Vertigo Test
Assess for vertigo with our comprehensive Vertigo Test. Quick, accurate evaluation for symptoms like dizziness and balance issues.


What is vertigo?
Vertigo is a familiar yet often misunderstood sensation that can significantly disrupt daily life. Characterized by a spinning or swaying feeling, it stems from issues within the vestibular system, primarily the inner ear, which is responsible for balance. This sensation, distinct from lightheadedness or faintness, can be disorienting and frightening for those experiencing it.
One prevalent cause of vertigo is benign paroxysmal positional vertigo (BPPV), where tiny calcium carbonate crystals within the inner ear's semicircular canals become dislodged, triggering sudden episodes of vertigo with specific head movements. Symptoms of BPPV include brief episodes of dizziness triggered by changes in head position, such as rolling over in bed or looking up.
Peripheral vertigo, originating in the inner ear, is the most common type, often related to issues like BPPV, vestibular neuritis, or Meniere's disease. Conversely, central vertigo arises from disruptions in the central nervous system, such as brainstem or cerebellar lesions, or traumatic brain injury. Distinguishing between peripheral and central vertigo is crucial for accurate diagnosis and appropriate treatment.
When evaluating vertigo symptoms, clinicians often assess associated features, such as nystagmus (involuntary eye movements), hearing loss, and balance impairments. The Dix-Hallpike maneuver and the head impulse test are among the diagnostic tools commonly used to pinpoint the cause of vertigo.
Traumatic brain injury (TBI) can also lead to vertigo, either directly through damage to the inner ear structures or indirectly by affecting the brain regions responsible for processing balance signals. In cases of TBI-related vertigo, comprehensive evaluation and management by healthcare professionals specializing in both neurology and otolaryngology are essential.
What are the two types of vertigo?
Vertigo manifests in two primary forms: peripheral and central vertigo, each originating from distinct anatomical areas and presenting unique symptoms.
Peripheral vertigo, often stemming from issues within the inner ear or vestibular nerve, includes conditions like benign paroxysmal positional vertigo (BPPV), vestibular neuritis, and Meniere's disease. Symptoms typically involve a spinning sensation triggered by specific head movements, abnormal eye movements and possibly hearing loss. Clinicians diagnose peripheral vertigo through tests such as the Dix-Hallpike maneuver to elicit characteristic nystagmus.
On the other hand, central vertigo arises from disruptions in the central nervous system, including the brainstem or cerebellum, often due to conditions like traumatic brain injury or stroke. Symptoms may be more persistent and severe, potentially accompanied by other neurological deficits. Diagnosing central vertigo requires a comprehensive evaluation, including imaging studies like magnetic resonance imaging (MRI) to identify underlying brain abnormalities.
Regardless of the type, accurate diagnosis is crucial for effective vertigo treatment. Healthcare providers, including otolaryngologists and neurologists, utilize various diagnostic tests to assess vestibular function and differentiate between peripheral and central causes, ultimately guiding appropriate management strategies for individuals experiencing vertigo symptoms.
