DKA Nursing Care Plan
Create an effective diabetic ketoacidosis nursing care plan with this guide and our PDF template.


What is diabetic ketoacidosis (DKA)?
Diabetic ketoacidosis (DKA) is a critical and life-threatening complication associated with diabetes mellitus, especially type 1 diabetes. It occurs due to a severe insulin deficiency, causing the body to break down fat for energy. This process produces ketones, which lead to metabolic acidosis as they accumulate in the blood. Elevated blood glucose levels, dehydration, and electrolyte imbalances mark DKA.
Key symptoms and management of diabetic ketoacidosis
Key symptoms of diabetic ketoacidosis include excessive thirst, frequent urination, nausea, vomiting, abdominal pain, fruity-smelling breath, confusion, and, in severe cases, unconsciousness. Complications such as cerebral edema, unstable blood glucose, and acute kidney injury may arise, requiring immediate medical intervention.
To stabilize patients and address metabolic acidosis, it is crucial to monitor vital signs, including blood pressure, along with fluid and electrolyte balance. Administering intravenous fluids helps restore fluid volume, while regular checks of arterial blood gas, serum glucose, and other parameters guide treatment. Interventions like adjusting therapy to lower blood glucose levels and administering insulin are essential to improving outcomes and preventing further harm.
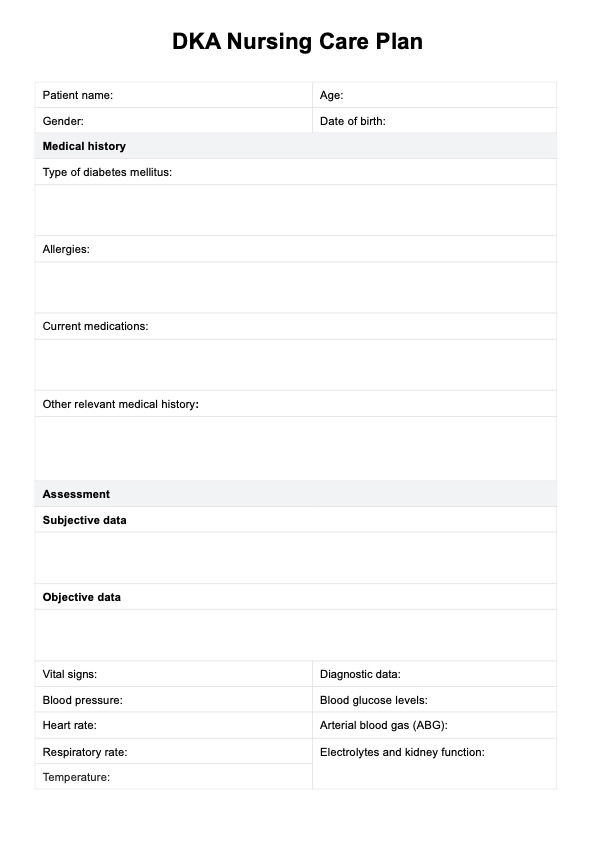
DKA Nursing Care Plan Template
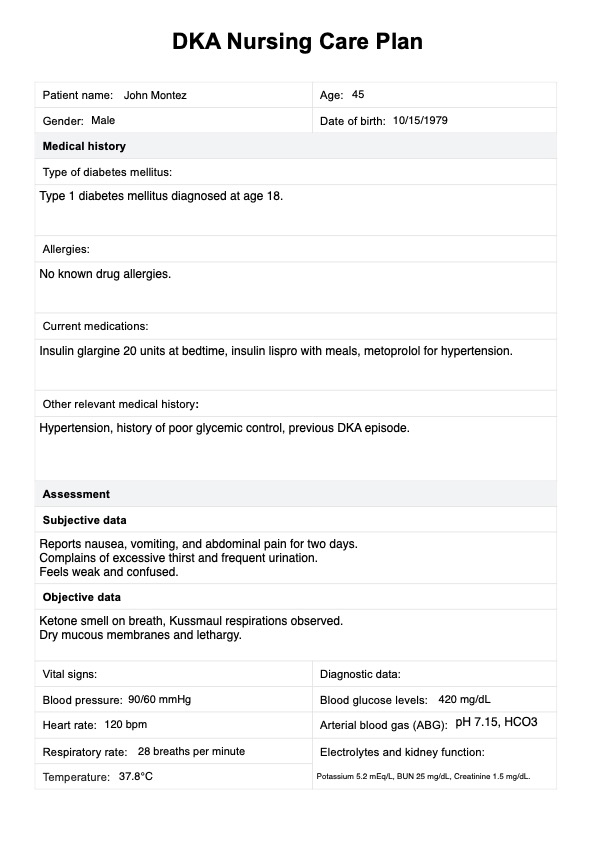
DKA Nursing Care Plan Example
How does our DKA Nursing Care Plan Template work?
