ECG 12-Lead Test
Discover the intricacies of the ECG 12-Lead Test, its significance, and its interpretation in our comprehensive guide. Learn more now!


What is an ECG 12-Lead Test, and what does it measure?
An ECG 12-lead test is a non-invasive procedure used to measure the heart's electrical activity. It involves attaching electrode patches to specific points on the body, including the limbs and chest. This test is crucial in diagnosing various heart conditions, including myocardial infarction (heart attack), irregular heartbeats, and heart disease.
By placing electrodes in proper positions, such as on the chest along the front midclavicular line and anterior axillary lines and on the limbs, the heart's electrical signals can be recorded from different angles, aiding in accurate interpretation.
During the ECG, leads and electrodes monitor the heart's electrical signals, including atrial activation and ventricular depolarization, which are crucial for determining heart rhythm and detecting abnormalities. The test is often painless and requires the patient to lie bare-chested while the electrode's limb leads are attached. The ECG machine records the electrical activity, displaying it as a graph or diagram for interpretation by a healthcare professional.
The results of the ECG can indicate irregular rhythms, such as atrial fibrillation or Brugada syndrome, as well as other abnormalities like electrolyte imbalances or signs of a heart attack. It's also helpful in assessing the QT interval, PR interval, and T wave, which provide further insights into cardiac health. Additionally, ECG readings can be compared to standard values charts, considering factors such as age, sex, and family history.
In some cases, continuous ECG monitoring may be necessary, mainly if symptoms are intermittent or need ongoing assessment. After the test, patients may be given a subsequent appointment to discuss the results with their doctor and determine any necessary actions or treatments. An ECG 12-lead test is essential in evaluating heart conditions and guiding appropriate medical interventions.
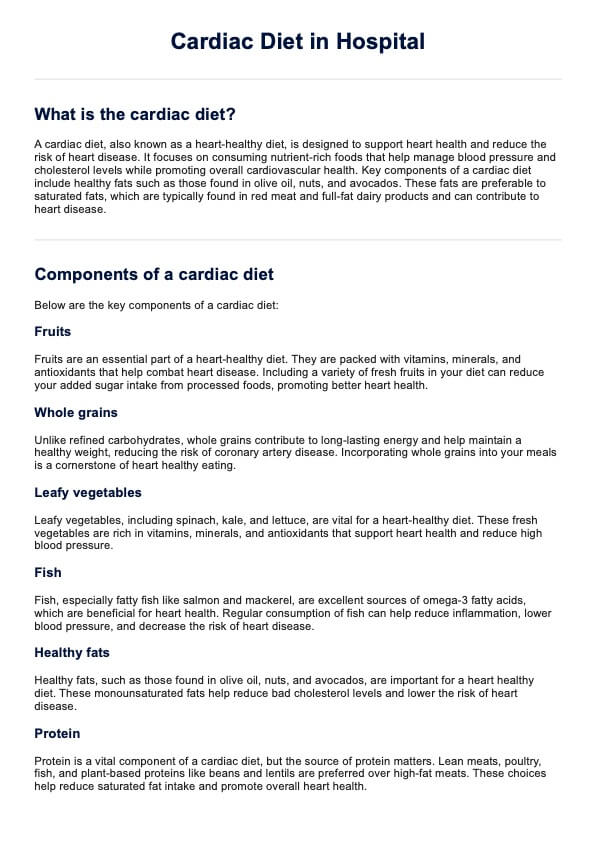
ECG 12-Lead Test Template
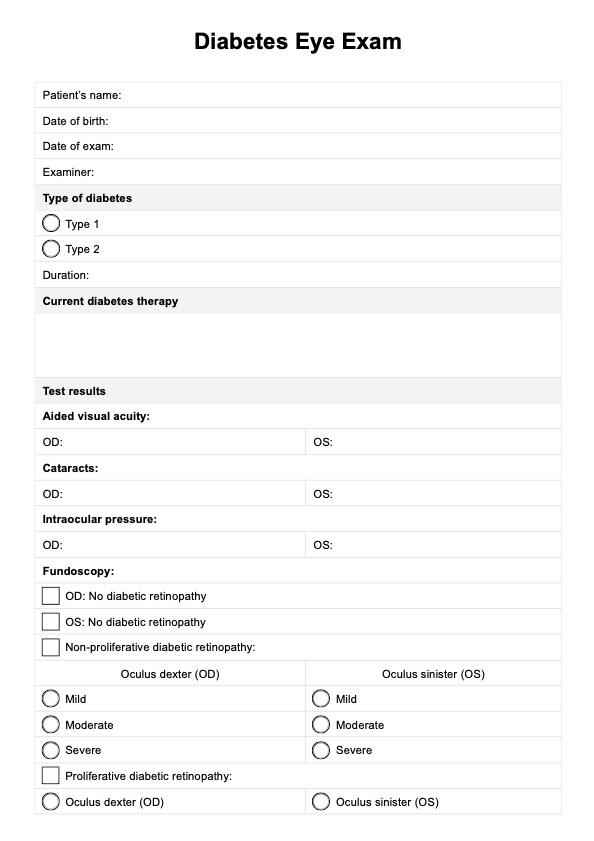
ECG 12-Lead Test Example
How is a 12-lead ECG Test conducted?
