Type 2 Diabetes Treatment Guidelines
Get comprehensive guidelines and examples for treating Type 2 Diabetes in Carepatron's free PDF download.


What is type 2 diabetes mellitus?
Type 2 diabetes mellitus, commonly referred to as type 2 diabetes, is a chronic metabolic disorder characterized by elevated levels of glucose (sugar) in the blood. Unlike type 1 diabetes, where the body's immune system attacks and destroys insulin-producing cells in the pancreas, type 2 diabetes typically develops when the body becomes resistant to the effects of insulin or doesn't produce enough insulin to maintain normal blood sugar levels. Insulin is a hormone produced by the pancreas that helps regulate blood sugar and allows glucose to enter cells to be used as energy.
Patients with type 2 diabetes mellitus often experience symptoms such as increased thirst, frequent urination, fatigue, and blurred vision. However, some individuals may have the condition for years without noticeable symptoms, making early detection through routine blood tests crucial.
Type 2 diabetes management is vital to prevent complications such as chronic kidney disease and atherosclerotic cardiovascular disease, both of which are more common in patients with type 2 diabetes mellitus. Therefore, understanding and effectively managing the condition are paramount.
Education on diabetes self-management plays a crucial role in empowering individuals with type 2 diabetes to take control of their health. This education includes learning about proper nutrition, regular physical activity, monitoring blood sugar levels, taking medications as prescribed, and managing stress.
Type 2 diabetes mellitus symptoms
Type 2 diabetes mellitus can manifest through various symptoms, although some individuals may not experience any noticeable signs in the early stages of the condition. Being aware of these symptoms is crucial for early detection and prompt management. Below are common symptoms associated with type 2 diabetes mellitus:
- Increased thirst: Experiencing excessive thirst, even after drinking fluids.
- Frequent urination: Needing to urinate more often than usual, particularly at night.
- Fatigue: Feeling unusually tired or lethargic, even after adequate rest.
- Blurred vision: Experiencing blurry or distorted vision, often due to fluctuations in blood sugar levels affecting the eyes.
- Slow wound healing: Cuts, bruises, or sores take longer than usual.
- Tingling or numbness: Feeling tingling sensations or numbness, especially in the hands or feet.
- Unexplained weight loss: Losing weight without making any significant changes to diet or exercise routine.
Type 2 diabetes causes
Type 2 diabetes mellitus develops when the body becomes resistant to insulin or fails to produce enough insulin to regulate blood sugar levels effectively. Several factors contribute to the development of type 2 diabetes. Understanding these causes is essential for prevention and management. Below are common causes associated with type 2 diabetes mellitus:
- Insulin resistance: Cells in the body become resistant to the effects of insulin, leading to elevated blood sugar levels. This resistance often develops due to excess body weight, particularly around the abdomen, and lack of physical activity.
- Genetics: Family history and genetics play a significant role in the risk of developing type 2 diabetes mellitus. Individuals with a family history of the condition are more likely to develop it themselves.
- Obesity: Excess body weight, especially visceral fat (fat stored around the abdomen), increases the risk of resistance to insulin and type 2 diabetes mellitus. Obesity is a significant risk factor for the development of the condition.
- Unhealthy lifestyle: Poor diet and lack of physical activity contribute to the development of type 2 diabetes mellitus. Consuming high-calorie, high-sugar foods and leading a sedentary lifestyle can increase the risk of obesity and resistance to insulin.
- Age: The risk of type 2 diabetes mellitus increases with age, particularly after age 45. Aging is associated with decreased insulin sensitivity and changes in metabolic function.
- Ethnicity: Certain ethnic groups, including African Americans, Hispanic/Latino Americans, Native Americans, and Asian Americans, have a higher prevalence of type 2 diabetes mellitus compared to other populations.
Type 2 Diabetes Treatment Guidelines Template
Type 2 Diabetes Treatment Guidelines Example
How is this different from type 1 diabetes?