A DKA nursing care plan ensures timely interventions and continuous monitoring of blood glucose levels, blood urea nitrogen, and vital signs to manage diabetic ketoacidosis effectively. It addresses critical complications like dehydration, metabolic acidosis, and cerebral edema while guiding insulin therapy and electrolyte management.
By following these steps, you can use the DKA Nursing Care Plan Template to provide effective and structured care to patients:
Step 1: Download the template
Access the DKA Nursing Care Plan Template from the Carepatron platform by clicking "Use template". You can also click on "Download" to get a fillable PDF copy. This template provides a structured format to document patient information, assessment data, diagnoses, goals, interventions, and evaluations, ensuring comprehensive care for DKA patients.
Step 2: Fill in patient information
Enter the patient’s basic information in the designated sections. Also, record their medical history, including the diagnosis of DKA, type of diabetes mellitus, allergies, current medications, and any relevant past medical history.
Step 3: Conduct the assessment
Gather both subjective and objective data. For subjective data, note the patient's symptoms and complaints, such as excessive thirst, nausea, or confusion. Under objective data, monitor and document vital signs (e.g., blood pressure, heart rate, respiratory rate, and temperature), blood glucose level, arterial blood gas (ABG) results, and electrolytes and kidney function.
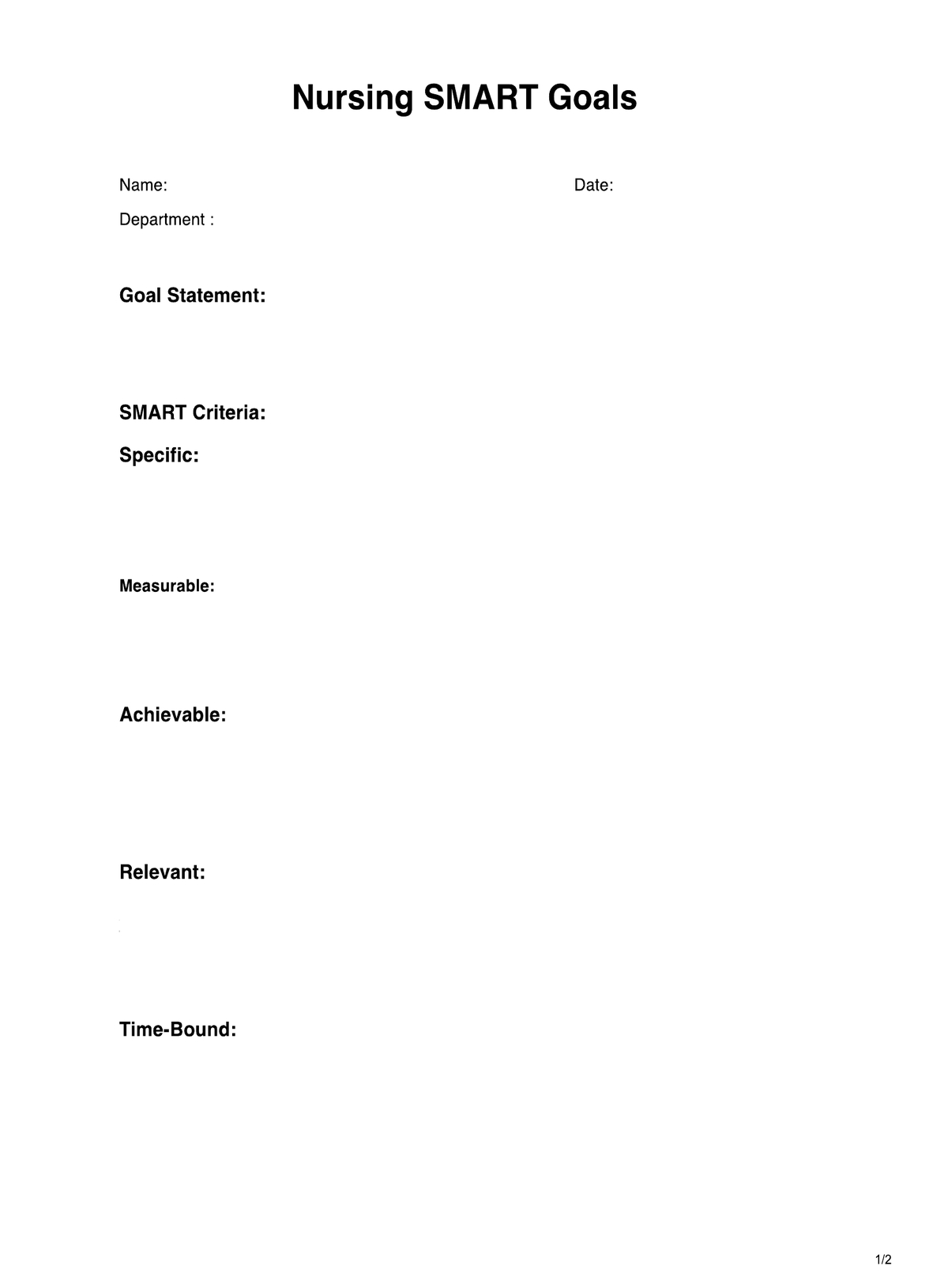
Step 4: Document the nursing diagnosis, goals, and interventions
Based on the assessment, create a nursing diagnosis (e.g., imbalanced fluid volume) and set specific goals (e.g., stabilize blood glucose levels). Identify key interventions such as administering intravenous fluids, insulin therapy, and educating the patient. Ensure you document the rationale for each intervention to clarify its importance in the patient's care plan.
