Diverticulitis Diet Plan
Manage your client's diverticulitis symptoms with our Diverticulitis Diet Plan. Incorporate this template into your practice for free.


What is diverticulitis?
Some patients develop a condition where tiny sacs form along the colon and become blocked or inflamed. This condition is called diverticulitis, and it can cause sudden, severe pain, usually in the lower left side of the abdomen. Other symptoms may include constipation, diarrhea, fever, chills, nausea, or vomiting. In some cases, the pain starts mild and gradually worsens over a few days.
It isn't entirely clear what causes diverticulosis (when these sacs form) or diverticulitis (when they become inflamed), but certain factors to play a role. Genetics may make some people more likely to develop the condition, while lifestyle habits also contribute. Eating a low-fiber diet high in red meat, not exercising enough, and taking certain medications may increase the risk. Smoking and obesity are also linked to a higher chance of developing the condition.
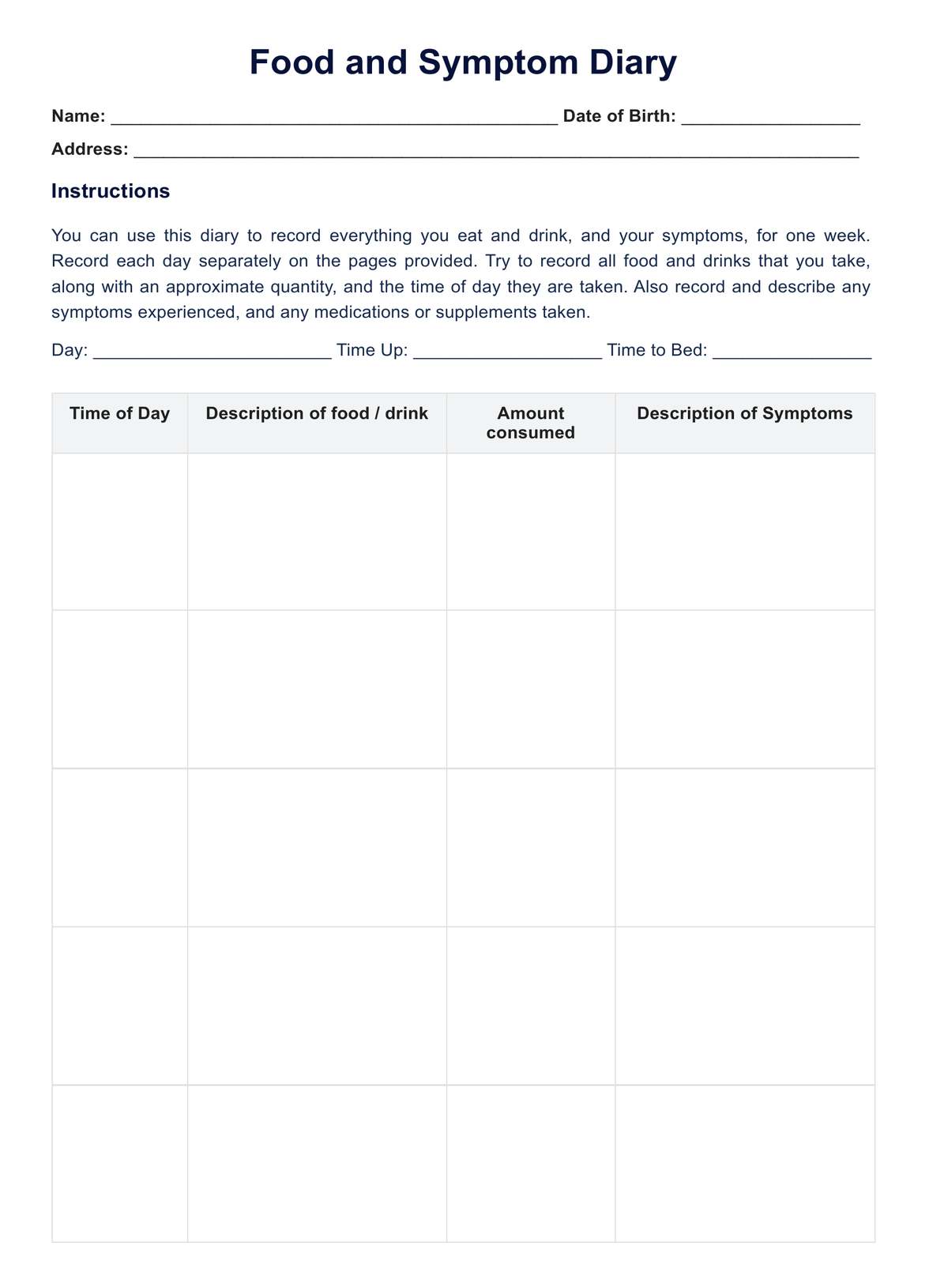
Managing diverticulitis often starts with diet changes, especially during flare-ups. A clear liquid diet may be recommended first, followed by a low-fiber diet, and then slowly transitioning back to high-fiber foods. Since diet plays a big role, having a Diverticulitis Diet Plan can help patients make better food choices and reduce the chances of future flare-ups.
