Burns Depression Checklist
Evaluate depression severity with the Burns Depression Checklist. Learn how to interpret findings and guide treatment decisions effectively.


What is major depressive disorder?
Experiencing a heavy weight upon waking, draining joy from daily activities, and rendering concentration difficult, alongside persistent feelings of emptiness and hopelessness, may indicate major depressive disorder (MDD). Seeking professional help is vital to address these symptoms and work towards recovery.
In 2008, the World Health Organization (WHO) identified major depressive disorder (MDD) as the third leading contributor to the global burden of disease. WHO forecasts suggest that by 2030, MDD is expected to become the leading cause (Bains & Abdijadid, 2023). A reliable screening tool is needed for both high and more typical prevalence. MDD isn't just feeling sad or down for a few days. It's a persistent and pervasive sense of emotional distress that significantly impacts a person's ability to function.
For many individuals, MDD begins with subtle signs that may go unnoticed or be dismissed as temporary mood swings. Initial signs frequently encompass feelings of melancholy, despair, agitation, and alterations in appetite, sleep habits, and energy levels. These signs can easily be mistaken for life's regular ups and downs, delaying recognizing a deeper problem.
This is where primary healthcare providers play a crucial role. They are often the first point of contact for individuals experiencing psychological and emotional distress, and their ability to detect low mood and inquire about the patient's mental health is vital. By fostering open and supportive communication, primary care providers can foster a safe space for patients to express their concerns and seek help.
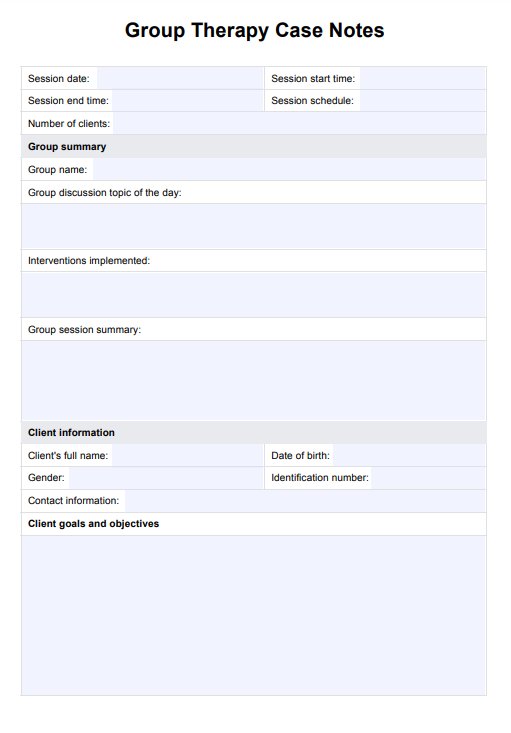
Burns Depression Checklist Template
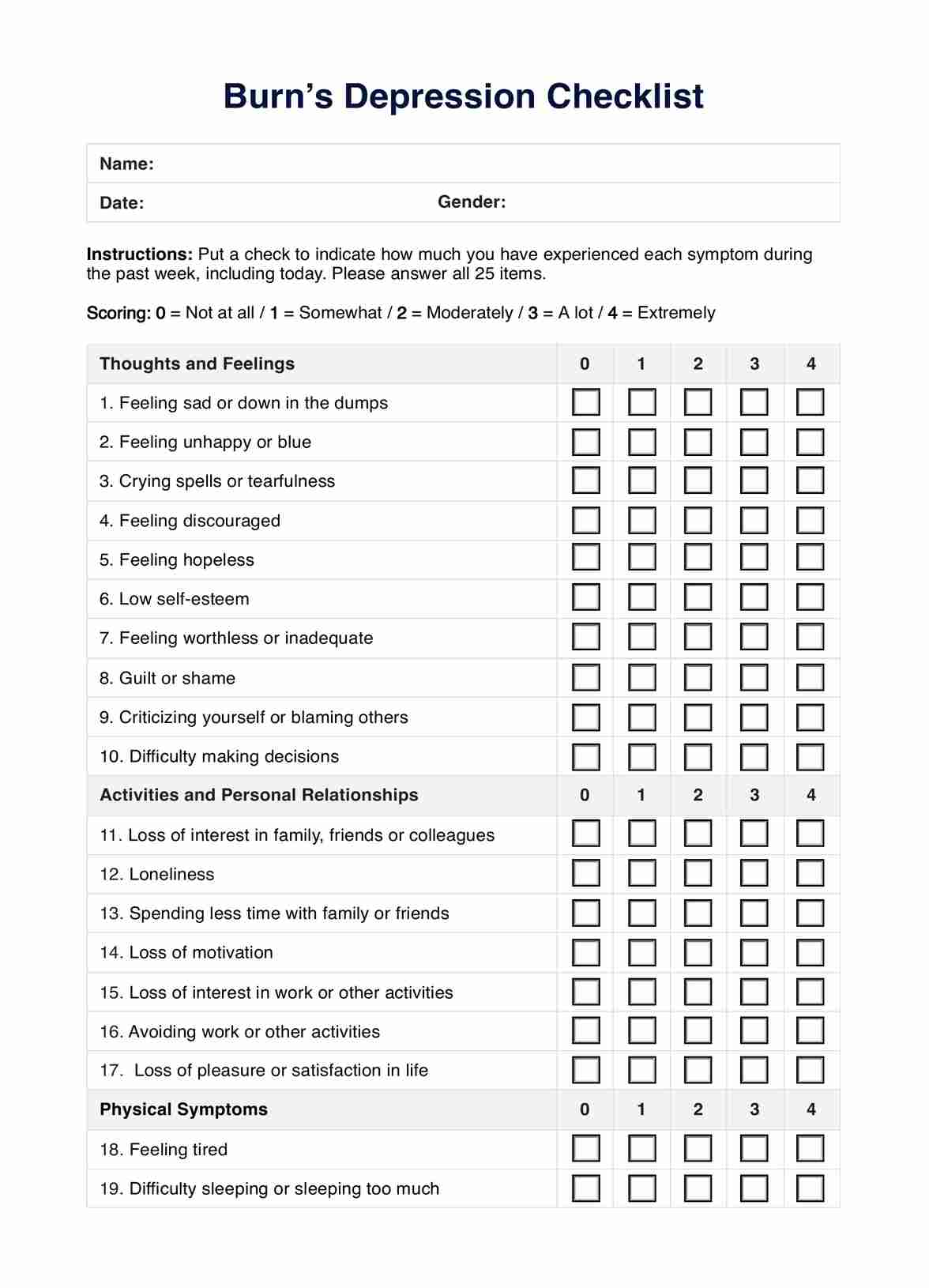
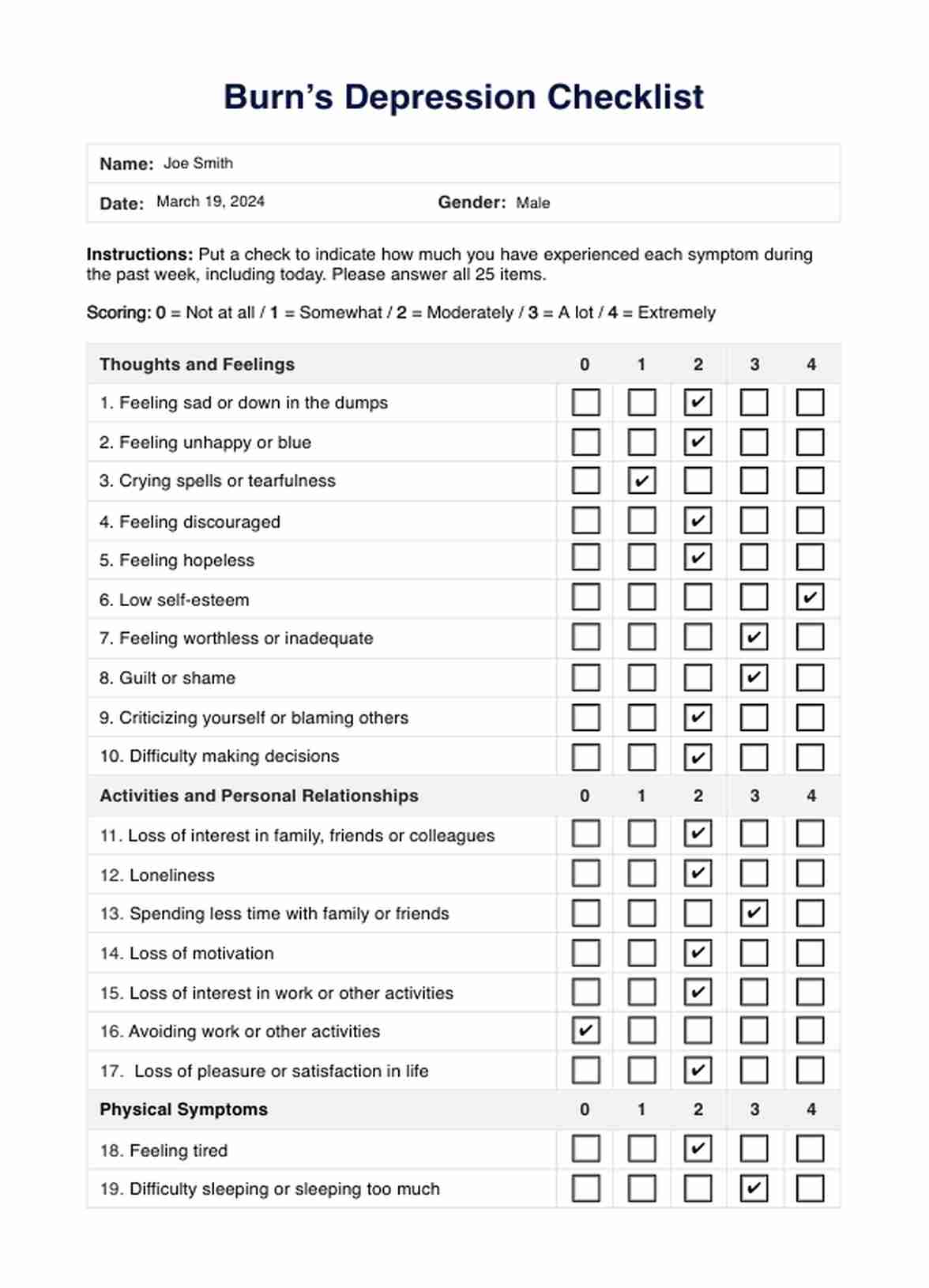
Burns Depression Checklist Example
Symptoms of major depressive disorder
Based on the Diagnostic and Statistical Manual of Mental Disorders or DSM-5 diagnosis, major depressive disorder (MDD) is characterized by the presence of five or more symptoms over two weeks, including at least one of either depressed mood or loss of interest or pleasure (Substance Abuse and Mental Health Services Administration, 2016).
Here are the common symptoms:
- Depressed mood most of the day, nearly every day
- Markedly diminished interest or pleasure in almost all activities
- Significant weight loss or gain or change in appetite
- Insomnia or hypersomnia
- Psychomotor agitation or retardation
- Fatigue or loss of energy
- Feelings of worthlessness or excessive guilt
- Diminished ability to think or concentrate, or indecisiveness
- Recurrent thoughts of death or suicide
Recognizing the symptoms of major depressive disorder is crucial for early intervention and appropriate treatment. By understanding these signs, individuals can seek support and embark on a path toward healing and improved mental well-being.
What is Burn's Depression Checklist?
The Burns Depression Checklist, also known as the Burns Depression Scale, is a depression screening tool developed by Dr. David Burns, a renowned psychiatrist and author.
Dr. David Burns, a magna cum laude graduate of Amherst College and a Stanford University School of Medicine alumni, completed his psychiatry residency at the University of Pennsylvania School of Medicine, holding various prestigious positions in psychiatry and earning certification from the National Board of Psychiatry and Neurology.
