Diverticulitis Test
Explore our comprehensive Diverticulitis Test for accurate diagnosis. Quick, reliable results to guide your path to digestive health.


Diverticulitis and its early detection importance
Abdominal pain, especially on the lower left side, can be unsettling. But, your doctor may consider diverticulitis possible if you have a history of digestive issues. This inflammation of pouches in your colon can be uncomfortable, but early detection is vital to effective management and preventing severe complications.
Why is early detection so important? Imagine faster relief from symptoms like pain and changes in bowel habits. Think about avoiding unnecessary tests and procedures by differentiating diverticulitis from other conditions early on. Most importantly, picture yourself empowered to work with your doctor on a personalized plan and make informed lifestyle changes to manage your gut health long-term.
Don't wait for discomfort to take control. If you experience potential symptoms, talk to your doctor. Early detection can make a significant difference in managing chronic diverticulitis more effectively and keeping you on track for a healthier you!
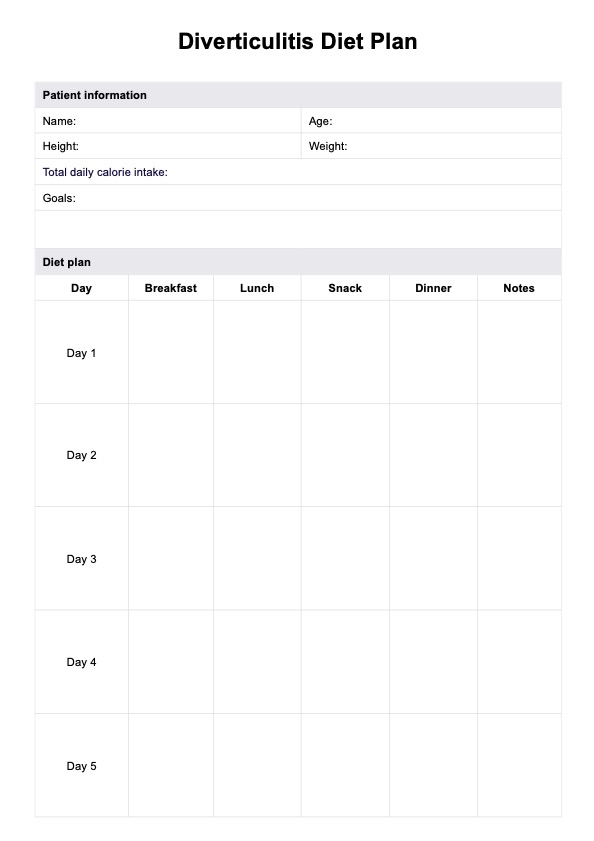
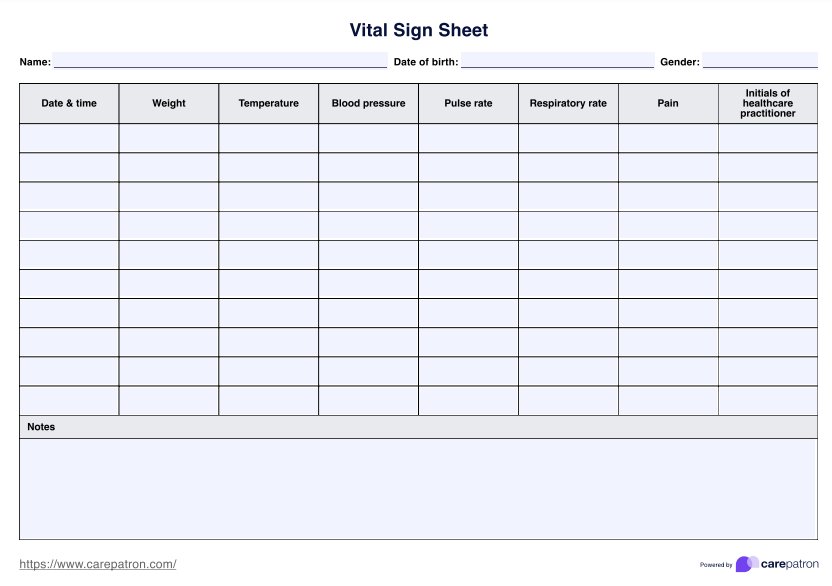
Diverticulitis Test Template
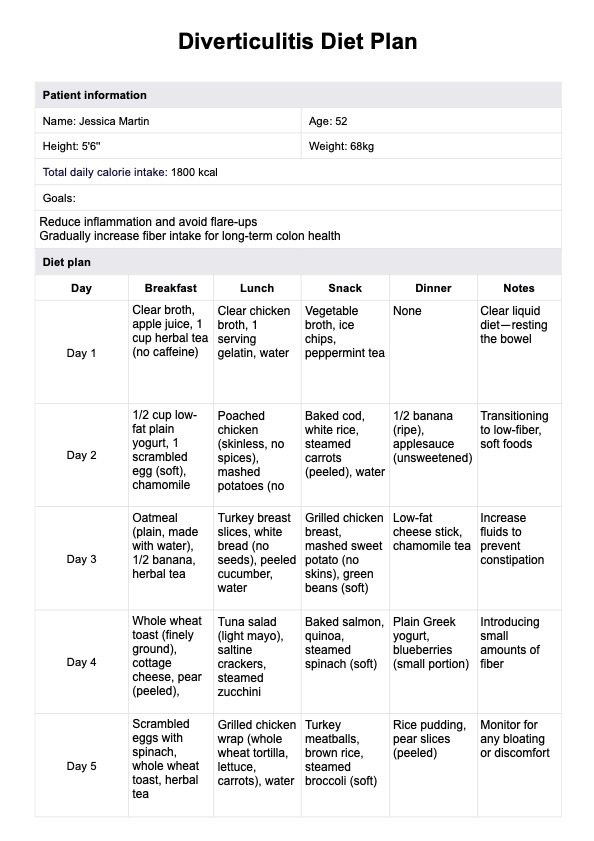
Diverticulitis Test Example
Symptoms and risk factors
Diverticulitis manifests with various symptoms, primarily centered around the lower left abdomen. Common indications include severe abdominal pain, alterations in bowel habits, nausea, and vomiting. In some cases, individuals may experience chills and sudden belly pain. The severity of symptoms varies, with very mild cases exhibiting few signs, while more severe instances may involve complications such as abdominal abscess or bowel perforation.
Several risk factors contribute to the development of diverticulitis. Age is a significant determinant as the condition becomes more prevalent in older individuals. A history of diverticular disease or chronic inflammation in the digestive tract increases the likelihood of developing diverticulosis. Dietary choices play a crucial role, with a low-fiber diet correlating with the development of diverticulosis, the precursor to diverticulitis.
Women of childbearing age face an elevated risk, potentially linked to hormonal factors. Other contributors include conditions affecting the digestive system, the use of nonsteroidal anti-inflammatory drugs (NSAIDs), lack of physical activity, and obesity. Certain genetic factors and compromised immune systems also play a role in susceptibility.