A 12-lead ECG test is typically conducted as follows:
- Preparation: The patient is asked to remove any clothing from the waist and lie comfortably on an examination table or bed. Sometimes, a patient may be asked to wear a hospital gown. It's essential to ensure that the chest area is accessible.
- Electrode placement: The skin is cleaned with alcohol wipes before electrode patches are attached to specific points on the body. The limbs and chest are the areas where the patches are placed in a particular pattern to capture the heart's electrical activity from different angles.
- Lead placement: The 12-Lead ECG consists of 10 electrodes in specific positions. Six electrodes are placed on the chest to capture the heart's electrical activity from different angles. The remaining four electrodes are placed on the limbs.
- Recording: The ECG machine records the heart's electrical signals onto a strip of graph paper or digital display. The patient is asked to remain still and breathe normally during the process.
- Analysis: Healthcare providers, usually physicians or cardiologists, analyze ECG data after recording to interpret the results and identify abnormalities in the heart's electrical activity, such as irregular rhythms, ischemia, or other cardiac conditions.
- Documentation: The findings of the ECG test are documented in the patient's medical record. Further diagnostic tests or treatments may be recommended if abnormalities are detected based on the results.
- Post-test: Once the ECG is complete and the results have been interpreted, the electrodes are removed from the patient's skin. The patient can then typically resume normal activities.
Ordering an ECG 12-Lead Test main indications
An ECG 12-Lead test may be ordered for various indications, including but not limited to:
- Chest pain: One of the most common reasons for ordering a 12-Lead ECG is to evaluate chest pain or discomfort. It helps determine whether the pain is due to a cardiac issue, such as a heart attack or angina.
- Suspected heart attack (myocardial infarction): If a patient presents with symptoms suggestive of a heart attack, such as chest pain, shortness of breath, nausea, or sweating, an ECG can help confirm the diagnosis by showing characteristic changes in the heart's electrical activity.
- Evaluation of irregular heart rhythms (arrhythmias): ECGs are crucial for diagnosing and evaluating various types of irregular heart rhythms, such as atrial fibrillation, atrial flutter, ventricular tachycardia, or bradycardia.
- Assessment of cardiac symptoms: Patients with palpitations, dizziness, fainting, or syncope may undergo a 12-Lead ECG to assess their heart's electrical activity and detect any underlying arrhythmias or conduction abnormalities.
- Monitoring heart health: Individuals with known heart conditions or risk factors for heart disease, such as hypertension, diabetes, hyperlipidemia, or a family history of heart disease, may undergo regular ECG testing as part of their cardiovascular evaluation and monitoring.
- Preoperative evaluation: Patients may require an ECG to assess their cardiac function and identify potential risks before undergoing certain surgeries, especially those involving anesthesia or cardiac stress.
- Screening for cardiac abnormalities: ECG screening may be performed in specific populations, such as athletes or individuals with a history of sudden cardiac death in the family, to detect underlying cardiac abnormalities, including inherited arrhythmias or structural heart diseases.
- Assessment of symptoms related to cardiac medications: Patients experiencing symptoms potentially associated with cardiac medications, such as chest pain, palpitations, or shortness of breath, may undergo an ECG to evaluate the effects of the drug on their heart rhythm and function.
How long does it take to complete an ECG 12-Lead Test?
A 12-Lead ECG test typically ranges from 5 to 10 minutes. However, it can vary depending on factors such as the patient's cooperation, the complexity of electrode placement, and the need for repeat testing due to technical issues or poor signal quality.
How to use the ECG 12-Lead Test template?