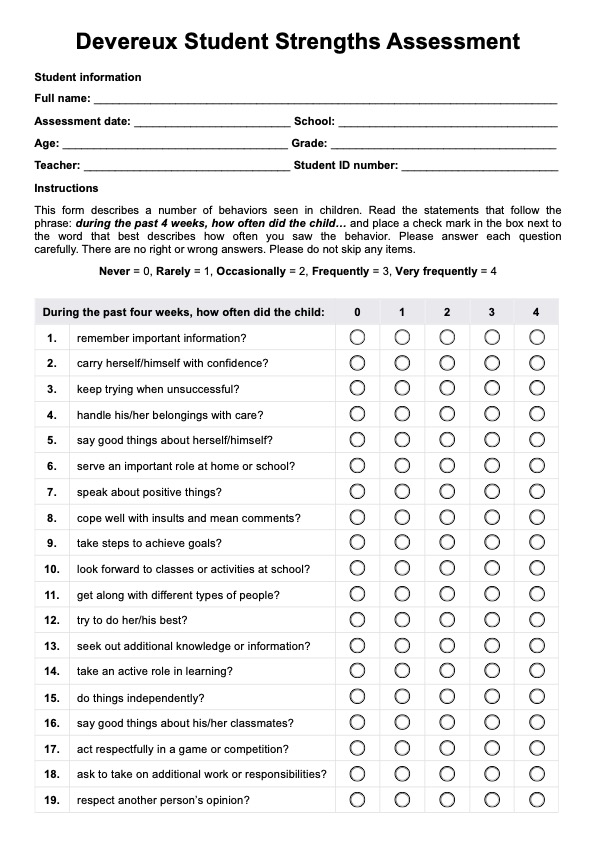
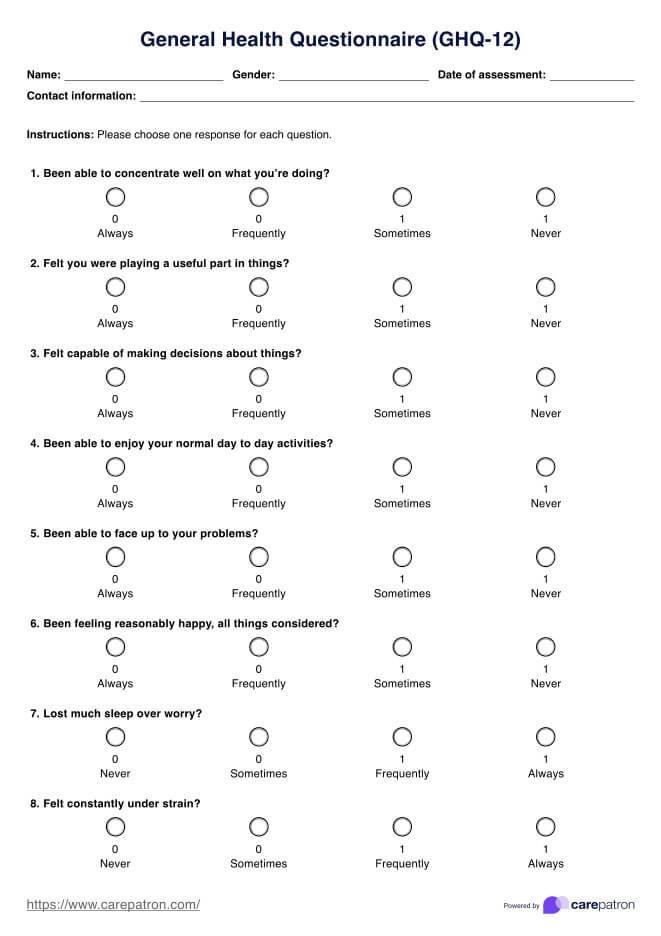
Patients self-report by answering the checklist consisting of 25 questions and a rating scale from 0 to 4, used to gauge the intensity of depressive symptoms experienced within the past week. It provides a brief evaluation of depression severity, ranging from the absence of symptoms to moderately severe depression in manifestation.
Designed for use in a primary care setting, this checklist assesses various symptoms of depression, such as mood, cognition, and physical symptoms, to aid in early detection and diagnosis. The checklist provides a structured approach for healthcare professionals to evaluate patient health and determine the need for further assessment or intervention.
