Gout Diagnosis Criteria
Uncover the essential Gout Diagnosis Criteria here, including symptoms, diagnostic tests, and the American College of Rheumatology guidelines.


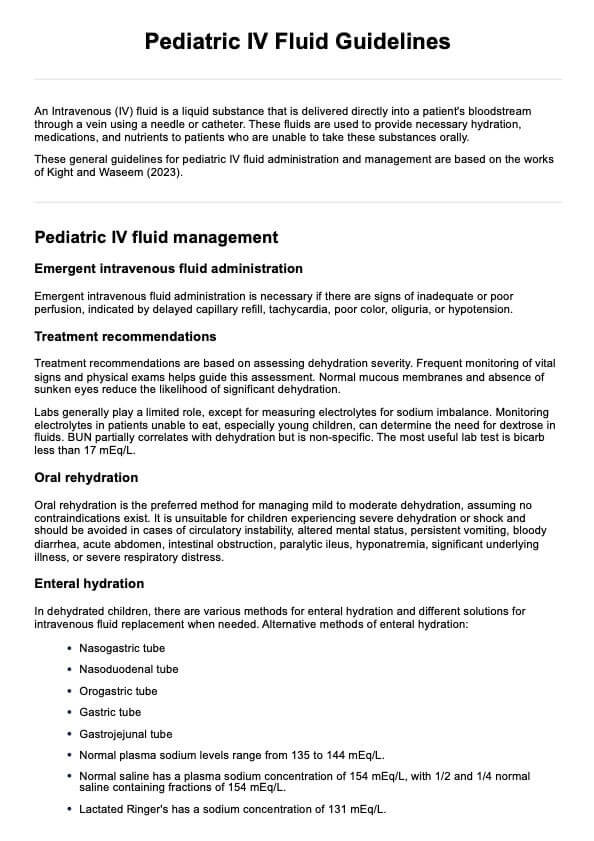
What is gout?
Gout, also known as gouty arthritis, is a common form of inflammatory arthritis characterized by sudden, severe attacks of pain, swelling, redness, and tenderness in the joints. Gout typically affects the joint at the base of the big toe, but it can also occur in other joints such as the ankles, knees, wrists, fingers, and elbows.
The condition is caused by the accumulation of urate crystals in the joints, resulting from elevated levels of uric acid in the blood. Uric acid is a waste product formed from the breakdown of purines, which are substances found in various foods and in the body's cells. When the body produces too much uric acid or the kidneys excrete too little, uric acid can build up and form needle-like crystals in the joints, triggering the inflammatory response seen in gout.
Acute gout attacks often occur suddenly, often at night, and can be triggered by factors such as alcohol consumption, high-purine foods, stress, and certain medications. Chronic gout (also known as chronic gouty arthritis), on the other hand, involves repeated episodes of pain and inflammation, which can eventually lead to joint damage and tophi, which are lumps of urate crystals that can form under the skin.
The American College of Rheumatology, publisher of the journal Arthritis & Rheumatology (Arthritis Rheum), provides guidelines for diagnosing and managing gout. According to their criteria, a gout diagnosis can be confirmed by identifying urate crystals in joint fluid or the presence of a tophus.
The prevalence of gout varies by region and demographic factors, with the condition being more common in men than in women and increasing in frequency with age. Risk factors for developing gout include genetics, obesity, hypertension, kidney disease, and certain dietary habits.
Symptoms of gout
Gout symptoms can vary depending on the stage of the condition. In the early stages, known as acute gout or acute gouty arthritis, symptoms typically come on suddenly and can include:
- Intense joint pain: Gout usually affects the large joint of the big toe but can occur in any joint. The pain is most severe within the first four to twelve hours after it begins.
- Lingering discomfort: After the severe pain subsides, some joint discomfort may last from a few days to a few weeks. Later attacks are likely to last longer and affect more joints.
- Inflammation and redness: The affected joint or joints become swollen, tender, warm, and red.
- Limited range of motion: As gout progresses, you may not be able to move your joints normally.