Preventive measures to prevent diverticulitis involve regular check-ups, a healthy lifestyle, and managing risk factors. Increased fiber intake, hydration, and a balanced diet promote digestive health, potentially reducing the risk of diverticulitis. Timely medical attention is crucial for those experiencing diverticulitis symptoms or possessing risk factors, as early detection and accurate diagnosis are pivotal for effective management and preventing severe complications associated with diverticulitis.
Diagnostic tests
Accurate diagnosis of diverticulitis is essential for timely and effective chronic condition management. Medical professionals employ a combination of diagnostic tests to diagnose diverticulitis, assess symptoms, identify complications, and tailor appropriate treatment plans. The diagnostic process of treating diverticulitis typically involves a sequential approach, starting with non-invasive methods before considering more invasive procedures.
- Physical examination: The initial step in diagnosing diverticulitis often involves a thorough physical examination. Healthcare providers assess the patient's abdominal tenderness, focusing on the lower left quadrant where diverticula are commonly located. Other signs, such as fever and elevated heart rate, may also be evaluated during this non-invasive assessment.
- Blood tests: Blood tests play a crucial role in the diagnostic process by revealing potential signs of inflammation or infection. Elevated white blood cell counts and increased levels of inflammatory markers can indicate the presence of diverticulitis. These tests aid in confirming the diagnosis and assessing the severity of the condition.
- Imaging studies: Imaging studies, including computed tomography (CT) scans, are instrumental in visualizing the gastrointestinal tract and detecting complications such as abscesses or bowel perforations. CT scans provide detailed images, allowing healthcare professionals to assess accurately and determine the most appropriate course of action.
- Colonoscopy: In some cases, a colonoscopy may be recommended to examine the entire colon. While not typically the first choice for diagnosing diverticulitis, a colonoscopy can help rule out other conditions and identify abnormalities within the colon, contributing to a comprehensive evaluation.
- Stool tests: Stool tests are valuable in excluding alternative causes of gastrointestinal symptoms and identifying signs of bleeding. Guaiac or fecal immunochemical tests may be conducted to check for blood in the stool, aiding in the diagnostic process.