Step 5: Evaluate the patient’s progress
Regularly evaluate the effectiveness of the interventions. Check if blood glucose levels are stabilized, ABG results are normalized, and the patient is rehydrated with stable vital signs. Address any complications and ensure timely interventions for positive outcomes.
When would you use this template?
A DKA nursing care plan is implemented when caring for individuals diagnosed with DKA, typically in hospital or acute care settings. The nursing care plan for DKA may be used in the following situations:
Emergency department admissions
Patients presenting with symptoms of DKA, such as high blood sugar, ketones in urine or blood, dehydration, altered mental status, and abdominal pain, often require immediate medical attention. Nursing care plans are crucial in managing these patients upon admission to the emergency department.
Inpatient hospital care
Individuals admitted to the hospital due to DKA or its complications need close monitoring and management. Nursing care plans help to guide ongoing care, including fluid and electrolyte management, insulin therapy, vital sign monitoring, and assessment for complications.
Patients with known diabetes
Patients with a history of diabetes, particularly type 1 diabetes, who might develop DKA due to illness, infection, inadequate insulin administration, or other triggers require vigilant monitoring. They may benefit from a proactive nursing care plan to prevent DKA episodes.
Pediatric cases
DKA can be particularly critical in pediatric patients. Nursing care plans are essential in managing children with DKA, as they might exhibit different symptoms and require specialized care to prevent complications like cerebral edema.
Home care and education
After acute treatment, individuals recovering from DKA may require ongoing monitoring and education to manage their condition at home. Nursing care plans include educating patients and their families on insulin administration, monitoring blood glucose levels, recognizing warning signs, and adhering to dietary recommendations.
Benefits of using the DKA Nursing Care Plan Template
Using the DKA Nursing Care Plan Template offers numerous advantages for managing patients with diabetic ketoacidosis (DKA). Here are the key benefits:
Comprehensive monitoring and documentation
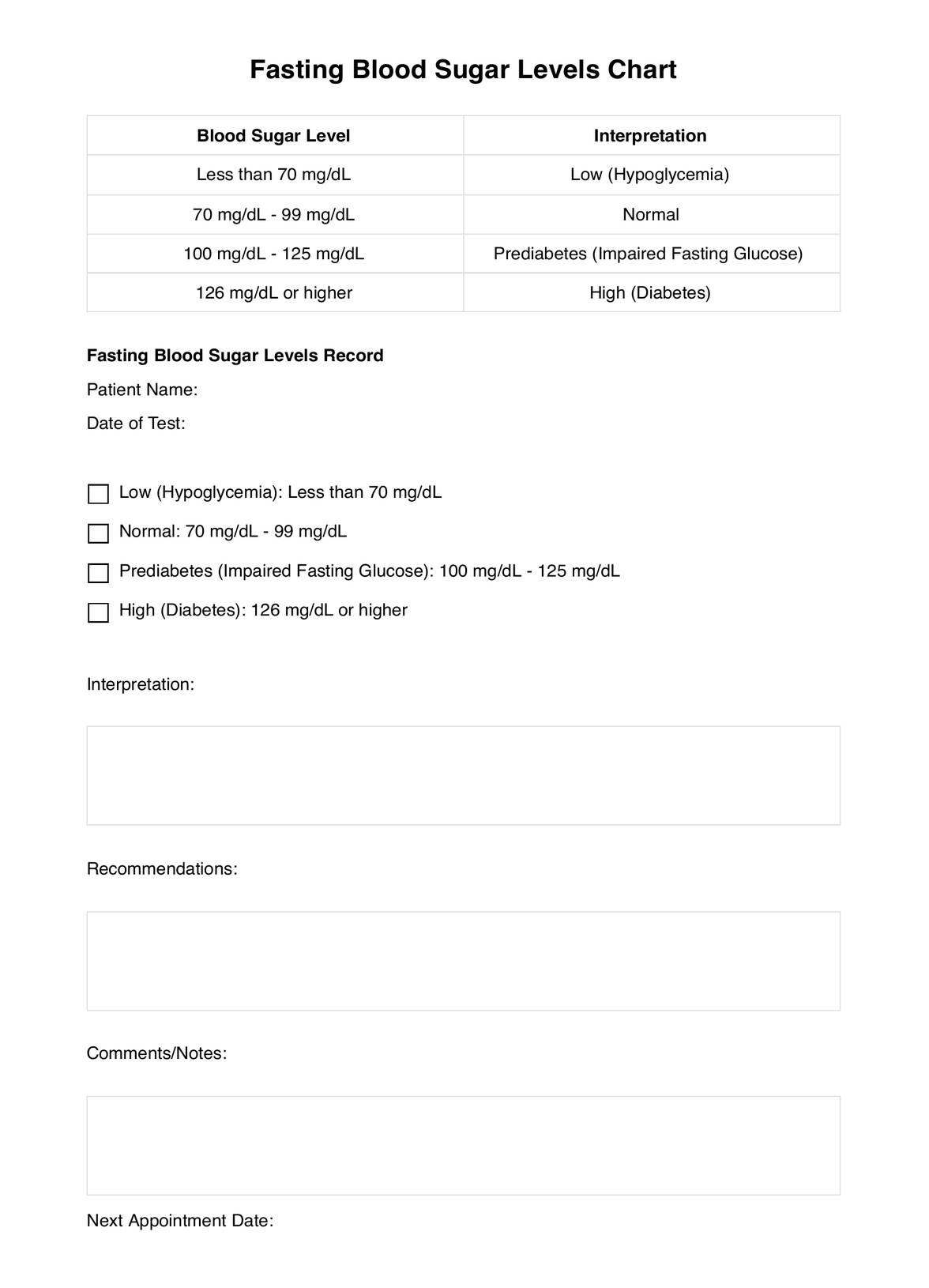