Type 2 diabetes mellitus and type 1 diabetes present distinct forms of diabetes with unique characteristics, causes, and treatment approaches. In type 2 diabetes, the body typically becomes resistant to insulin or fails to produce sufficient insulin to regulate blood glucose levels adequately. This resistance often develops due to excess body weight, sedentary lifestyle, and genetic predisposition.
On the other hand, type 1 diabetes results from the autoimmune destruction of insulin-producing beta cells in the pancreas, leading to an absolute deficiency of insulin.
Unlike type 2 diabetes, which commonly develops in adulthood and is associated with lifestyle factors, type 1 diabetes often manifests in childhood or adolescence and is less influenced by lifestyle choices.
Treatment approaches also differ significantly between the two types. Individuals with type 2 diabetes often begin with lifestyle modifications, including diet and exercise, to improve insulin sensitivity and blood glucose control. Oral medications or injectable therapies such as GLP-1 receptor agonists or insulin may be prescribed as the disease progresses.
Conversely, individuals with type 1 diabetes require lifelong insulin therapy to manage blood glucose levels. This typically involves multiple daily insulin injections or insulin pump therapy to mimic the body's natural insulin secretion.
How do healthcare professionals diagnosis type 2 diabetes?
Diagnosing type 2 diabetes involves a series of steps aimed at assessing an individual's blood glucose levels and identifying any signs or symptoms of the condition. Healthcare professionals follow guidelines established by organizations such as the American Diabetes Association (ADA) to ensure accurate diagnosis and appropriate management.
Here are the steps involved in diagnosing type 2 diabetes:
Screening high-risk individuals
Healthcare providers may initiate screening for type 2 diabetes in individuals who are at high risk based on factors such as obesity, sedentary lifestyle, family history of diabetes, or history of gestational diabetes. Screening may involve assessing fasting plasma glucose levels, OGTT, or A1C levels.
Assessing symptoms
Patients with type 2 diabetes may present with symptoms such as increased thirst, frequent urination, fatigue, blurred vision, and unexplained weight loss. Healthcare professionals carefully evaluate these symptoms during the diagnostic process.
Conducting laboratory tests
Laboratory tests play a crucial role in confirming the diagnosis of type 2 diabetes. The ADA recommends the use of specific diagnostic criteria, including:
- Fasting Plasma Glucose (FPG) test: A blood test measuring glucose levels after an overnight fast.
- Oral Glucose Tolerance Test (OGTT): A test measuring glucose levels before and after consuming a glucose solution.
- Hemoglobin A1C (A1C) test: A blood test reflecting average blood glucose levels over the past 2-3 months.
Confirming diagnosis
To confirm the diagnosis of type 2 diabetes, healthcare professionals typically require two separate measurements indicating elevated blood glucose levels. The ADA diagnostic criteria include:
- Fasting Plasma Glucose ≥ 126 mg/dL (7.0 mmol/L)
- 2-hour Plasma Glucose during OGTT ≥ 200 mg/dL (11.1 mmol/L)
- A1C ≥ 6.5%
Evaluating for complications
Once diagnosed, healthcare professionals may assess patients for complications associated with type 2 diabetes, such as cardiovascular disease, diabetic kidney disease, and microvascular complications. Early detection and management of complications are essential for optimizing patient outcomes.
Developing a management plan
Following diagnosis, healthcare professionals work with patients to develop a comprehensive management plan tailored to their needs. This plan may include medical nutrition therapy, physical activity recommendations, weight management strategies, medication management (including insulin therapy if needed), and regular monitoring of blood glucose levels.