Widely recognized as one of the depression screening tools, the Burns Depression Checklist helps clinicians identify individuals who may benefit from appropriate treatment for depression. Its systematic approach enhances the accuracy of diagnosis and facilitates timely interventions to improve patient outcomes in managing depressive symptoms.
How do you interpret the findings of this checklist?
Interpreting the results of the Burns Depression Checklist involves correlating the total score with the level of depression:
- Total score of 0-5 indicates no depression
- Scores ranging from 6-10 suggest a normal but unhappy mood
- A score of 11-25 signifies mild depression
- Scores between 26-50 indicate moderate depression
- Total scores of 51-75 represent severe depression
- Scores of 76-100 signify extreme depression
Primary care practitioners use these scores to gauge the severity of depressive symptoms, guide treatment decisions, and monitor progress over time, tailoring interventions to address the individual's specific needs.
Why is this checklist essential?
Utilizing the Burns Depression Checklist in primary care practices can significantly enhance patient care and outcomes by facilitating early detection and management of depressive symptoms. This assesses mood and related symptoms, providing valuable insights into patients' mental health status during primary care consultations.
To encourage family doctors
It encourages family doctors to routinely screen for depression during primary care visits, ensuring that mental health concerns are not overlooked. By integrating depression screening into regular assessments in most primary care consultations, healthcare providers can promptly identify individuals at risk and initiate appropriate interventions to improve outcomes.
To enhance primary care practices
Primary care plays a significant role in a patient's life. Incorporating the checklist into primary care practices enhances efficiency and accuracy in identifying key depression-related concerns. This allows healthcare providers to allocate resources effectively, prioritize follow-up care, and coordinate multidisciplinary interventions to address patients' mental health needs comprehensively.
To empower patients
By using the checklist, healthcare providers empower patients to actively participate in managing their mental health by fostering open communication and shared decision-making. Patients can feel validated and supported as their concerns are acknowledged and addressed. This results in improved treatment adherence and overall satisfaction with primary health care.
Major depressive disorder treatment
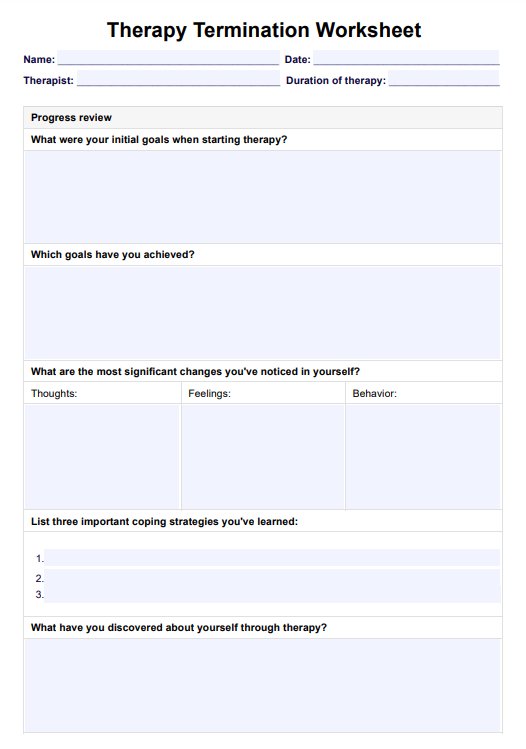
Recovering from MDD is rarely straightforward. It requires patience, resilience, and ongoing support from healthcare professionals, loved ones, and community resources. Recognizing that healing is a gradual process is part of the journey.
Once diagnosed, appropriate treatment for MDD typically involves a combination of psychotherapy, medication, and lifestyle modifications.