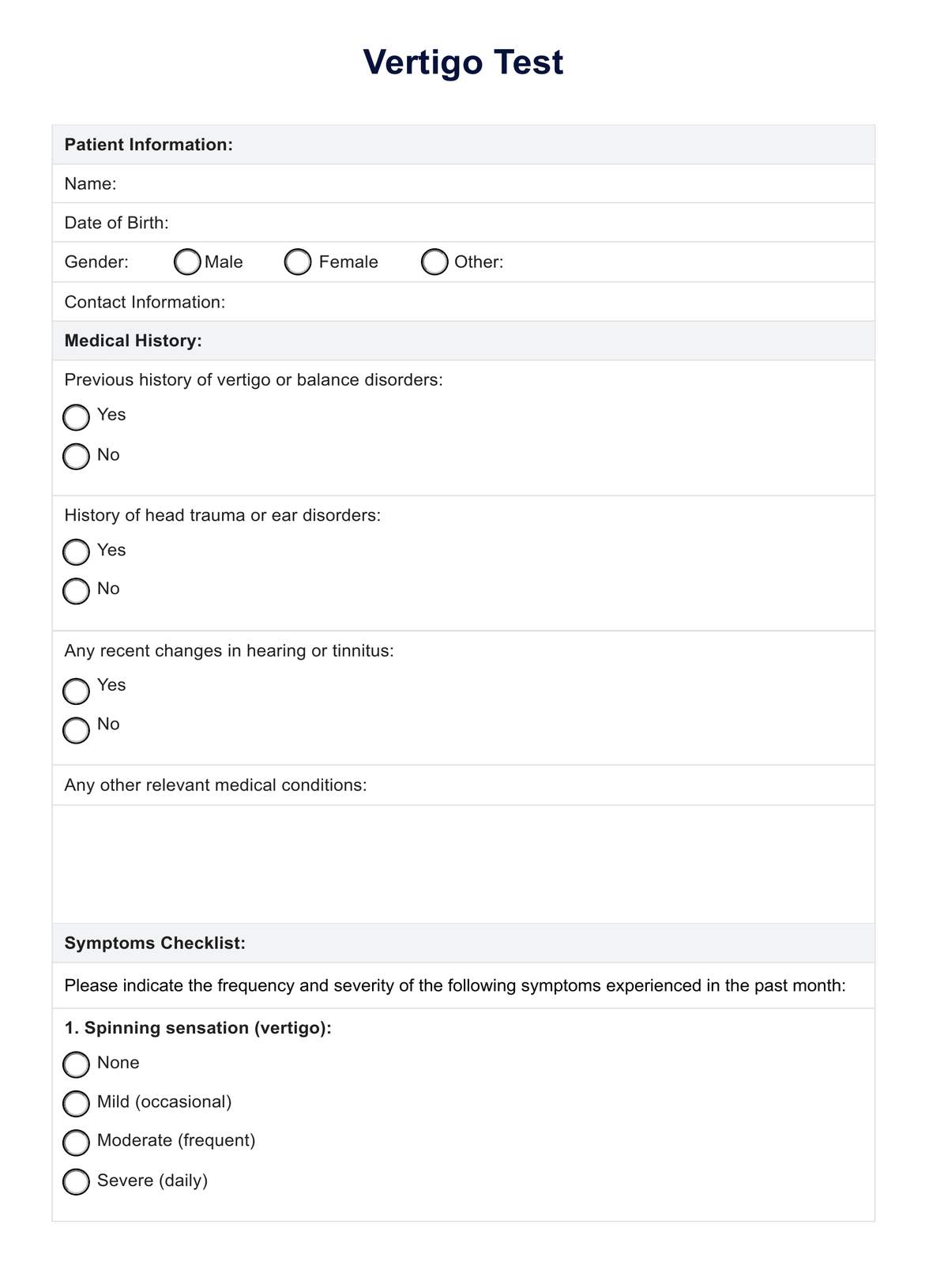
Vertigo Test Template
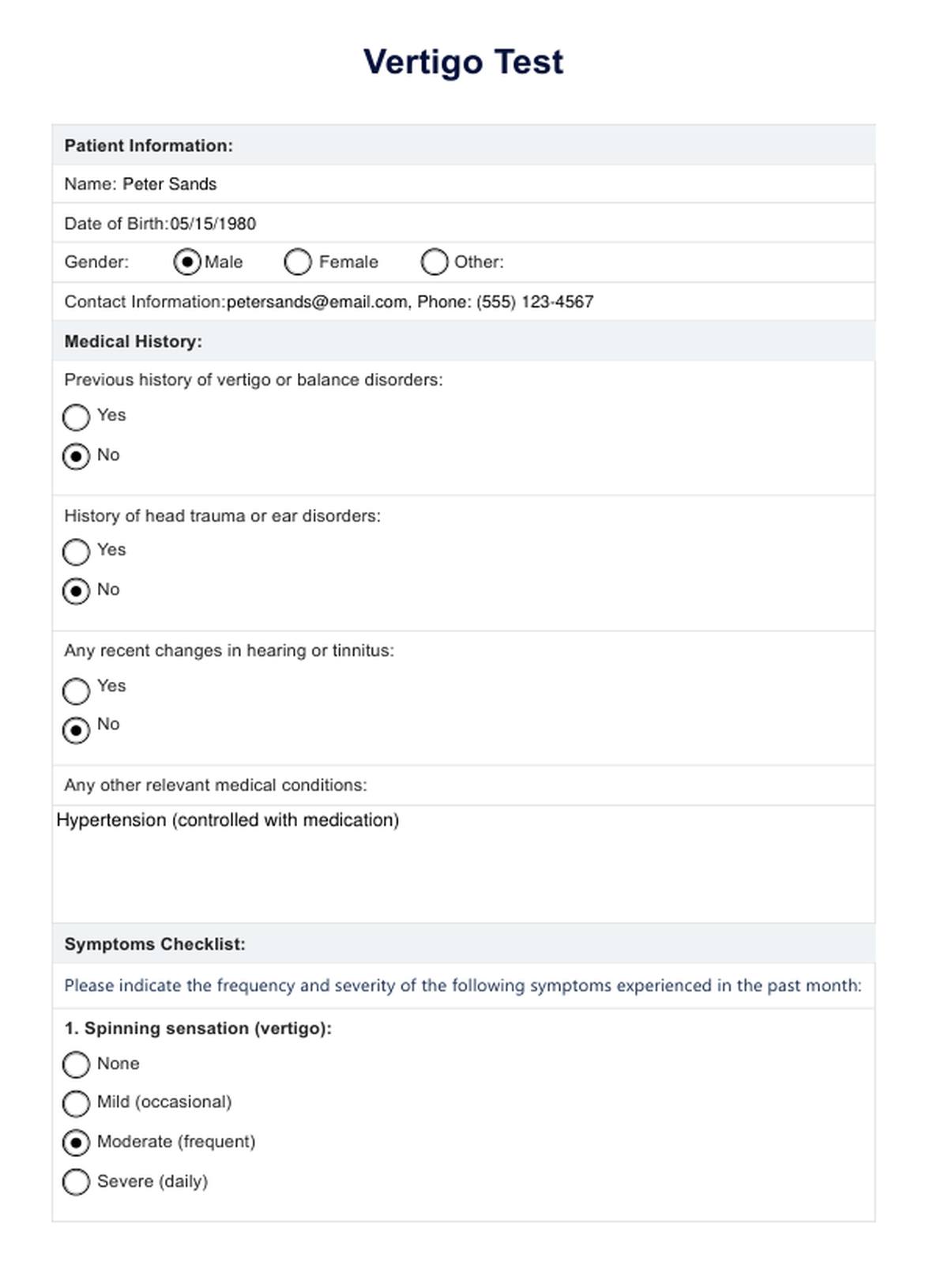
Vertigo Test Example
What are the symptoms of vertigo?
Here are some of the symptoms of vertigo:
Spinning sensation
The hallmark symptom of vertigo is a spinning sensation as if the environment is whirling around or the individual is rotating. This sensation can be intense and debilitating, leading to disorientation and imbalance.
Abnormal eye movements
Vertigo often accompanies rapid eye movements, known as nystagmus, which may occur in response to changes in head position or as a reflex function of the vestibular system. Observing and recording these eye movements is crucial for diagnosis during a physical examination.
Balance problems
Individuals with vertigo may experience difficulty maintaining balance, especially when standing or moving. This imbalance can lead to falls or feelings of unsteadiness, affecting spatial awareness and daily activities.
Nausea and vomiting
Vertigo-induced nausea and vomiting are common symptoms, often triggered by the disorienting sensations caused by the inner ear disorder. These symptoms can be distressing and may worsen the overall sense of discomfort.
Sensitivity to movement
Vertigo sufferers may become more sensitive to certain movements, particularly those involving changes in head position. Even minor shifts in posture or orientation can exacerbate symptoms and trigger vertigo episodes.
Hearing loss or tinnitus
In some cases, vertigo may be accompanied by hearing loss or ringing in the ears (tinnitus), indicating possible involvement of the inner ear structures. Hearing tests may be necessary to assess auditory function and identify related health conditions.
What are the causes of vertigo?
Understanding the myriad causes of vertigo is crucial for accurate diagnosis and effective management. Here's a comprehensive list:
- Benign paroxysmal positional vertigo (BPPV): Dislodged calcium carbonate crystals in the inner ear can trigger brief episodes of vertigo with specific head movements.