Treatment guidelines
Effective management of type 2 diabetes mellitus involves a comprehensive approach aimed at controlling blood glucose levels, preventing complications, and improving overall health outcomes. The following treatment guidelines outline key strategies recommended for individuals with type 2 diabetes:
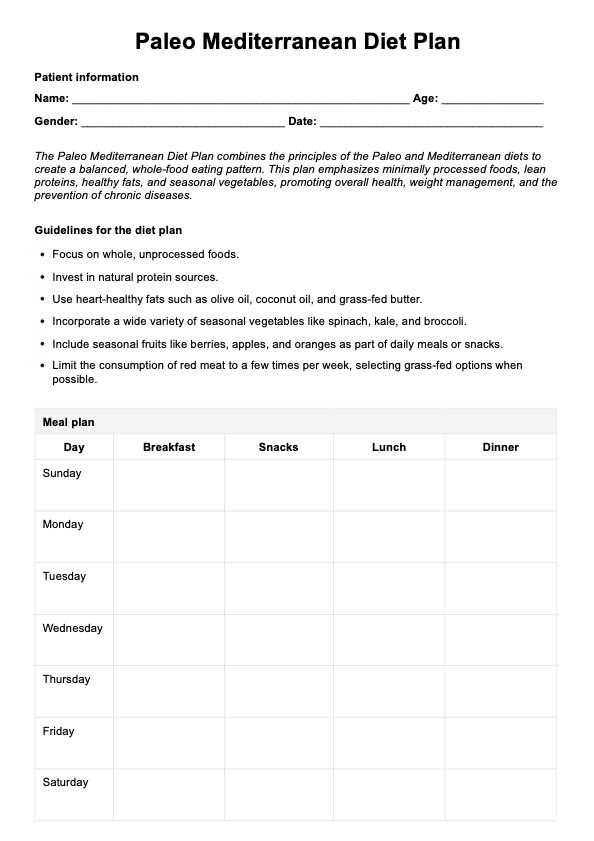
Medical nutrition therapy (MNT)
Medical nutrition therapy is crucial in managing type 2 diabetes by promoting healthy eating habits and controlling blood glucose. Individuals with type 2 diabetes should receive personalized nutrition counseling from a registered dietitian or certified diabetes educator. Emphasis should be placed on consuming a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats while limiting refined carbohydrates, saturated fats, and sodium.
Physical activity
Regular physical activity helps improve insulin sensitivity, lower blood glucose levels, and promote overall health and well-being. Patients with type 2 diabetes should engage in at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity aerobic exercise per week, spread across at least three days. Additionally, resistance training exercises should be performed at least two days per week.
Medication management
Medications are often necessary to achieve target blood glucose levels and reduce the risk of complications in patients with type 2 diabetes. Medication therapy should be individualized based on factors such as glycemic control, presence of comorbidities, risk of hypoglycemia, and patient preferences. Commonly used medications include metformin, sulfonylureas, DPP-4 inhibitors, GLP-1 receptor agonists, SGLT2 inhibitors, and insulin therapy.
Monitoring blood glucose levels
Regular monitoring of blood glucose levels helps patients and healthcare providers assess the effectiveness of treatment and make necessary adjustments. Patients with type 2 diabetes should monitor their blood glucose levels according to their healthcare provider's recommendations. This may include self-monitoring of blood glucose using a glucometer and periodic A1C testing to assess long-term glucose control.
Diabetes self-management education and support (DSMES)
Diabetes self-management education empowers patients with the knowledge and skills needed to manage their condition and prevent complications effectively. Patients should receive comprehensive DSMES, including education on diabetes self-monitoring, medication management, nutrition therapy, physical activity, blood glucose target ranges, and strategies for preventing and managing hypoglycemia and hyperglycemia.
Regular follow-up care
Regular follow-up visits with healthcare providers are essential for ongoing assessment, monitoring, and adjustment of treatment plans. Patients should schedule regular follow-up appointments with their healthcare team, including physicians, nurses, dietitians, and diabetes educators, to review progress, address concerns, and make any necessary changes to their diabetes management plan.
How does our Type 2 Diabetes Treatment Guidelines template work?
Our Type 2 Diabetes Treatment Guidelines template at Carepatron operates based on the latest standards and guidelines, notably the 2024 ADA Diabetes Standards of Medical Care Clinical Guideline Summary from the American Diabetes Association (ADA).
