Dysphagia Care Plan
Optimize patient outcomes with our free Dysphagia Care Plan template. Streamline care delivery for individuals with swallowing difficulties.


What is dysphagia?
Dysphagia refers to impaired swallowing, making it challenging for individuals to move food or liquids from their mouth to their stomach. This condition can result from various causes, such as neurological disorders, stroke, or throat injuries, and can range from mild discomfort to a complete inability to swallow. Individuals with dysphagia often face aspiration risk, where food or liquid mistakenly enters the lungs, leading to serious complications and risk of aspiration pneumonia.
A care plan for dysphagia is essential for managing these swallowing difficulties and preventing complications. This may include an impaired swallowing care plan and dysphagia management, which focuses on techniques to improve swallowing safety. Key nursing interventions include ensuring the patient eats slowly, using specialized utensils, and positioning the individual properly during meals.
Dysphagia management aims to reduce the risk of aspiration and provide long-term care, such as exercises and modified diets. A nursing care plan for dysphagia often outlines steps for monitoring the patient’s progress and ensuring safe eating habits. Identifying impaired swallowing related issues helps healthcare teams, like a speech language pathologist, take preventive actions and support patients with effective treatments tailored to their condition.
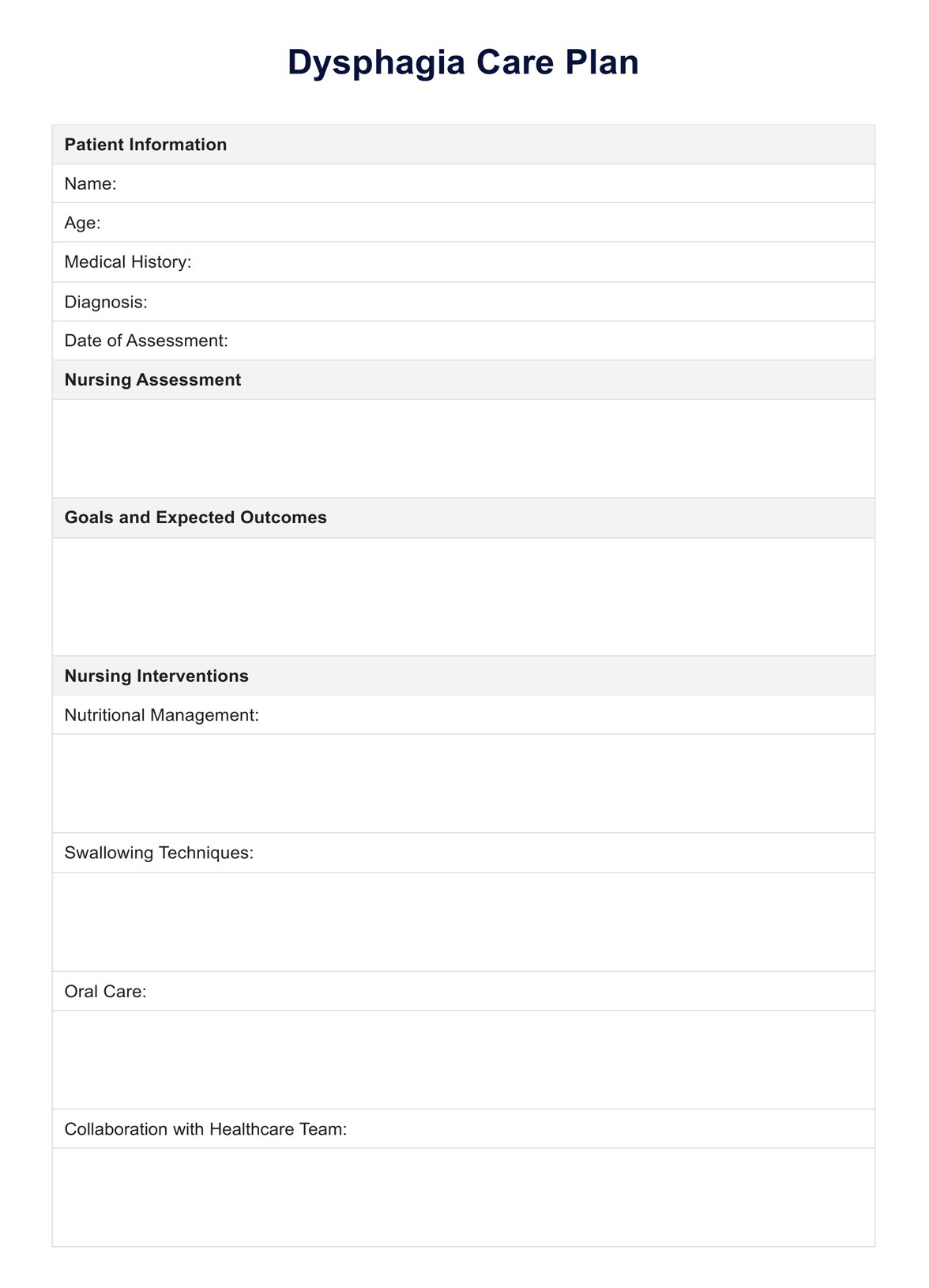
Dysphagia Care Plan Template
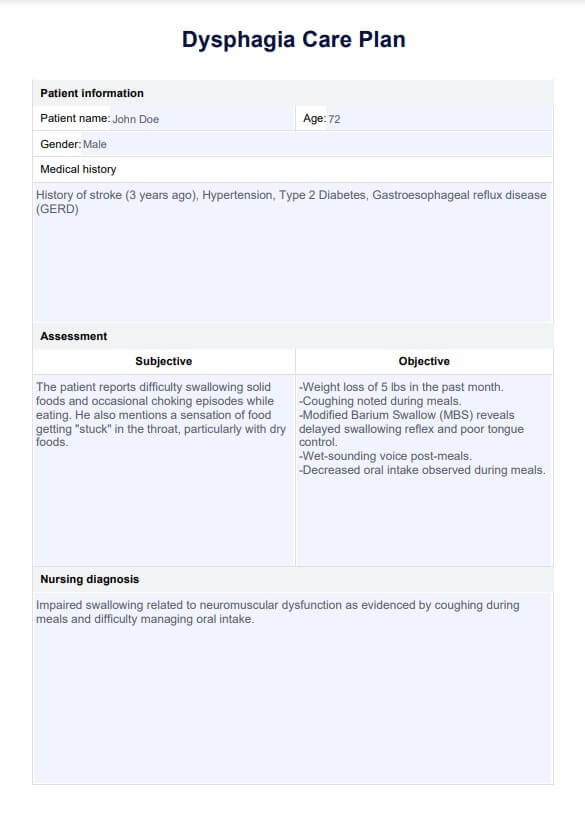
Dysphagia Care Plan Example
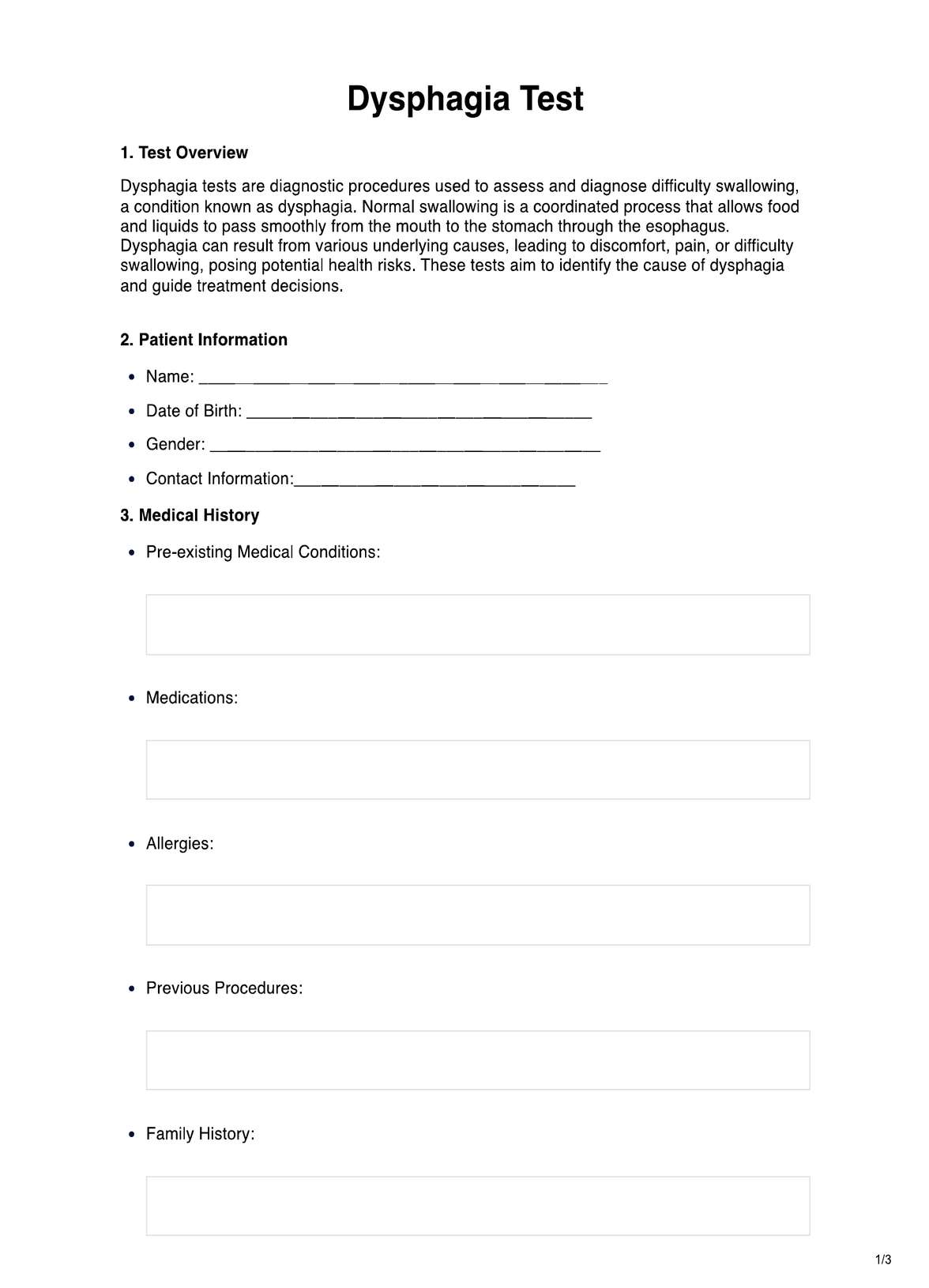
What is included in a Dysphagia Care Plan?
A Dysphagia Care Plan is a comprehensive framework designed to address the unique needs of individuals experiencing swallowing difficulties. It outlines personalized strategies to manage symptoms, improve safety during meals, and enhance the quality of life while minimizing the risk of aspiration and related complications. Here are the key components of a Dysphagia Care Plan:
Patient information
This section includes essential details about the patient, such as their medical history, current medications, and any previous incidents of aspiration pneumonia or respiratory complications. Understanding the patient’s background helps tailor the dysphagia treatment to their specific needs.
Initial nursing assessment and diagnosis
A thorough evaluation by a healthcare professional, often including a clinical swallowing evaluation and a swallowing evaluation by a speech-language pathologist. This assessment identifies the level of swallowing impairment and the specific facial muscles affected, guiding subsequent interventions.
Goals and outcomes
Goals and outcomes define the desired results of the care plan, such as improving oral intake, minimizing aspiration risk, or increasing independence in feeding. These goals should be realistic and measurable to track progress and modify interventions if necessary.
Nursing interventions and rationale
Based on the initial assessment, specific interventions are selected to address the patient’s swallowing difficulties. These may include modifying food and liquid textures, using adaptive feeding equipment, implementing safe swallowing techniques, and providing education and training to the patient and caregivers. The rationale for each intervention should be clearly stated.