In the later stages, known as chronic gout, the symptoms can become more persistent and can include:
- Chronic joint pain: The pain and inflammation can become chronic, affecting more than one joint.
- Tophi: The formation of tophi, which are hard, uric acid crystals deposits under the skin, can occur. Tophi can develop in various areas such as the fingers, toes, elbows, or ears.
- Joint damage: Untreated gout can lead to joint damage and deformity.
How is this different from arthritis?
Gout is often classified as a type of arthritis due to the inflammation it causes in the joints. However, it is distinct from other forms of arthritis in several ways:
- Gout (acute gouty arthritis): Caused by the accumulation of uric acid crystals in the joints, leading to intense pain and swelling, typically in one joint at a time. Attacks are sudden and severe, often occurring at night.
- Rheumatoid arthritis: An autoimmune disorder causing chronic inflammation of multiple joints, with persistent symptoms that develop gradually.
- Osteoarthritis: Characterized by the gradual wear and tear of joint cartilage, without the formation of uric acid crystals.
- Septic arthritis (acute arthritis): Caused by an infection in the joint, leading to pain, swelling, and fever. This condition requires immediate medical attention.
Understanding the differences between these types of arthritis is crucial for accurate diagnosis and effective treatment.
Primary gout vs. secondary gout
Primary gout, also known as idiopathic gout, is the most common form and occurs when the body produces too much uric acid or fails to excrete it properly. This imbalance can be due to genetic factors, lifestyle choices such as diet and alcohol consumption, or the natural aging process.
In primary gout, the kidneys may be healthy but are unable to keep up with the excess uric acid, leading to its accumulation and crystal formation in the joints. The management of primary gout focuses on long-term lifestyle changes and medication to control uric acid levels and prevent future attacks.
Secondary gout, on the other hand, results from other medical conditions or treatments that increase uric acid levels. For example, certain cancers, blood disorders, and kidney diseases can lead to secondary gout. Medications such as diuretics and low-dose aspirin can also contribute to its development.
In these cases, treating the underlying condition or adjusting medication can often alleviate the gout symptoms. Understanding the distinction between primary and secondary gout is essential for healthcare professionals to provide targeted and effective treatment, addressing both the symptoms and the root cause of the elevated uric acid levels.
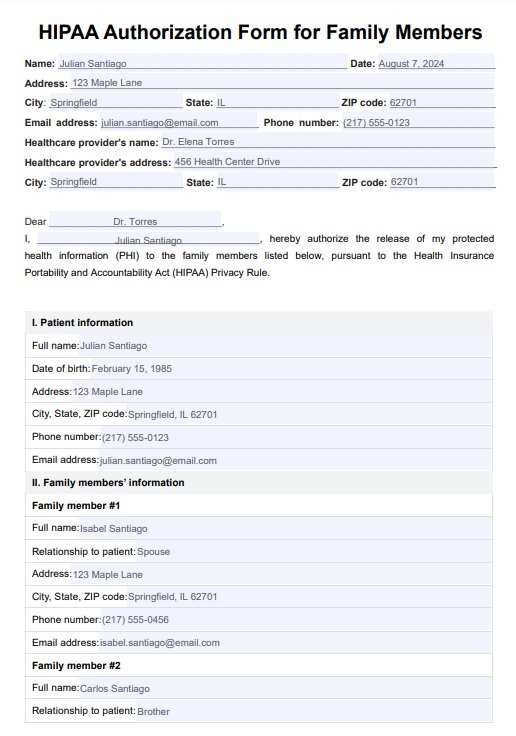
Gout Diagnosis Criteria Template
Gout Diagnosis Criteria Example
How do healthcare professionals diagnose gout?
