DSM 5 Criteria for Conduct Disorder
Discover the DSM 5 Criteria for Conduct Disorder and its impact on mental health. Learn about diagnosis, treatment, and research in our comprehensive guide.


What is conduct disorder?
Conduct Disorder (CD) is a mental health condition characterized by a persistent pattern of aggressive, defiant, and antisocial behaviors that violate the rights of others or societal norms. Children and adolescents with CD may display a wide range of disruptive behaviors, such as:
- Physical aggression toward people or animals, including bullying, fighting, and cruelty.
- Destruction of property, such as vandalism or arson.
- Deceitfulness or theft, including lying, shoplifting, or breaking and entering.
- Serious rule violations include truancy, running away from home, or staying out late without permission.
These behaviors are not just occasional lapses in judgment or typical childhood mischief; they are more severe and persistent. Conduct disorder can lead to clinically significant impairment in social, academic, and/or occupational functioning. If untreated, it can persist into adulthood, potentially leading to antisocial personality disorder or other legal and social issues.
Causes of conduct disorder
The cause of conduct disorder is believed to be multifactorial, involving genetic, environmental, and psychological factors. A history of child abuse, family dysfunction, and exposure to violence are key risk factors that increase the likelihood of developing CD. Additionally, neurological issues, such as problems in the brain's frontal lobe, which is responsible for impulse control and judgment, may contribute to the disorder.
Consequences of conduct disorder
The consequences of conduct disorder can be severe and long-lasting. Individuals with CD are at a higher risk of academic failure, substance abuse, legal problems, and difficulties in relationships. Without treatment, CD can evolve into more serious mental health disorders, such as adult antisocial personality disorder (ASPD).
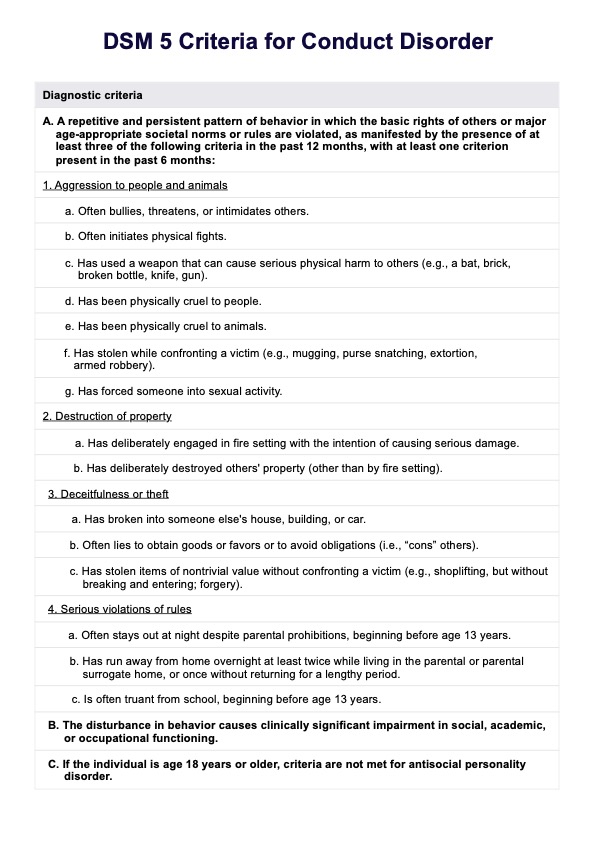
Difference of conduct disorder from oppositional defiant disorder and antisocial personality disorder
Conduct disorder is distinct from oppositional defiant disorder (ODD) and antisocial personality disorder (ASPD), although they share some similarities. ODD is characterized by a pattern of angry, defiant behavior but does not involve the violation of the basic rights of others to the extent seen in CD.
On the other hand, ASPD is a more severe form of CD that persists into adulthood, with a broader pattern of disregard for and violation of the rights of others. In fact, ASPD is the only personality disorder in the DSM that requires a person to be previously diagnosed with CD.
Understanding the nuances of these disorders is crucial for accurate diagnosis and effective treatment.
