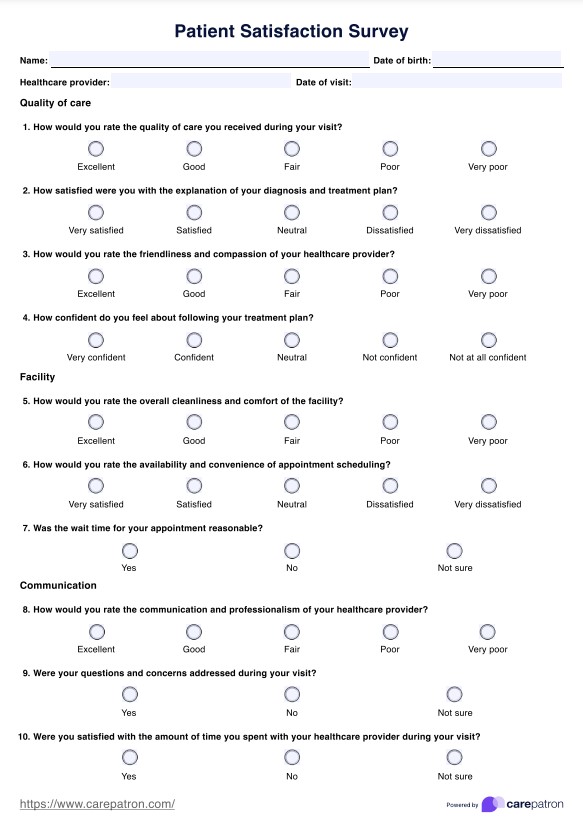
Benefits of using our Ineffective Airway Clearance Nursing Care Plan Template
Using an Ineffective Airway Clearance Nursing Care Plan Template provides a structured approach that supports healthcare practitioners in addressing issues associated with an ineffective airway clearance nursing diagnosis. Here’s how it benefits patient care and integrates essential elements to support the respiratory system:
Streamlined assessment
The template allows for a focused assessment of the respiratory system, helping practitioners quickly identify signs of ineffective airway clearance related to symptoms like abnormal breath sounds, an ineffective breathing pattern, coughing, or shallow breathing. Evaluating factors like respiratory rate and oxygen saturation helps determine the patient’s need for supplemental oxygen and other interventions.
Guided intervention planning
By offering evidence-based intervention guidelines, the template facilitates targeted approaches, such as pursed lip breathing, to assist with ineffective breathing patterns and encourage proper lung expansion. This promotes optimal oxygen intake and clearance of secretions by engaging abdominal muscles for effective coughing.
Enhanced monitoring and safety
Using the template supports monitoring vital respiratory parameters, such as respiratory rate and arterial blood gases. Regularly assessing these indicators enables practitioners to track progress and ensure the patient’s airway remains clear and oxygenated. Instructions to monitor oxygen saturation and blood pressure levels and provide supplemental oxygen when necessary ensure timely adjustments to the care plan to prevent complications.
Thorough documentation
The template includes sections for comprehensive documentation of symptoms, interventions, and outcomes, ensuring that care teams have access to all relevant patient information. Documenting observations such as breath sounds, cough effectiveness, and response to interventions like lung expansion exercises or pursed lip breathing facilitates better communication and continuity of care.
Commonly asked questions
A nurse should reevaluate the care plan if there are changes in the patient's respiratory status, lack of improvement in symptoms, or if new complications arise that may affect airway clearance.
The primary goals include improving airway patency, enhancing the effectiveness of coughing, increasing oxygenation, and reducing the risk of respiratory infections.
Nurses can assess airway clearance by observing breathing patterns, listening for abnormal lung sounds, checking oxygen saturation levels, and evaluating the effectiveness of the cough reflex.

.jpg)