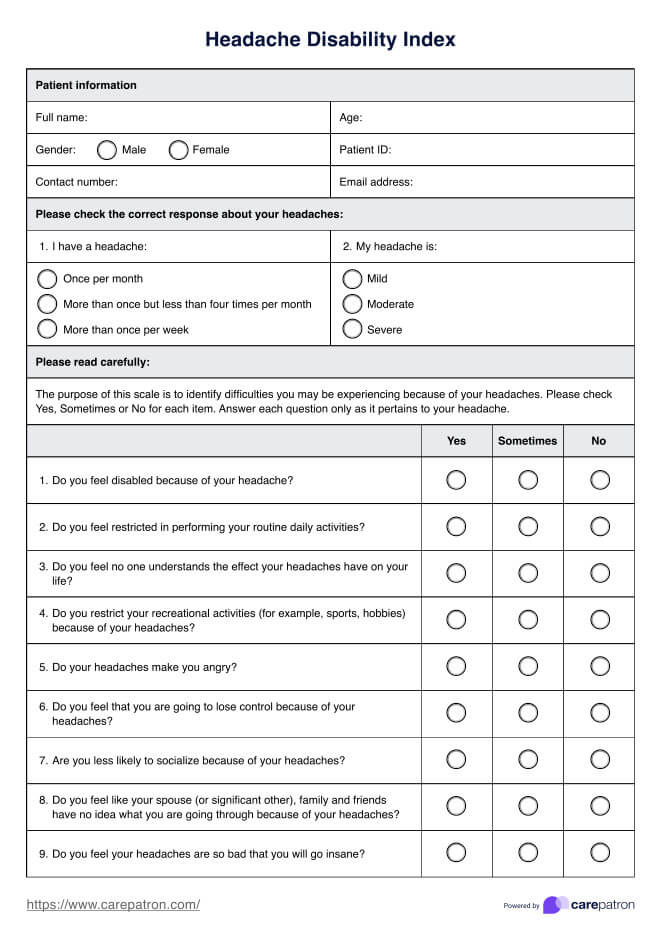
Diagnosing gout involves a comprehensive evaluation by healthcare professionals to distinguish it from other conditions that may present with similar symptoms, such as rheumatoid arthritis or pseudogout. The diagnostic process can be dividend into three parts, each with its own smaller parts:
1. Clinical evaluation
A thorough clinical evaluation is the first step in diagnosing gout. This includes assessing the patient's medical history and conducting a physical examination. Here's what this evaluation entails:
- Medical history: The healthcare professional will inquire about the patient's symptoms, duration of attacks, frequency of episodes, and any family history of gout.
- Physical examination: The physician will examine the affected joints for signs of inflammation, swelling, redness, and tenderness.
2. Laboratory tests
Laboratory tests are crucial for confirming the presence of high uric acid levels and identifying urate crystals in the joint fluid. Here are the relevant lab tests:
- Blood test: A blood sample may be taken to measure the levels of uric acid in the blood. High uric acid levels are associated with gout, but they can also be elevated in people without gout or normal during a gout attack.
- Synovial fluid analysis (joint fluid analysis): If the diagnosis is uncertain, a healthcare professional may use a needle to draw fluid from the affected joint (joint aspiration) and examine it for urate crystals under a microscope. The presence of urate crystals confirms a diagnosis of gout.
3. Imaging tests
Imaging tests play a supportive role in diagnosing gout by visualizing joint changes and detecting urate crystals. These tests may be done:
- X-rays: While X-rays cannot detect gout in the early stages, they can help rule out other causes of joint inflammation and assess any joint damage in chronic gout.
- Ultrasound: This imaging technique can detect urate crystals in joints, even when there are no visible signs of a gout attack.
- Dual-energy CT scan: This specialized CT scan can detect the presence of urate crystals in joints, even when not flaring, but it is not commonly used for diagnosing gout due to its high cost.