Evaluation
Regular evaluation and reassessment are critical to monitor the patient’s progress and make necessary modifications to the care plan. This may involve reevaluating swallowing function, adjusting food and liquid textures, or providing additional education to patients and caregivers.
Symptoms of dysphagia
Dysphagia, can present with various symptoms that may affect a person's ability to eat slowly and drink safely. Early identification of these signs is critical for effective nursing care and reducing the risk for aspiration. A thorough nursing assessment is essential to identify these symptoms and promote safe swallowing practices.
Below are common symptoms of dysphagia:
- Difficulty swallowing solid foods or liquids
- Pain while swallowing (odynophagia)
- Choking or coughing during meals
- Feeling like food is stuck in the throat or chest
- Frequent gag reflex or regurgitation
- Needing to chew food for an extended time before swallowing
- Hoarse voice or sore throat after eating
- Difficulty taking oral medications
- Unintentional weight loss due to reduced intake
- Recurrent respiratory infections due to aspiration
Causes of dysphagia
Dysphagia can arise from a variety of underlying conditions, affecting the ability to swallow and leading to swallowing impairment. Identifying the root cause is crucial for effective dysphagia management and creating a tailored care plan to address the patient's specific needs. The following are common causes of difficulty swallowing:
- Neurological disorders such as stroke, Parkinson’s disease, or multiple sclerosis
- Muscular diseases, including muscular dystrophy or myasthenia gravis
- Structural abnormalities in the throat or esophagus, such as strictures or tumors
- Endotracheal or tracheostomy tubes, which may cause temporary or permanent swallowing issues
- Delayed gastric emptying or gastroesophageal reflux disease (GERD)
- Weak or uncoordinated swallowing reflex
- Long-term mechanical ventilation
- Side effects from certain medications that impact swallowing
- Post-surgical complications involving the throat or esophagus
- Fatigue and lack of adequate rest periods between meals
- Poor oral care leading to infections or inflammation of the mouth or throat
Types of dysphagia
According to Wolf (1990), dysphagia is categorized into four primary types based on the location of the swallowing problem: oropharyngeal, esophageal, esophagogastric, and paraesophageal.
Oropharyngeal dysphagia
Oropharyngeal dysphagia occurs when there is difficulty moving the food bolus from the oral cavity to the cervical esophagus. It results from either abnormal motility of the oropharynx or physical impairment to passage (obstruction). Symptoms include the sensation of food sticking in the oral cavity or neck region, as well as pulmonary aspiration.
Esophageal dysphagia
Esophageal dysphagia occurs when there is difficulty with the passage of solid or liquid material through the esophagus, specifically the region between the upper and lower esophageal sphincters. It results from either abnormal motility of this segment of the esophagus or physical impairment to passage (obstruction).
Esophagogastric dysphagia
Esophagogastric dysphagia occurs when there is impairment of passage of material from the lower esophageal sphincter into the gastric fundus due to motor or physical obstruction. Causes include abnormalities of the lower esophageal sphincter, benign or malignant strictures of the distal esophagus, and mass lesions of the gastric cardia.
Paraesophageal dysphagia
Paraesophageal dysphagia occurs when there is either physical impingement on the esophageal wall and lumen or infiltration of the esophageal wall leading to obstruction. If extensive, this may have secondary motor effects on the esophagus.
References
Wolf, D. C. (1990). Dysphagia (H. K. Walker, W. D. Hall, & J. W. Hurst, Eds.). PubMed; Butterworths. https://www.ncbi.nlm.nih.gov/books/NBK408/#:~:text=Dysphagia%20can%20be%20classified%20into
Commonly asked questions
The dysphagia care plan aims to improve impaired swallowing related to function, maintain adequate nutrition, prevent aspiration pneumonia, and enhance the patient's overall quality of life.
Interventions for dysphagia include modifying diet texture, implementing swallowing techniques, providing oral care, coordinating with other healthcare professionals, and monitoring the patient's progress.
The four stages of dysphagia are the oral preparatory phase, the oral phase, the oral cavity, the pharyngeal phase, and the esophageal phase. These stages represent the events involved in swallowing, from chewing and forming a bolus to passage through the throat and into the esophagus.