Using an ECG 12-Lead Test template can help ensure consistency and accuracy in documenting and interpreting electrocardiogram results. Here's a general guide on how to use such a template:
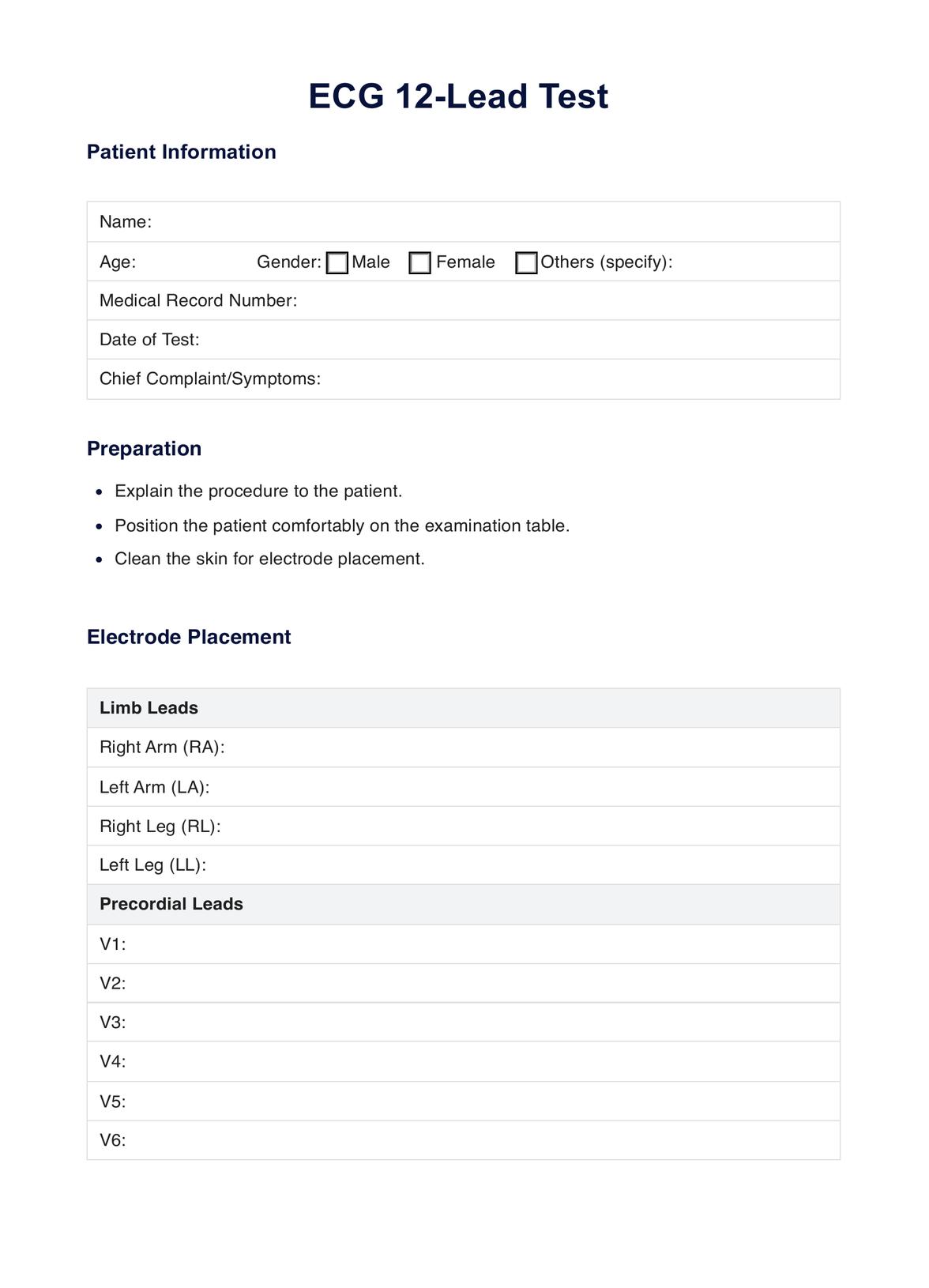
- Patient information: Start by filling in the patient's demographic information, including their name, date of birth, medical record number, and any relevant medical history or risk factors.
- Preparation: Document any preparations before conducting the ECG, such as explaining the procedure to the patient, positioning them on the examination table, and cleaning the skin for electrode placement.
- Electrode placement: Use the template to indicate the placement of electrodes on the patient's body. This may include specific diagrams or descriptions for placing electrodes on the limbs (arms and legs) and chest (precordial leads).