- Vestibular neuritis: Inflammation of the vestibular nerve, typically viral in origin, leading to sudden vertigo attacks.
- Meniere's disease: Fluid buildup in the inner ear can cause recurrent vertigo, hearing loss, and tinnitus.
- Labyrinthitis: Inner ear infection resulting in vertigo, often accompanied by hearing loss and nausea.
- Traumatic brain injury (TBI): Head trauma can disrupt the vestibular system, leading to vertigo and imbalance.
- Medication side effects: Certain medications, such as those for blood pressure or anxiety, may induce vertigo as a side effect.
- Anxiety and panic disorders: Psychological factors can contribute to feelings of dizziness and vertigo, particularly in stressful situations.
- Vascular disorders: Reduced blood flow to the inner ear or brain can lead to vertigo episodes.
- Otosclerosis: Abnormal bone growth in the middle ear can affect hearing and balance, leading to vertigo.
- Mal de debarquement syndrome (MdDS): Persistent sensation of rocking or swaying after disembarking from a vehicle or boat.
- Peripheral neuropathy: Damage to nerves outside the central nervous system can affect balance and contribute to vertigo.
- Psychiatric disorders: Conditions like depression or somatization disorder may manifest with vertigo symptoms.
By recognizing the diverse potential causes, healthcare providers can perform targeted diagnostic tests, such as Dix-Hallpike maneuvers, audiometric tests, and MRI scans, to accurately diagnose and manage vertigo in patients.
Diagnosing vertigo
Diagnosing vertigo requires a multifaceted approach to unravel the underlying causes behind this perplexing sensation. Healthcare providers embark on a journey akin to detective work, piecing together clues from patient history, symptoms, and diagnostic tests to arrive at a precise diagnosis.
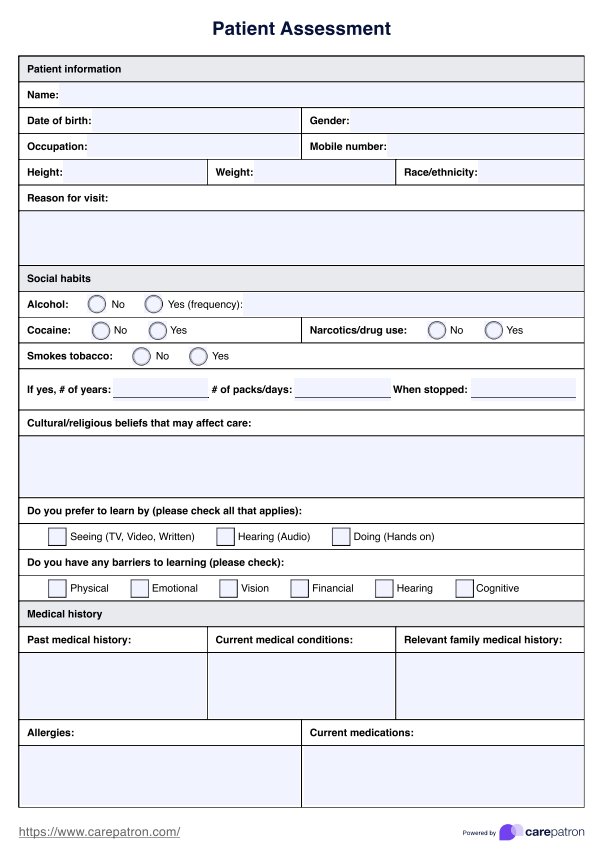
The initial step in diagnosing vertigo involves a comprehensive patient history assessment. Healthcare providers delve into the frequency, duration, and characteristics of vertigo episodes, as well as any accompanying symptoms like nausea, abnormal eye movements (nystagmus), or hearing disturbances. Identifying any precipitating factors or associated medical conditions is crucial in narrowing down the potential causes.
Physical examination techniques play a pivotal role in diagnosing vertigo, with maneuvers like the Dix-Hallpike test used to provoke characteristic nystagmus indicative of peripheral vestibular dysfunction, such as benign paroxysmal positional vertigo (BPPV). Additionally, assessing balance, gait, and neurological function provides valuable insights into the vestibular system's integrity and central nervous system involvement.