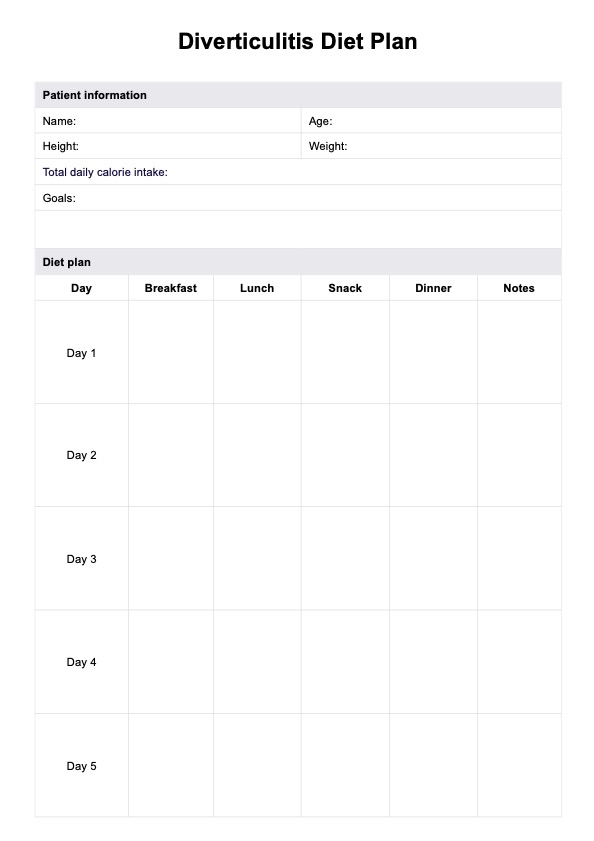
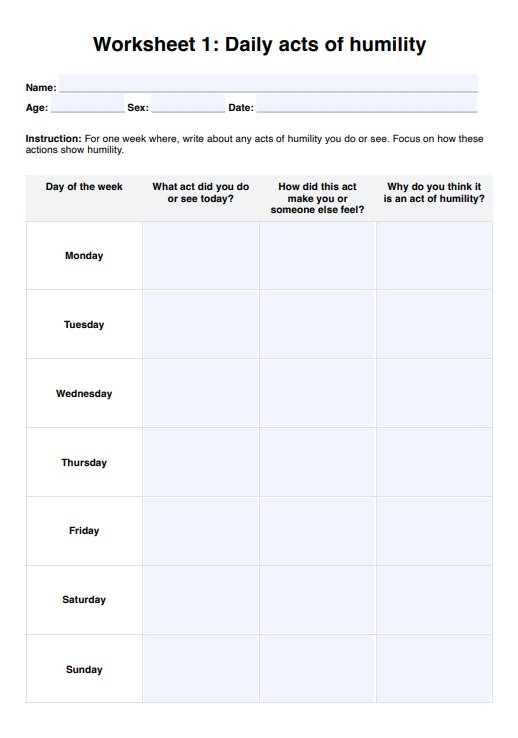
Diverticulitis Diet Plan Template
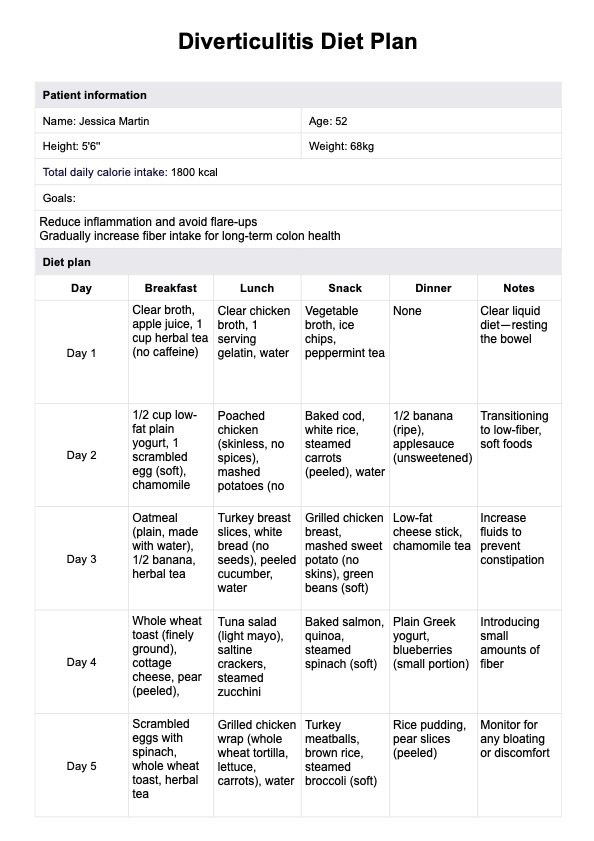
Diverticulitis Diet Plan Example
How does this Diverticulitis Diet Plan work?
When working with patients who need a diet for diverticulitis, having a structured meal plan can make all the difference. Whether you're working with a patient who needs a low-fiber diet to ease symptoms or someone ready to start eating high-fiber foods for prevention, this Diverticulitis Diet Plan will help guide their meals. Follow these four steps to use the template:
Step 1: Download the template
First, grab a copy of the Diverticulitis Diet Plan. You can click "Use template" and access it through the Carepatron platform. You can also select "Download" to get a fillable PDF copy of this diet plan.
Step 2: Assess the patient's needs
Before filling out the meal plan, determine where your patient is in their recovery. Are they currently in a diverticulitis flare-up, requiring a clear liquid diet? Or are they ready to slowly reintroduce into a normal diet of cooked vegetables, whole wheat bread, and other high-fiber foods? If they have a history of digestive and kidney diseases, be extra mindful of their fiber intake and how their digestive system reacts to certain foods.
Step 3: Customize the plan
Now it’s time to personalize the template. If your patient is in the early stages of recovery, focus on low-fiber foods like white rice and bananas. As they improve, incorporate more high-fiber diet foods like beans, whole grains, and vegetables. Keep an eye on foods that trigger diverticulitis, such as processed meats or fried foods.
Step 4: Provide guidance and follow-up
Once the plan is complete, review it with your patient. Emphasize the importance of gradually increasing dietary fiber while monitoring symptoms. Remind them to start slow with easy-to-digest options like cooked vegetables if they're moving from a liquid diet to solid foods. Schedule a follow-up to assess how their body responds and adjust the plan if needed.
When would you use this template?
This template is a great tool for creating personalized diet plans that are good for the patient's digestive tract. Here are three key situations where you might find it especially useful:
During a diverticulitis flare-up
When a patient has a diverticulitis flare-up, their stomach needs a break. They may have to stick to a clear liquid diet or a low-fiber diet for a while to let their digestive system heal. This template helps outline what they can eat, when to start adding cooked vegetables, and how to safely return to a normal diet without worsening symptoms.
When helping a patient recover
After a flare-up, patients need to reintroduce certain foods slowly so they don’t upset their stomachs. This template makes it easy to plan meals that start with gentle foods and gradually add more dietary fiber like high-fiber foods and whole grains. Having a step-by-step plan takes the guesswork out of recovery and helps them feel more in control.