The template helps ensure regular blood glucose monitoring and monitoring blood glucose levels throughout treatment. This allows for accurate tracking of blood sugars, glucose levels, and the effectiveness of insulin injections or insulin doses.
Enhanced fluid and electrolyte management
By closely tracking fluid balance, fluid resuscitation, and electrolyte balance, the template helps prevent electrolyte imbalances and manage electrolyte levels. It ensures timely intervention to correct fluid overload or decreased blood pressure and provides a structured approach to maintaining fluid intake and urine output.
Improved diabetes management
The template supports the management of insulin deficiency by assisting healthcare providers in administering insulin therapy and injections as needed. It also aids in glycemic control by adjusting insulin therapy to normalize blood glucose levels and lower blood glucose when necessary.
Thorough assessment of risk factors
The template includes sections that allow for thorough documentation of risk factors such as urine ketones, osmotic diuresis, and insulin deficiency, helping to identify potential complications like cardiac arrhythmias, urinary tract infections, or acute renal failure.
Timely intervention and education
It guides nurses in providing appropriate nursing interventions, including administering medications and insulin therapy, to address potential complications like low blood pressure, decreased blood pressure, and potassium levels. The template also emphasizes the importance of educating patients about recognizing symptoms of DKA and adhering to diabetes management practices, thus improving overall patient outcomes.
Commonly asked questions
It's essential to monitor blood glucose levels frequently, especially during the initial phase of treatment, to assess the effectiveness of insulin therapy and ensure glucose levels are stabilizing. Typically, blood glucose levels should be checked every 1-2 hours until stabilized.
The key steps include administering insulin therapy, administering medications as prescribed, and closely monitoring vital signs such as blood pressure, heart rate, and respiratory rate. This helps assess the patient’s response to treatment and detect any complications early.
Patient education should focus on the importance of monitoring blood glucose levels, administering insulin therapy as prescribed, and recognizing signs of complications. Teaching patients about maintaining hydration and proper medication adherence is also crucial for effective diabetes management.