Here's how our template functions:
Timely and evidence-based treatment decisions
Our template ensures that treatment decisions are made promptly and based on evidence-based guidelines. It captures essential elements within the social determinants of health and promotes collaborative decision-making with individuals with diabetes and their care partners, considering individual preferences, prognoses, comorbidities, and financial considerations.
Alignment with the chronic care model
We align our diabetes management approach with the Chronic Care Model, emphasizing person-centered team care and integrated long-term treatment approaches for diabetes and comorbidities. Our template fosters ongoing collaborative communication and goal setting among all team members to optimize patient outcomes.
Facilitation of team-based care
Carepatron's template facilitates both in-person and virtual team-based care, ensuring that individuals with diabetes have access to a multidisciplinary team knowledgeable and experienced in diabetes management. We utilize patient registries, decision support tools, and community involvement to meet the diverse needs of individuals with diabetes.
Assessment of diabetes health care maintenance
Our template includes tools for assessing diabetes health care maintenance using reliable and relevant data metrics. We prioritize improving processes of care and health outcomes while considering care costs, individual preferences and goals, and treatment burden. By leveraging these assessments, we aim to optimize the quality and efficiency of diabetes care delivery.
Benefits of having Type 2 Diabetes Treatment Guidelines
Type 2 Diabetes Treatment Guidelines offer numerous benefits for healthcare providers and patients, ensuring optimal management of the condition and reducing the risk of complications. Let's explore these benefits:
1. Evidence-based care
By adhering to established treatment guidelines, healthcare providers can deliver evidence-based care grounded in scientific research and recommendations from organizations such as the American Diabetes Association (ADA). This ensures that patients receive the most effective treatments backed by clinical evidence.
2. Risk factor management
Treatment guidelines provide clear recommendations for managing risk factors associated with type 2 diabetes, such as obesity, high blood pressure, and dyslipidemia. Implementing these recommendations helps reduce the risk of cardiovascular events and other complications associated with the condition.
3. Glycemic control
Guidelines establish glycemic targets for blood glucose levels, allowing healthcare providers to monitor and adjust treatment plans to achieve optimal glycemic control. Maintaining blood glucose within target ranges reduces the risk of diabetes-related complications and improves overall health outcomes.
4. Prevention of complications
Treatment guidelines emphasize the importance of early intervention and preventive measures to reduce the risk of complications such as diabetic kidney disease, neuropathy, and retinopathy. By following these guidelines, healthcare providers can help prevent or delay the onset of diabetes-related complications.
5. Personalized treatment plans
Guidelines consider individual patient characteristics, including age, comorbidities, and treatment preferences, allowing healthcare providers to develop personalized treatment plans tailored to each patient's needs. This customized approach improves treatment adherence and patient satisfaction.
6. Integration of new therapies
Treatment guidelines evolve based on emerging research and clinical trials, allowing for the integration of new therapies and technologies into diabetes management. Innovations such as continuous glucose monitoring (CGM) and novel glucose-lowering medications are incorporated into guidelines to improve patient outcomes.
7. Education and empowerment
Guidelines provide valuable education and resources for healthcare providers and patients, empowering individuals with the knowledge and skills to manage type 2 diabetes effectively. Education on lifestyle modifications, self-monitoring techniques, and medication management promotes patient empowerment and self-care.
Leveraging the diabetes treatment guidelines template can bolster your practice and client progress. This tool ensures a thorough assessment and effective intervention strategies.
Commonly asked questions
The standard treatment protocol for type 2 diabetes includes lifestyle modifications such as diet and exercise, along with oral medications or injectable therapies like insulin to control blood glucose levels.
Five main treatment options for type 2 diabetes include metformin, sulfonylureas, DPP-4 inhibitors, GLP-1 receptor agonists, and SGLT2 inhibitors, which can be used alone or in combination to lower blood glucose levels.
The advised treatment for type 2 diabetes includes a combination of lifestyle modifications, such as diet and exercise, along with medication management tailored to the individual patient's needs and preferences.













-template.jpg)