- Interpretation: Use the template to document the understanding of the ECG results, including identifying each waveform (P wave, QRS complex, T wave) and evaluating the heart rate, rhythm, intervals (PR, QT), and presence of abnormalities.
- Clinical implications: Describe the clinical impact of the ECG findings, including any suspected diagnoses, recommended further evaluation or testing, and potential treatment interventions.
- Documentation: Complete the template by documenting the findings and interpretations in the patient's medical record, ensuring accuracy and clarity for future reference.
- Follow-up: If necessary, outline any follow-up actions or recommendations based on the ECG results, such as scheduling additional tests, referring the patient to a specialist, or adjusting their treatment plan.
- Review and signature: Review the completed template for accuracy and completeness before signing and dating it to confirm that the ECG was performed and interpreted correctly.
A standardized ECG 12-Lead Test template can streamline documentation and facilitate communication between healthcare providers, ensuring comprehensive and consistent care for patients undergoing electrocardiographic evaluation.
Common abnormalities and conditions detected using an ECG 12-Lead Test
An ECG 12-Lead Test can detect various abnormalities and conditions related to the heart's electrical activity and function. Some common abnormalities and conditions include:
- Arrhythmias: Irregular heart rhythms, such as atrial fibrillation, atrial flutter, ventricular tachycardia, and bradycardia, can be identified on the ECG.
- Myocardial infarction (heart attack): Changes in the ST segment and T wave on the ECG can indicate myocardial ischemia or injury, suggesting a heart attack.
- Ischemic heart disease: ECG findings such as ST-segment depression, T-wave inversion, or development of pathological Q waves can indicate myocardial ischemia, which may be indicative of underlying coronary artery disease.
- Conduction abnormalities: ECG can detect conduction abnormalities such as atrioventricular (AV) blocks, bundle branch blocks, and fascicular blocks, which affect the expected propagation of electrical impulses through the heart.
- Cardiomyopathies: Changes in the ECG pattern, such as increased QRS voltage or nonspecific ST-T wave changes, may suggest underlying cardiomyopathies, including hypertrophic cardiomyopathy, dilated cardiomyopathy, or restrictive cardiomyopathy.
- Electrolyte imbalances: Abnormalities in serum electrolyte levels, such as hyperkalemia or hypokalemia, can manifest as specific changes on the ECG, such as peaked T waves or flattened T waves, respectively.
- Pericarditis: ECG findings such as widespread ST-segment elevation with PR segment depression (diffuse concave upward ST-segment elevation) are characteristic of acute pericarditis.
- Pulmonary embolism: In cases of acute pulmonary embolism, ECG findings may include sinus tachycardia, S1Q3T3 pattern (prominent S wave in lead I, Q wave, and inverted T wave in lead III), and right heart strain patterns (such as T wave inversion in suitable precordial leads).
- Electrophysiological disorders: ECG can detect inherited arrhythmia syndromes such as Brugada syndrome, long QT syndrome, and Wolff-Parkinson-White syndrome, which are associated with specific ECG patterns.
These are just a few examples of the many abnormalities and conditions that can be detected using an ECG 12-Lead Test. Interpretation of the ECG findings requires careful analysis by a trained healthcare professional to accurately diagnose and manage the underlying cardiac condition.
Can medications or medical conditions affect the results of an ECG 12-Lead Test?
Yes, medications and medical conditions can affect the results of an ECG 12-Lead Test. Certain medications, such as those that affect heart rate or rhythm (e.g., beta-blockers, calcium channel blockers, antiarrhythmics), can alter the appearance of the ECG waveform.
Also, medical conditions such as electrolyte imbalances (e.g., hyperkalemia, hypokalemia), cardiac hypertrophy, myocardial ischemia, and structural heart diseases can influence ECG findings. Healthcare professionals must consider the patient's medication history and medical conditions when interpreting ECG results to ensure accurate diagnosis and appropriate management.
Commonly asked questions
Yes, improper electrode placement can significantly impact the accuracy of ECG results. Incorrect placement can distort the recorded electrical signals, leading to misinterpretation of the ECG and potentially missing critical cardiac abnormalities.
A 12-lead ECG comprehensively assesses the heart's electrical activity, allowing healthcare professionals to detect cardiac abnormalities, including arrhythmias, conduction disturbances, ischemia, and infarction.
While a 12-lead ECG is valuable for detecting cardiac abnormalities, it does not provide direct information about the heart's structure or function. Additional imaging tests such as echocardiography or cardiac MRI may be needed to assess cardiac anatomy and function more comprehensively.