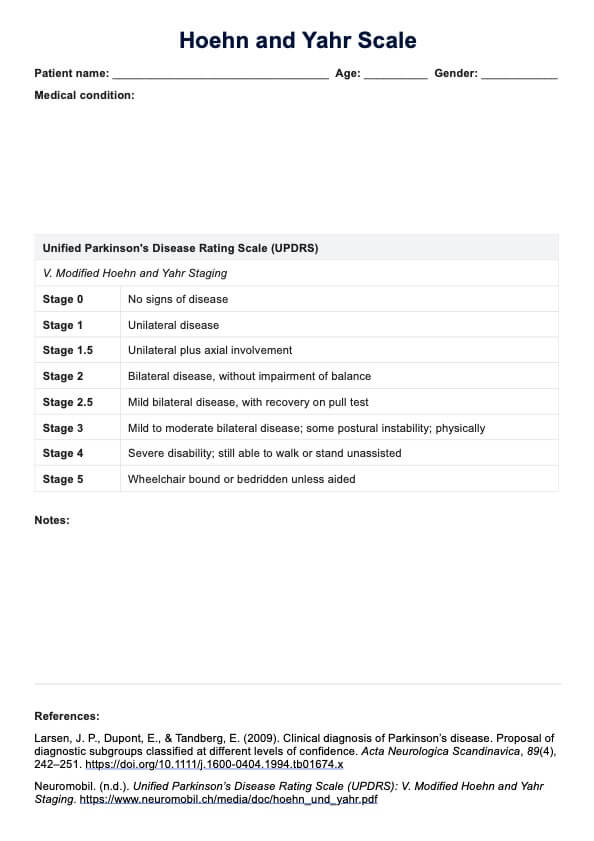
What are the diagnostic criteria for gout?
To accurately diagnose gout, healthcare professionals rely on specific clinical diagnostic criteria. The American College of Rheumatology (ACR) and the European League Against Rheumatism (EULAR) have jointly developed the ACR/EULAR Gout Classification Criteria which serve as both diagnostic and classification criteria for gout.
These criteria are the new gout classification criteria for clinical studies and research rather than for diagnosing individual patients, but they can still provide valuable guidance for healthcare professionals.