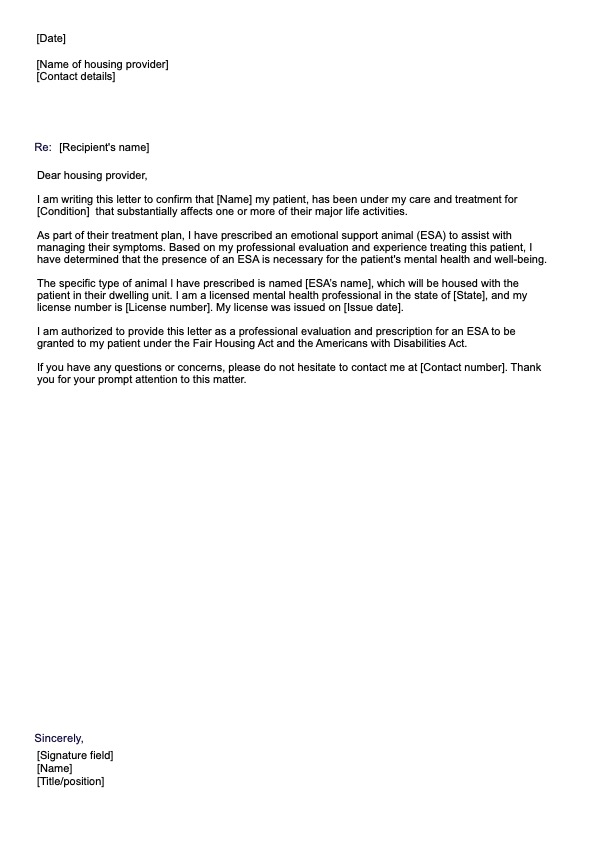
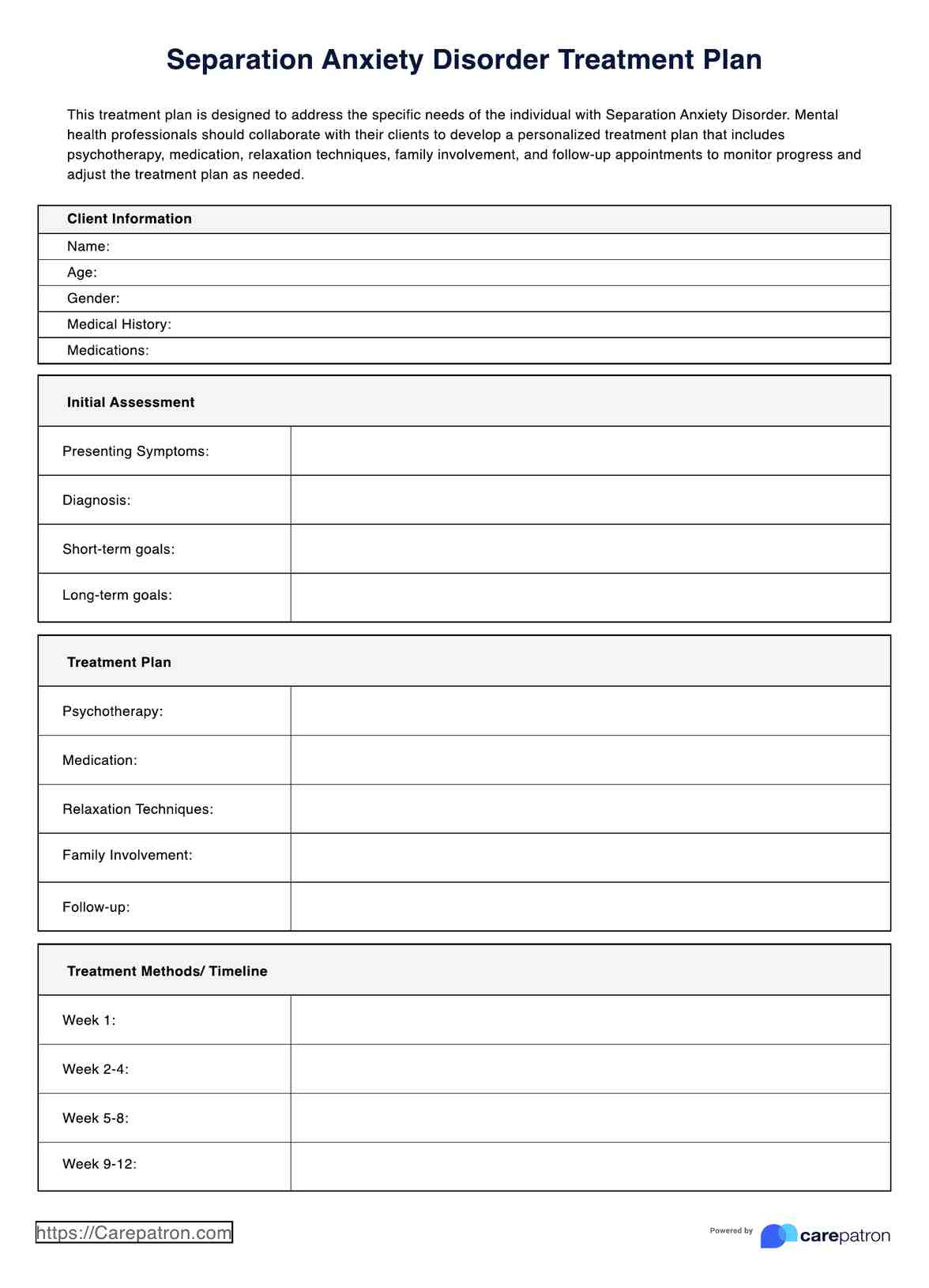
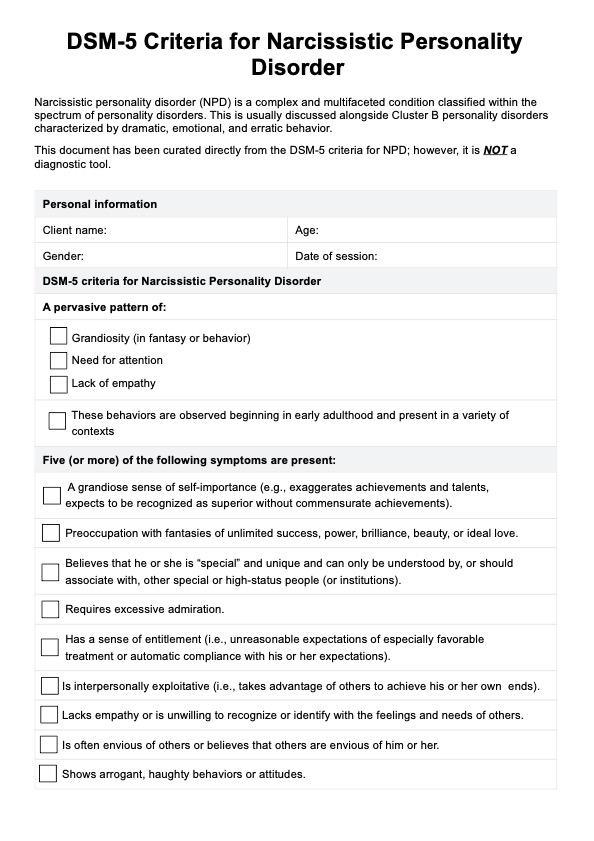
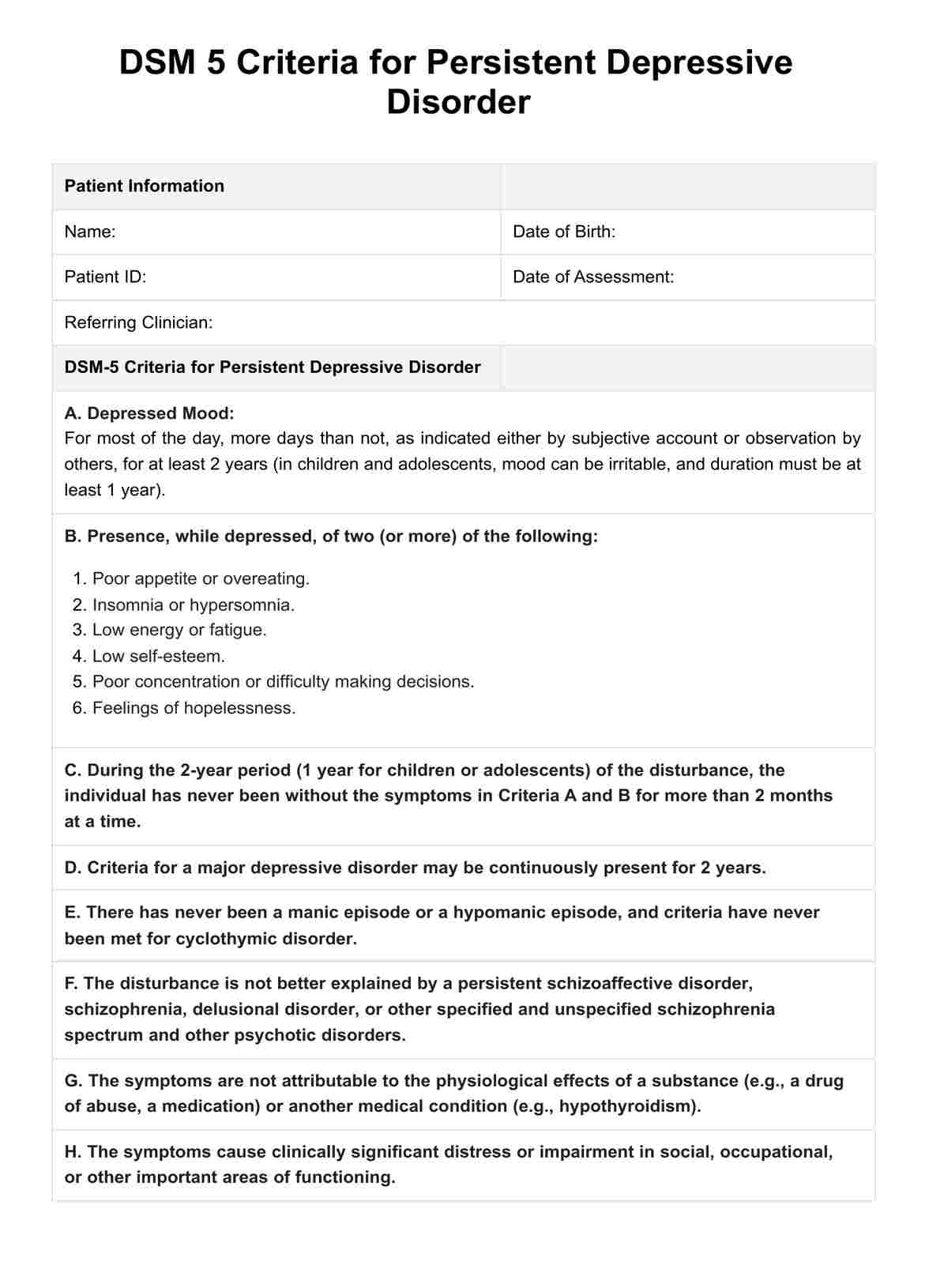
DSM 5 Criteria for Conduct Disorder Template
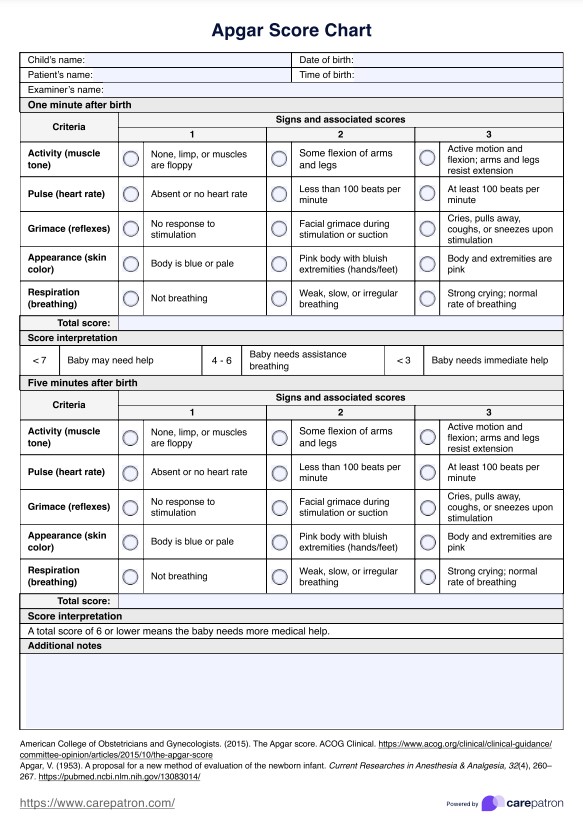
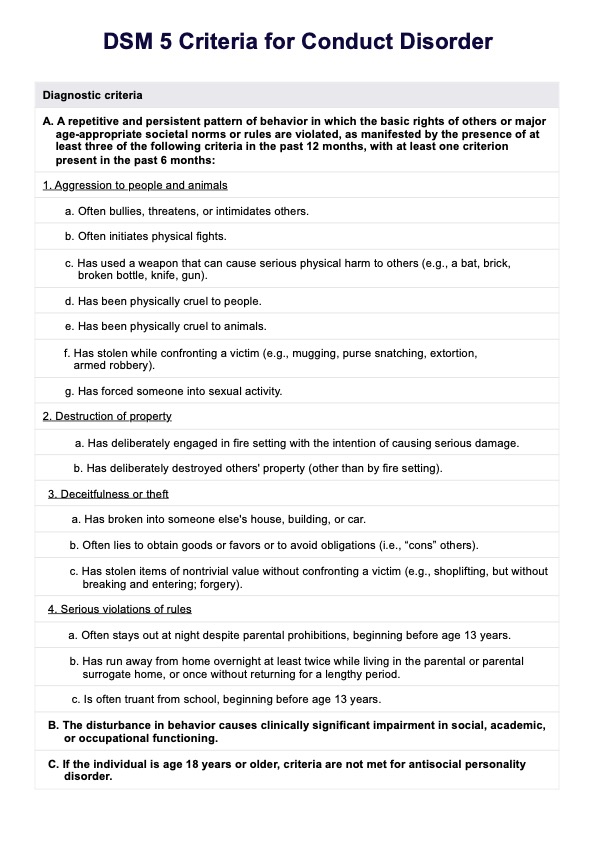
DSM 5 Criteria for Conduct Disorder Example
How do healthcare professionals diagnose conduct disorder?
To diagnose conduct disorder, healthcare professionals conduct a thorough evaluation that includes:
- Clinical interview: A detailed interview with the child, parents, and teachers to gather information about the child's behavior, family history, and any environmental factors that may contribute to the disorder.
- Observation: Observing the child's behavior in different settings, such as at home, school, or during the clinical interview, to identify patterns of conduct problems and to assess interpersonal and emotional functioning.
- Psychological testing: Administering standardized tests to assess the child's emotional, behavioral, and cognitive functioning, as well as any co-occurring mental health conditions.
- Medical evaluation: A physical examination to rule out any medical conditions contributing to the child's behavior.