Interpreting test results
Interpreting test results is crucial in understanding an individual's health status. Here's a breakdown of the process:
Normal findings
Normal results in diverticulitis indicate the absence of acute inflammation or complications. Diverticulitis is the inflammation of the diverticula, which are pockets inside the colon. When the condition is uncomplicated, it heals quickly with the proper treatment, and normal findings suggest the absence of inflammation and possible infection.
However, about 25% of people with acute diverticulitis develop complications, which may include abscesses, blockage in the bowel, perforation, bowel obstruction, and fistula. In the absence of these complications, the results would be considered normal.
Physical findings in diverticulitis may include abdominal tenderness, distension, a tender mass in the abdomen, absent or abnormal bowel sounds, and conclusions related to fistula formation. Left lower quadrant tenderness is the most common physical exam finding called diverticulitis, as most diverticula occur in the sigmoid colon. Normal findings in the physical examination suggest the absence of these signs, indicating the lack of acute inflammation or complications.
Abnormal findings
Abnormal results in the context of diverticulitis may indicate various deviations from the expected values, signaling potential health issues. These abnormal findings could include:
- Elevated white blood cell counts in blood tests may indicate the presence of an infection or inflammation.
- Blood in stool tests suggests gastrointestinal bleeding, which can be a sign of complications such as diverticular bleeding.
- Visual evidence of diverticula, inflammation, or complications in imaging studies, such as edematous thickening of the bowel wall with inflammatory changes, abscess, or scarring due to chronic inflammation.
These abnormal findings are essential for diagnosing and managing diverticulitis, as they can indicate the presence of complications or the need for further evaluation and treatment.
Correlation with symptoms and clinical history
While individual tests offer valuable clues, a complete picture of diverticulitis requires piecing them together with a patient's history and symptoms. This symphony of information is crucial for accurate diagnosis, especially in severe cases.
Imagine a patient with severe abdominal pain and altered bowel habits. Blood tests might show high white blood cell counts, hinting at inflammation. Stool tests, like finding blood, could point to potential bleeding. But the real story unfolds when we connect these findings with the patient's medical history. Have they had previous digestive issues? Are there any pre-existing conditions that influence the stool test's interpretation?
Different tests play specific roles. CT scans and ultrasounds offer a visual map of the colon, revealing inflamed tissue, abscesses, or scarring from chronic inflammation. However, their accuracy can vary depending on the location of the inflamed colon cancer diverticula. For example, one study found point-of-care ultrasound highly accurate in diagnosing uncomplicated cases in Asian populations but less so for specific locations like the cecum.
Ultimately, a holistic approach is the key to unlocking the proper diagnosis. By carefully considering symptoms, medical history, and the specific insights offered by each test, healthcare professionals can comprehensively understand the situation and chart the best course of treatment.
Follow-up and treatment
Follow-up and treatment play crucial roles in managing diverticulitis effectively. Here's a concise overview:
Follow-up
- Medical monitoring: Regular follow-up appointments are essential for monitoring the progress of diverticulitis and assessing the response to treatment.
- Diagnostic tests: Follow-up may involve repeating diagnostic tests, such as CT scans or blood tests, to track improvements or identify any recurrence of symptoms.
- Symptom evaluation: Ongoing assessment of symptoms, including abdominal pain, bowel habits, and overall well-being, helps determine the effectiveness of the treatment plan.
Treatment
- Antibiotics: If diverticulitis is uncomplicated, antibiotics are commonly prescribed to address the infection. Follow the prescribed course diligently.
- Pain management: Severe abdominal pain can be managed with pain relievers, as healthcare professionals recommend.
- Dietary changes: Adopting a clear liquid or low-residue diet during acute episodes helps rest the digestive system. Gradual reintroduction of fiber is often advised during recovery.
- Hospitalization: In severe cases or complications like abscess formation, hospitalization may be necessary for intravenous antibiotics, pain control, and close monitoring.
- Surgery: For recurrent or complicated cases, surgical interventions like bowel resection may be considered to address persistent symptoms or prevent future episodes.
Lifestyle modifications
- High-fiber diet: A high-fiber diet can promote bowel regularity and prevent diverticula formation.
- Hydration: Adequate fluid intake supports overall digestive health and prevents constipation.
- Regular exercise: Physical activity aids in maintaining a healthy digestive system.
Commonly asked questions
The best test for diverticulitis is a CT scan, which provides detailed gastrointestinal and intestinal tract images and helps identify complications.
Diverticulitis can be detected by blood tests that reveal signs of inflammation or infection, such as elevated white blood cell counts and inflammatory markers.
Warning signs and other symptoms of diverticulitis include severe abdominal pain, changes in bowel habits, nausea, vomiting, and, in some cases, chills and sudden belly pain.