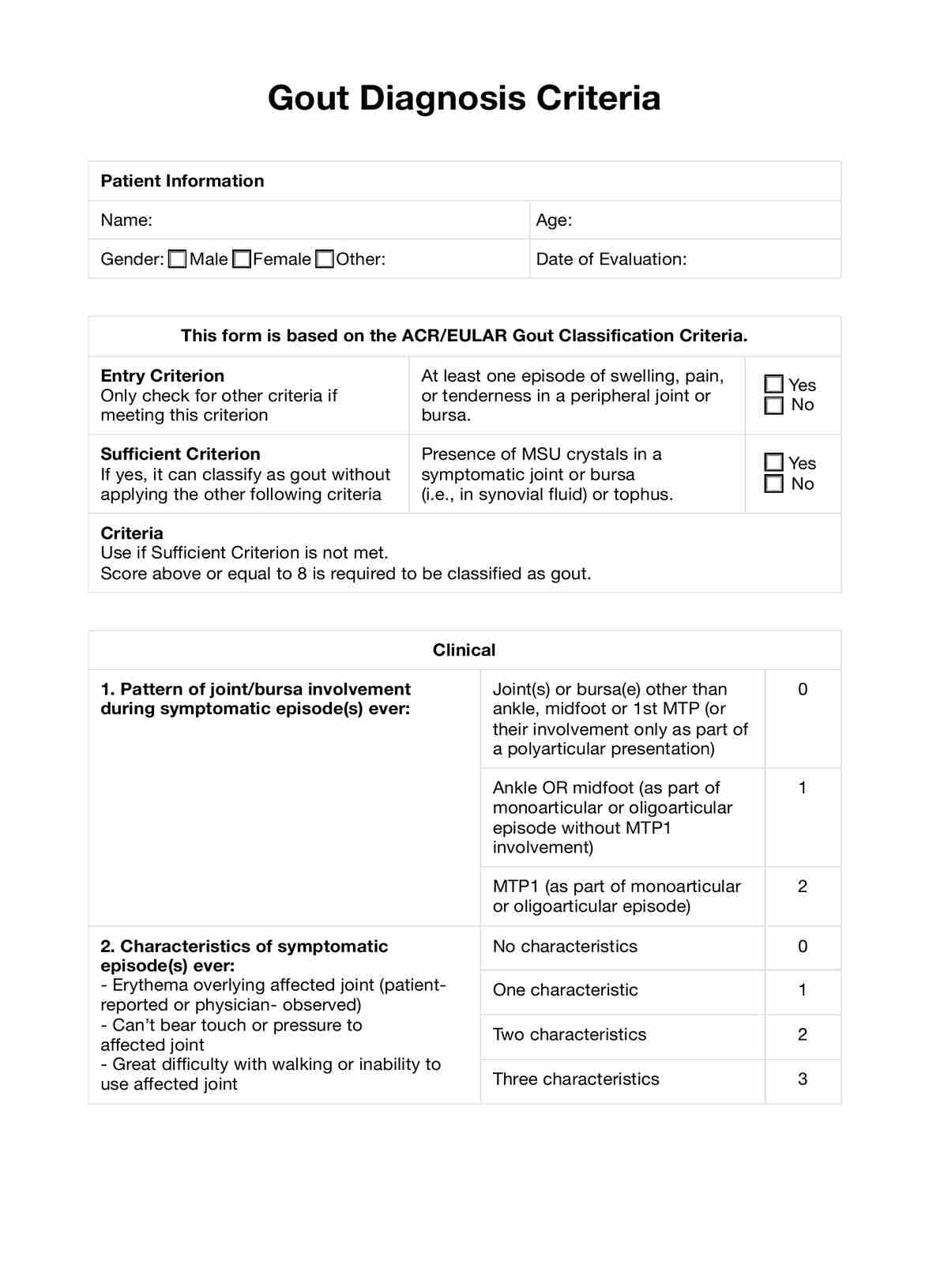
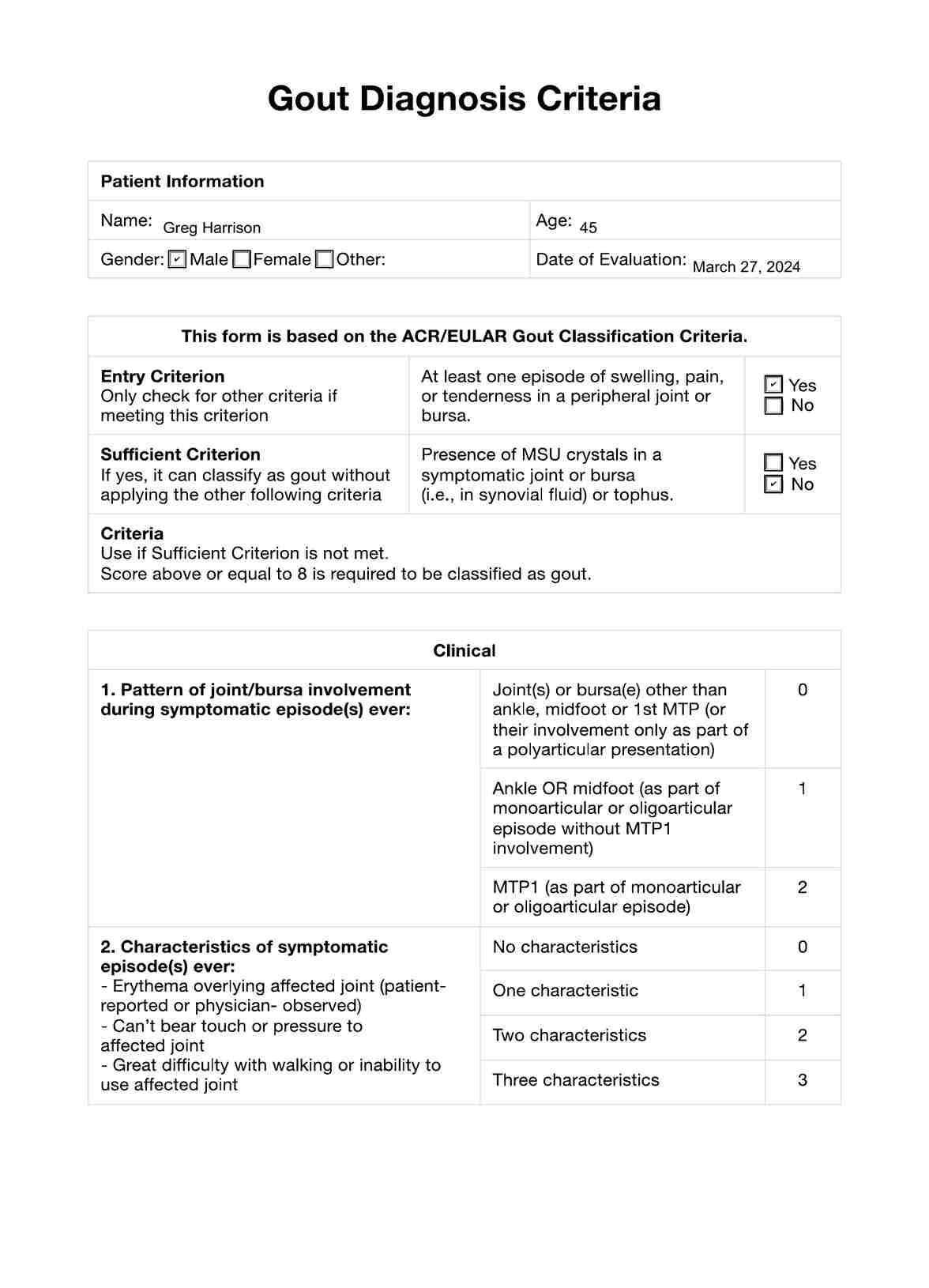
ACR/EULAR gout classification criteria
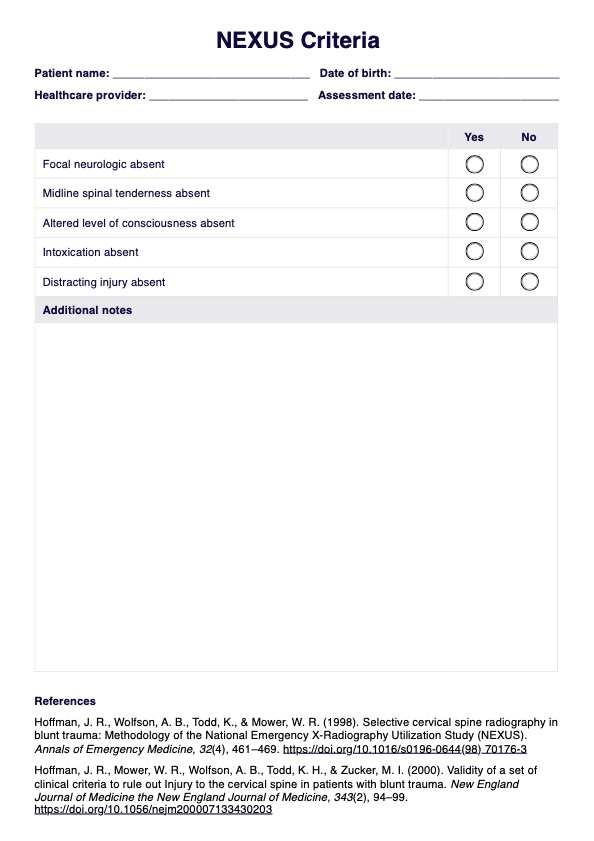
The ACR/EULAR criteria for gout classification are based on a scoring system that includes clinical, laboratory, and imaging findings, similar to the approach used in systemic sclerosis classification criteria. The criteria below are used when a patient meets the entry criterion of having at least one episode of swelling, pain, or tenderness in a peripheral joint or bursa. A score of 8 or more is classified as gout.
- Entry criterion: This is the preliminary criteria; the other criteria do not apply if this is not fulfilled. There should be at least one episode of swelling, pain, or tenderness in a peripheral joint or bursa.
- Sufficient criterion: Check if monosodium urate (MSU) crystals exist in a symptomatic joint or bursa (i.e., in synovial fluid) or tophus. If one of these is present, it can be classified as gout without applying further criteria.