- Review of records: Examining school records, medical history, and any previous psychological evaluations to gather additional information about the child's behavior and development.
By combining information from these assessments, healthcare professionals can determine whether the child meets the DSM-5 criteria for conduct disorder and develop an appropriate treatment plan while also considering the presence of co-occurring conditions such as bipolar disorder.
What is DSM 5?
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), is a comprehensive classification system for mental disorders. It is published by the American Psychiatric Association (APA) and is widely used by mental health professionals in the United States and around the world.
The DSM-5 serves as the standard for diagnosing mental disorders and provides standardized criteria to ensure consistency and accuracy in diagnosis. The manual covers a wide range of mental health conditions, including mood disorders, anxiety disorders, personality disorders, and more. The DSM-5 is regularly updated to reflect advances in our understanding of mental health and to incorporate the latest research findings.
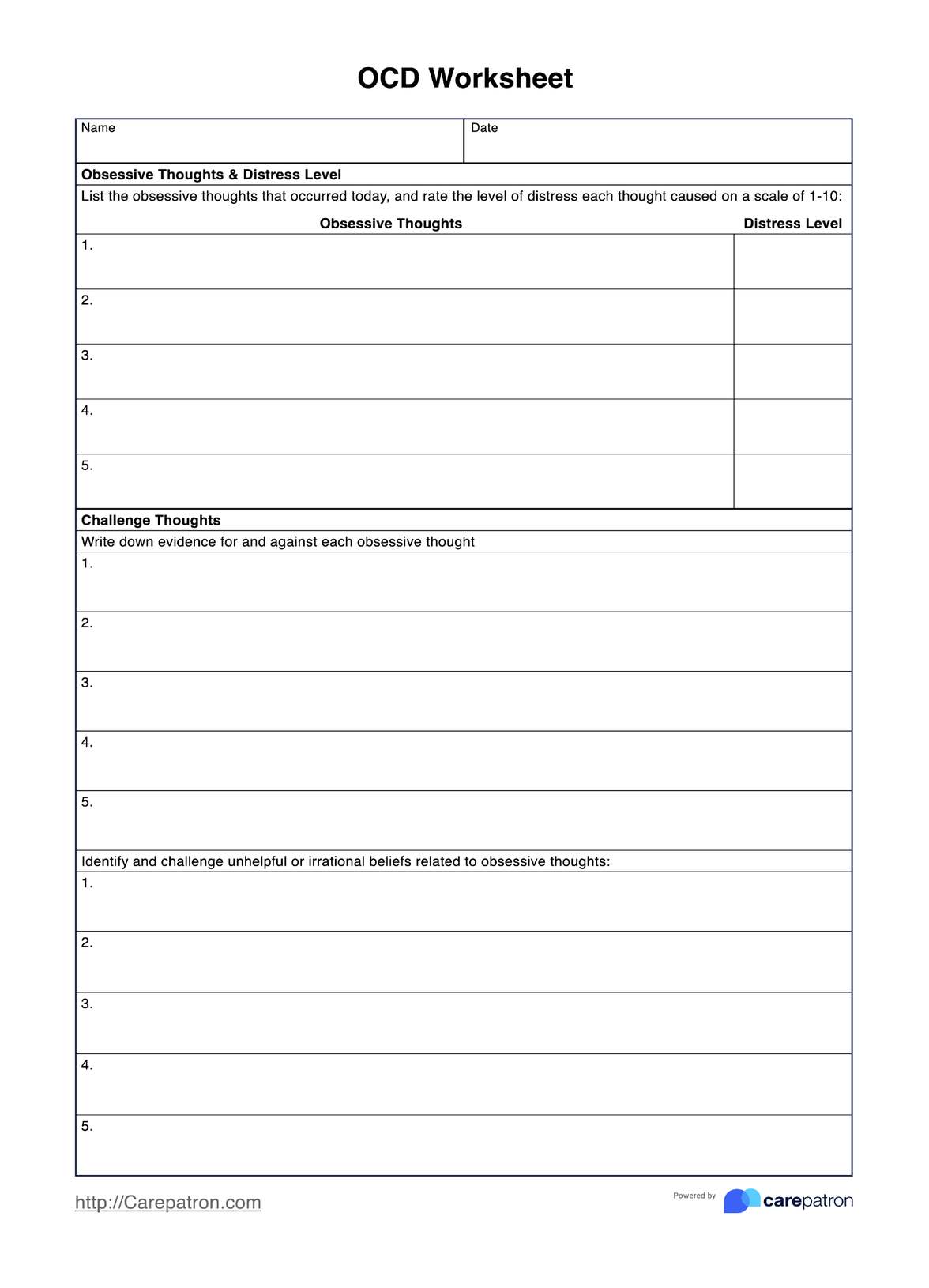
DSM criteria for conduct disorder
DSM criteria for conduct disorder outline specific behaviors and patterns that characterize the disorder. To be diagnosed with conduct disorder, a person must display a persistent pattern of behavior that violates the rights of others or major age-appropriate societal norms or rules. Essentially, these are conduct disorder symptoms.
