A cut-off score of 25 on the FAB scale indicates an increased risk of falls in older adults. Scores below this threshold suggest the need for fall prevention strategies and further evaluation.
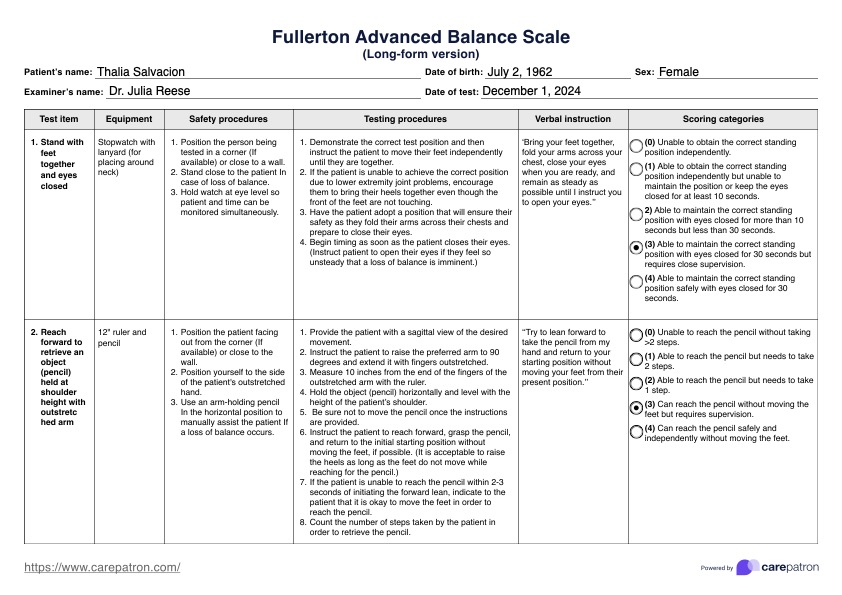
Fullerton Advanced Balance (FAB) Scale
Use the Fullerton Advanced Balance (FAB) Scale to evaluate balance in functionally independent older adults. Get this free fillable template here.
Fullerton Advanced Balance (FAB) Scale Template
Commonly asked questions
The FAB scale assessment typically takes 10 to 20 minutes to complete, making it a practical tool for evaluating balance during routine clinical visits.
A functional balance assessment is essential for older adults who live independently because it helps spot balance issues that might lead to falls. Good balance is critical to staying active and healthy, which supports their independence and keeps them healthy, functioning adults. This assessment lets healthcare providers recommend ways to improve stability, helping older adults stay safe and confident in their daily lives.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