Additional Criteria
These are used if the Sufficient Criterion is not met. Each has an associated score. A total score greater or equal to 8 is required for classification as gout.
Clinical
- Pattern of joint/bursa involvement during symptomatic episode(s):
- Joint(s) or bursa(e) other than ankle, midfoot, or 1st MTP: 0 points
- Ankle OR midfoot (as part of monoarticular or oligoarticular episode without MTP1 involvement): 1 point
- MTP1 (as part of monoarticular or oligoarticular episode): 2 points
- Characteristics of symptomatic episode(s):
- Erythema overlying affected joint: 1 point
- Can't bear touch or pressure to affected joint: 1 point
- Great difficulty with walking or inability to use affected joint: 1 point
- Time-course of episode(s):
- Presence of ≥2 typical episodes (time to maximal pain <24 hours, resolution of symptoms in ≤14 days, complete resolution between episodes): 2 points
- Clinical evidence of tophus: 4 points
Laboratory
- Serum urate concentration:
- <4 mg/dL: -4 points
- 4-<6 mg/dL: 0 points
- 6-<8 mg/dL: 2 points
- 8-<10 mg/dL: 3 points
- ≥10 mg/dL: 4 points
- Synovial fluid analysis:
- MSU negative: -2 points
Imaging
- Imaging evidence of urate deposition in symptomatic joint or bursa (ultrasound evidence of double-contour sign or DECT demonstrating urate deposition): 4 points
- Imaging evidence of gout-related joint damage (conventional radiography demonstrating at least one erosion): 4 points
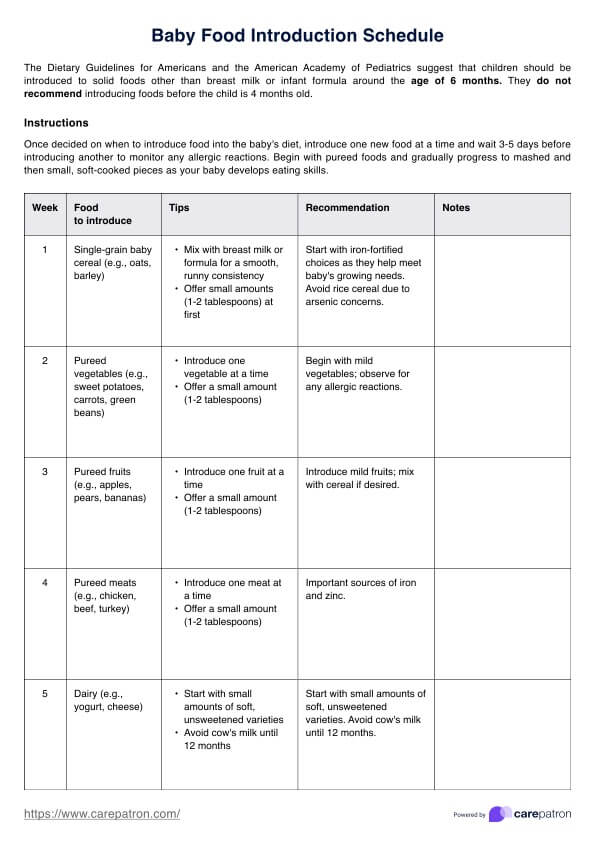
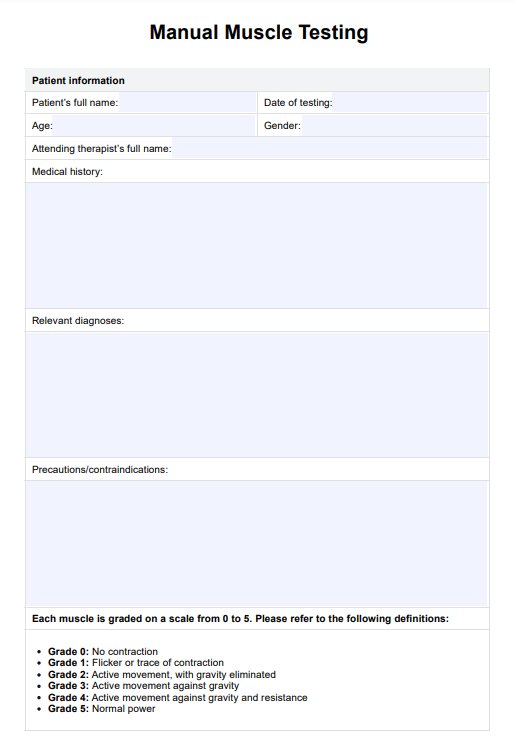
How to use our Gout Diagnosis Criteria template
The Gout Diagnosis Criteria template is based on the ACR/EULAR Gout Classification Criteria and is designed to assist healthcare professionals in diagnosing gout effectively. Here are the steps to follow:
Step 1: Access and explain the template
Download the Gout Diagnosis Criteria template from our platform and explain its purpose and structure to the patient. This helps in setting the right expectations and understanding the importance of the information being collected.