According to the DSM-5, the criteria for conduct disorder include the following:
- Aggression to people and animals:
- Often bullies, threatens, or intimidates others.
- Often initiates physical fights.
- Has used a weapon that can cause serious physical harm to others (e.g., a bat, brick, broken bottle, knife, gun).
- Has been physically cruel to people.
- Has been physically cruel to animals.
- Has stolen while confronting a victim (e.g., mugging, purse snatching, extortion, armed robbery).
- Has forced someone into sexual activity.
- Destruction of property:
- Has deliberately engaged in fire setting with the intention of causing serious damage.
- Has deliberately destroyed others' property (other than by fire setting).
- Deceitfulness or theft:
- Has broken into someone else's house, building, or car.
- Often lies to obtain goods or favors or to avoid obligations (i.e., "cons" others).
- Has stolen items of nontrivial value without confronting a victim (e.g., shoplifting, but without breaking and entering; forgery).
- Serious violations of rules:
- Often stays out at night despite parental prohibitions, beginning before age 13 years.
- Has run away from home overnight at least twice while living in the parental or parental surrogate home (or once without returning for a lengthy period).
- Is often truant from school, beginning before age 13 years.
The presence of at least three of these criteria in the past 12 months, with at least one criterion present in the past six months, is required for a diagnosis of conduct disorder. The severity of conduct disorder can be classified as mild, moderate, or severe based on the number and severity of the behaviors exhibited.
Differences between the DSM 4 and DSM 5 conduct disorder criteria