For long-term digestive health
Some patients want to avoid future diverticulitis flare-ups by making smarter food choices. This template helps them build a diet with enough fiber intake from high-fiber foods while keeping track of any foods that trigger diverticulitis. It’s a simple way to help them stay on top of their digestive health and feel their best.
Benefits of using a plan for a diverticulitis diet
A diet plan takes the guesswork out of what to eat and when. Here are three benefits of our plan:
It's easy to use
Patients can follow clear guidelines for low-fiber foods, high-fiber foods, or a clear liquid diet based on their current needs. It helps them stay on track without constantly worrying about which certain foods might upset their digestive system.
It saves time
Planning meals ahead of time means less stress during busy days. Instead of scrambling to find dietary fiber-rich meals or safe cooked vegetables, patients already have a plan in place. This makes grocery shopping, meal prep, and daily eating much simpler.
It's available in digital and printable formats
Whether patients prefer a printed copy on the fridge or a digital version on their phone, this plan works both ways. Having it handy makes it easier to follow whether they're at home, dining out, or grocery shopping. A flexible format ensures they can stick to their diverticulitis diet no matter where they are.
Commonly asked questions
During a diverticulitis flare-up, clients may benefit from following a clear liquid diet to allow the digestive system time to rest. This could include consuming broth, clear juices, and gelatin while temporarily avoiding solid foods. Once symptoms start improving, they might gradually transition to a low-fiber diet before slowly reintroducing high-fiber foods as tolerated. They should consult a healthcare professional to determine its suitability for their needs.
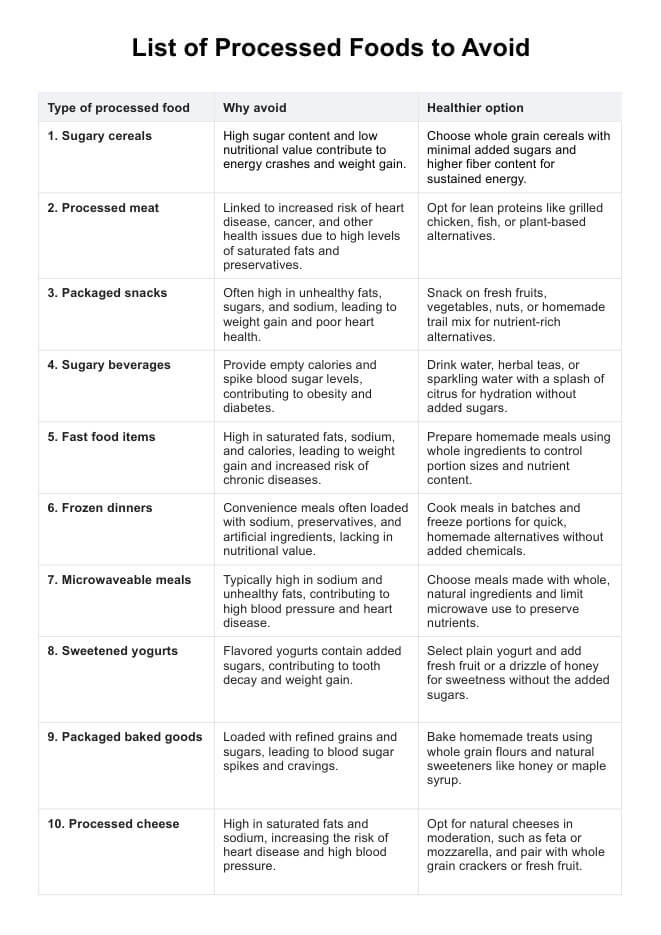
Some foods may contribute to digestive discomfort or inflammation, which could potentially trigger a flare-up in certain individuals. Processed foods, red meat, and low-fiber foods might slow digestion and increase pressure in the colon. Encouraging a balanced diet with dietary fiber from high-fiber foods, such as whole grains and vegetables, may help support digestive health and reduce the likelihood of a diverticulitis attack.
During a diverticulitis flare-up, it's best to follow a diet of clear liquids, including vegetable juice, broth, and water. As symptoms improve, you can gradually add canned or cooked fruits and other low-fiber foods before transitioning back to a healthy diet.