Step 2: Fill in patient information and evaluate clinical features
Enter the patient's basic information such as name, date of evaluation, gender, and age. Then, review and check the boxes corresponding to the clinical features the patient exhibits, including the pattern of joint involvement and characteristics of symptomatic episodes.
Step 3: Record laboratory and imaging test results
Input the results of laboratory tests, particularly the serum urate concentration, and assess any imaging findings for evidence of urate deposition and gout-related joint damage.
Step 4: Confirm diagnosis
Based on the ACR/EULAR criteria and the total score, determine whether the patient can be classified as having gout. Record any additional notes that may assist in the patient's treatment plan.
Gout treatments
Treatment for gout aims to alleviate pain during acute attacks and prevent future attacks and complications, such as the development of tophi and kidney stones. Here are some common professional and home gout treatments, as well as some ways to manage it:
Medications for acute attacks
To quickly manage the pain and inflammation of an acute gout attack, healthcare professionals often prescribe the following medications:
- Nonsteroidal anti-inflammatory drugs (NSAIDs): These are often the first line of treatment to reduce inflammation and pain during an acute gout attack.
- Colchicine: This medication is effective in reducing gout pain and is usually used if NSAIDs are contraindicated.
- Corticosteroids: These can be taken orally or injected into the affected joint to quickly reduce inflammation and pain.
Medications to prevent future attacks
To reduce the frequency of gout attacks and prevent complications, long-term medications are often prescribed:
- Urate-lowering therapy (ULT): Drugs like allopurinol and febuxostat are used to lower the levels of uric acid in the blood, preventing the formation of urate crystals.
- Probenecid: This uricosuric drug helps the kidneys excrete more uric acid, reducing the risk of gout attacks.
Lifestyle modifications
Making lifestyle changes can significantly reduce the risk of gout attacks and improve overall health:
- Dietary changes: Avoiding foods high in purines, such as red meat, organ meats, and certain types of seafood, can help reduce the risk of gout attacks.
- Weight management: Maintaining a healthy weight can reduce the risk of gout and its complications.
Home treatments
In addition to professional treatments, there are simple home remedies that can provide relief during a gout attack.
- Cold compresses: Applying ice packs to the affected joint can help reduce inflammation and alleviate pain during an acute gout attack.
- Hydration: Drinking plenty of water can help flush uric acid from the body, reducing the risk of crystal formation.
In addition to these treatments, it's important for patients to avoid alcohol and sugary drinks, which can trigger gout attacks. Regular follow-up with a healthcare professional is essential to monitor the effectiveness of the treatment plan and make necessary adjustments.
Commonly asked questions
Gout diagnosis is confirmed through a combination of clinical evaluation, laboratory tests (such as serum urate levels), and imaging studies (like ultrasound or X-ray) to detect urate crystals or joint damage.
The most reliable diagnostic indicator of gout is the presence of monosodium urate (MSU) crystals in the synovial fluid of a symptomatic joint or in a tophus, as observed under a microscope.
The gold standard for diagnosing gout is the identification of monosodium urate crystals in synovial fluid or tophaceous material using polarized light microscopy.