Differences between the DSM-4 and DSM-5 conduct disorder criteria are relatively minor, but they do exist. The DSM-5, published in 2013, aimed to provide clearer, more precise criteria and reflect the latest field research.
Here are some of the key differences between the DSM-4 and DSM-5 criteria for conduct disorder:
- Disorder classification: DSM-4 classified Conduct Disorder under "Attention deficit and disruptive behavior disorders," but in the DSM-5, it has been reclassified under "Disruptive, Impulse-Control, and Conduct Disorders."
- Introduction of specifier: DSM-5 introduced a new specifier, "With limited prosocial emotions," to describe individuals who show at least two of the following traits persistently over at least 12 months and in multiple relationships and settings: lack of remorse or guilt, callous lack of empathy, unconcerned about performance, and shallow or deficient affect.
- Severity specifier: DSM-5 added a severity specifier (mild, moderate, severe) based on the number of conduct problems, their impact on others, and the harm caused.
These changes aimed to provide more detailed and accurate descriptions of individuals with Conduct Disorder, allowing for better diagnosis and treatment planning.
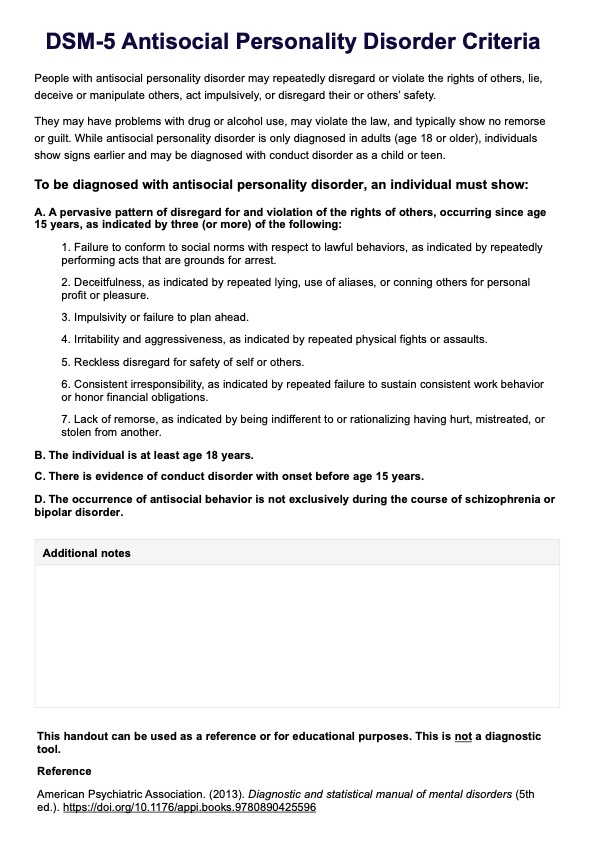
Conduct disorder treatment
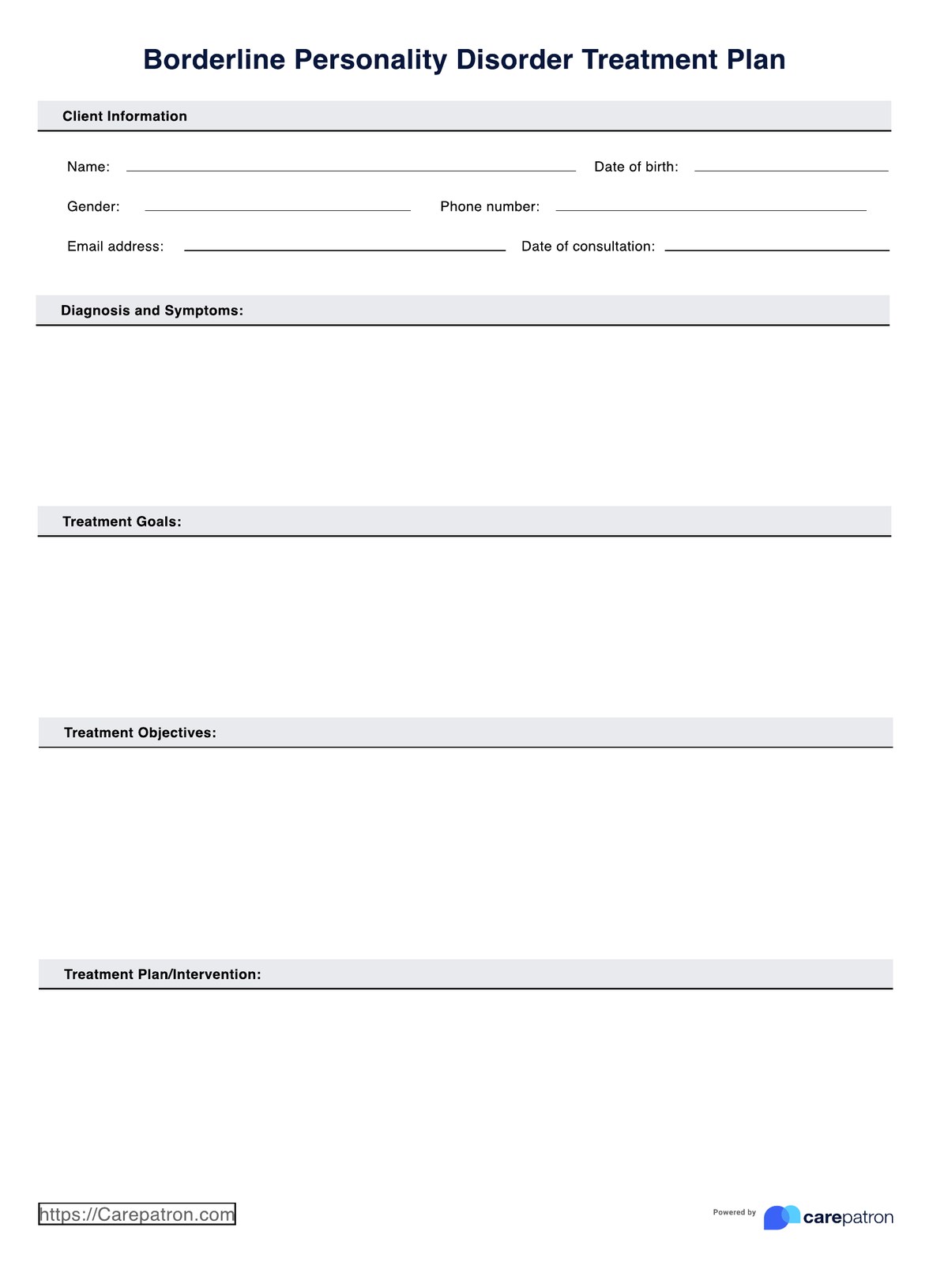
To effectively address Conduct Disorder, a comprehensive treatment plan is essential. Here are some key components of treatment for Conduct Disorder:
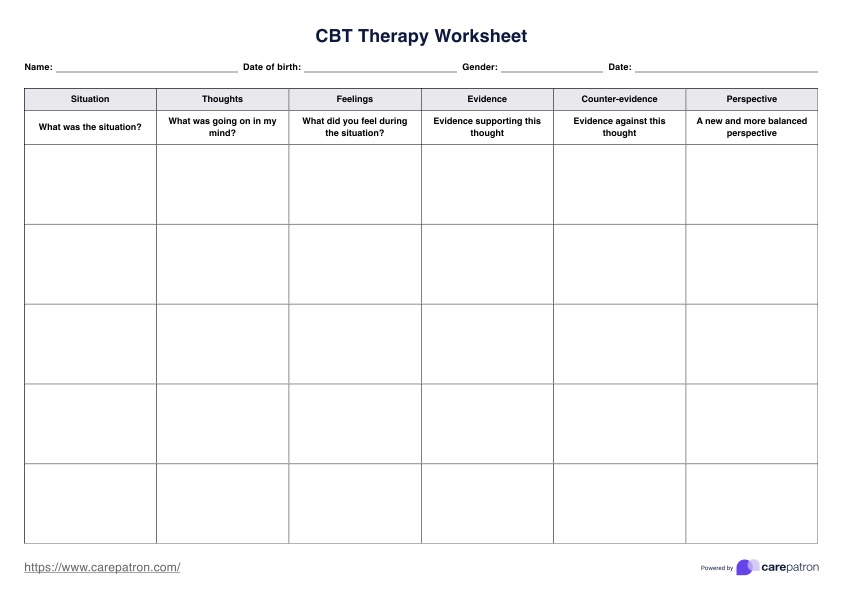
- Cognitive-behavioral therapy (CBT): CBT helps children and adolescents identify and change negative thought patterns and behaviors. It can improve problem-solving skills, anger management, and impulse control.