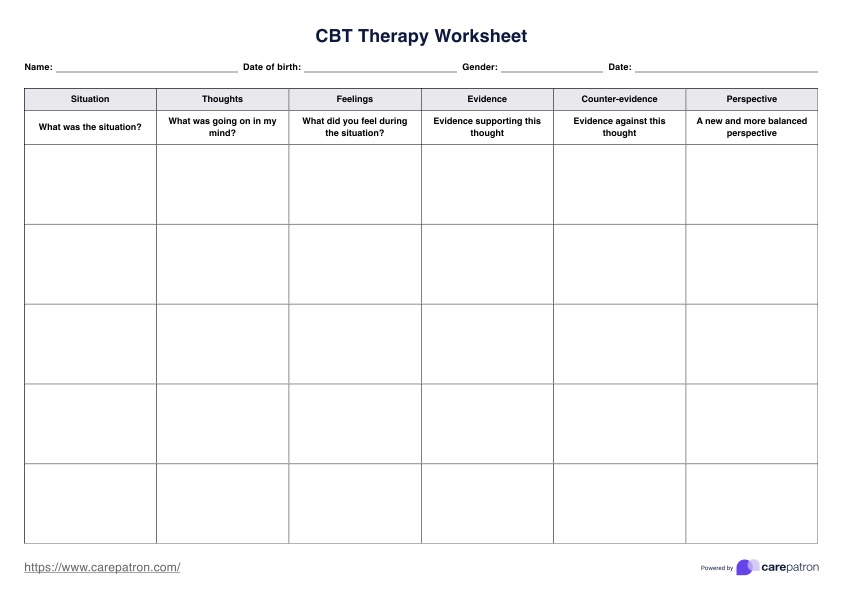
- Psychotherapy: Therapy sessions provide a supportive environment for individuals to explore their emotions. They include identifying negative thought patterns and developing coping strategies to manage their depression effectively.
- Medication: Antidepressants, which typically adjust neurotransmitter usage in the brain to regulate mood and behavior more effectively, should be prescribed by a certified professional.
- Lifestyle modifications: Lifestyle changes like regular exercise, adequate sleep, healthy eating habits, and stress management techniques can complement therapy and medication in treating depression by promoting overall well-being and resilience to stressors.
What are other examples of depression assessments?
Assessing depression is crucial in understanding and managing this complex mental health condition. Various current depression inventories are available for this purpose, each offering unique insights into an individual's depressive symptoms and severity.
- Beck Depression Inventory-II (BDI-II): The BDI-II is a self-report questionnaire developed by Dr. Aaron Beck that assesses the severity of depressive symptoms in adults and adolescents. It consists of 21 items covering various aspects of depression, such as mood, pessimism, and guilt, providing a quantitative measure of depression severity.
- Children's Depression Inventory (CDI2): Specifically designed by Maria Kovacs for children and adolescents aged 7 to 17, the CDI2 is a self-report questionnaire that evaluates depressive symptoms in this population. The full-length CDI2 comprises 28 items assessing mood, interpersonal relationships, and school performance, aiding in the early detection and management of depression in young individuals.
- Depression Anxiety Stress Scales (DASS-42): The DASS-42 is a comprehensive tool that assesses symptoms of depression, anxiety, and stress in adults. With 42 items divided into three subscales, it provides an understanding of an individual's emotional well-being, guiding tailored interventions for managing depressive symptoms alongside anxiety and stress.
- Hamilton Depression Rating Scale (HAM-D-21): The HAM-D-21 is a clinician-administered questionnaire used to assess the severity of depressive symptoms in adults. With 21 items covering various domains of depression, such as mood, guilt, and suicidal ideation, it aids in diagnosing depression and monitoring treatment response in clinical settings.
- Mood and Feelings Questionnaire (MFQ): Adrian Angold and Elizabeth J. Costello developed this tool for children and adolescents. MFQ is a self-report questionnaire that evaluates mood disturbances and depressive symptoms. Its 33 items assess a wide range of emotional experiences, providing valuable insights into the presence and severity of depression in young individuals.
Commonly asked questions
Depressive disorders can affect anyone, no matter the age, gender, or background. However, it's essential to recognize that depression can impact individuals of all demographics.
If a patient struggles with persistent sadness, hopelessness, or loss of interest in activities they once enjoyed, it's crucial to seek help from a healthcare professional. Additionally, seeking assistance is advisable if these symptoms interfere with daily functioning or last for more than two weeks.
Overcoming major depressive disorder often involves a combination of treatments, including therapy, medication, lifestyle modifications, and support from loved ones. Consider working closely with a healthcare provider to develop a personalized treatment plan.


















-template.jpg)