- Parent training programs: These programs educate parents on effective parenting techniques, such as setting clear boundaries, using consistent discipline, and reinforcing positive behaviors.
- Family therapy: Family therapy can address communication issues and conflict resolution and improve overall family dynamics, which can be crucial in managing conduct disorder.
- Medication: While there are no specific medications for Conduct Disorder, certain medications may be prescribed to treat co-occurring conditions such as ADHD, depression, or anxiety.
- Group therapy: Group therapy can provide a supportive environment for children and adolescents to learn social skills, empathy, and how to interact positively with peers.
It's important to note that early intervention and a tailored approach to treatment are crucial for effectively managing Conduct Disorder and preventing long-term consequences.
Research on conduct disorder
The study of Conduct Disorder (CD) has made significant strides in recent years, shedding light on its complex nature. Groundbreaking research provides a deeper understanding of the disorder, paving the way for more effective interventions.
One such study by Pardini and Frick (2013) explored multiple developmental pathways through which children and adolescents can develop a tendency toward Conduct Disorder. The review outlined three distinct etiological pathways based on the age of onset of antisocial behavior, the presence of callous-unemotional traits, and issues with anger regulation.
Another significant study conducted by Staginnus et al. (2023) at the University of Bath, UK, investigated brain structural differences in children with Conduct Disorder who experienced childhood maltreatment. They revealed that maltreated youths with CD exhibited more extensive changes in brain structure compared to non-maltreated youths with CD and healthy controls.
These studies highlight the importance of considering individual differences and environmental factors in understanding and treating Conduct Disorder. As research evolves, it promises more targeted and effective interventions for those affected by this challenging disorder.
References
Elmaghraby, R., & Garayalde, S. (2021, September). What are disruptive, impulse control and conduct disorders? Psychiatry.org. https://www.psychiatry.org/patients-families/disruptive-impulse-control-and-conduct-disorders/what-are-disruptive-impulse-control-and-conduct
Pardini, D., & Frick, P. J. (2013). Multiple developmental pathways to conduct disorder: Current conceptualizations and clinical implications. Journal of the Canadian Academy of Child and Adolescent Psychiatry, 22(1), 20–25. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3565711/
Searight, H. R., Rottnek, F., & Abby, S. L. (2001). Conduct disorder: Diagnosis and treatment in primary care. American Family Physician, 63(8), 1579–1589. https://www.aafp.org/pubs/afp/issues/2001/0415/p1579.html
Staginnus, M., Cornwell, H., Toschi, N., Oosterling, M., Paradysz, M., Smaragdi, A., González-Madruga, K., Pauli, R., Rogers, J. C., Bernhard, A., Martinelli, A., Kohls, G., Raschle, N. M., Konrad, K., Stadler, C., Freitag, C. M., De Brito, S. A., & Fairchild, G. (2023). Testing the ecophenotype model: Cortical structure alterations in conduct disorder with versus without childhood maltreatment. Biological Psychiatry: Cognitive Neuroscience and Neuroimaging, 8(6), 609–619. https://doi.org/10.1016/j.bpsc.2022.12.012
Substance Abuse and Mental Health Services Administration. (2016, June). Table 17, DSM-IV to DSM-5 conduct disorder comparison. PubMed; Substance Abuse and Mental Health Services Administration (US). https://www.ncbi.nlm.nih.gov/books/NBK519712/table/ch3.t13/
Commonly asked questions
The criteria for conduct disorder include a repetitive and persistent pattern of behavior that violates the basic rights of others or major age-appropriate societal norms or rules, with at least three of the specified criteria present in the past 12 months.
The DSM-5 code for conduct disorder is 312.81 for the childhood-onset type, 312.82 for the adolescent-onset type, and 312.89 for the unspecified onset.
No, conduct disorder and antisocial personality disorder (ASPD) are not the same. Conduct disorder is diagnosed in children and adolescents, while ASPD is diagnosed in adults. However, individuals with conduct disorder are at an increased risk of developing ASPD in adulthood.


















-template.jpg)