Diagnostic tests further elucidate the underlying etiology of vertigo. Audiometric tests evaluate auditory function, ruling out hearing loss or inner ear abnormalities. Advanced imaging modalities like magnetic resonance imaging (MRI) may be utilized to investigate central causes of vertigo, such as brainstem lesions or tumors.
Collaboration among healthcare providers, including otolaryngologists, neurologists, and physical therapists, enhances diagnostic accuracy and ensures comprehensive care for patients experiencing vertigo. By employing a systematic approach encompassing patient history, physical examination, and diagnostic tests, healthcare providers can unravel the mysteries of vertigo and guide patients toward effective treatment strategies, ultimately restoring their equilibrium and quality of life.
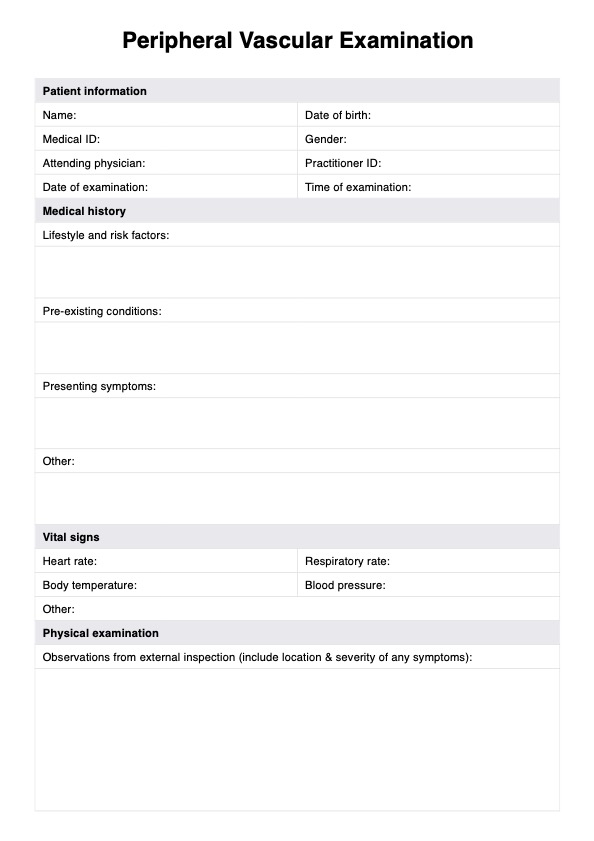
How does this Vertigo Test work?
The Vertigo Test is a valuable tool for healthcare practitioners in assessing and diagnosing vertigo in patients. Here's how it works:
Step 1: Patient information collection
Healthcare providers gather essential patient demographics and medical history, including previous vertigo episodes, head trauma, and ear disorders. This information provides crucial context for interpreting symptoms and selecting appropriate diagnostic tests.
Step 2: Symptoms checklist
Patients are asked to indicate the frequency and severity of vertigo symptoms, including spinning sensation, abnormal eye movements (nystagmus), balance problems, nausea or vomiting, sensitivity to movement, and hearing loss or tinnitus. This checklist helps quantify symptoms and guide further evaluation.
Step 3: Diagnostic test selection
Based on reported symptoms and medical history, healthcare providers determine the diagnostic tests needed to confirm or rule out specific causes of vertigo. These may include the Dix-Hallpike maneuver, head impulse test, audiometric tests, and MRI scans to assess vestibular function and identify underlying pathology.
Step 4: Test interpretation
Results from diagnostic tests are carefully interpreted to ascertain the presence of peripheral or central vertigo, determine the underlying etiology, and guide treatment decisions. Observation of nystagmus during positional maneuvers like the Dix-Hallpike test may indicate benign paroxysmal positional vertigo (BPPV), while abnormalities on MRI scans may suggest central nervous system involvement.
Step 5: Treatment recommendations
Based on the diagnostic findings, healthcare providers recommend appropriate treatment options, such as canalith repositioning procedures for BPPV, vestibular rehabilitation exercises, medication, or referral to specialists for further evaluation and management.
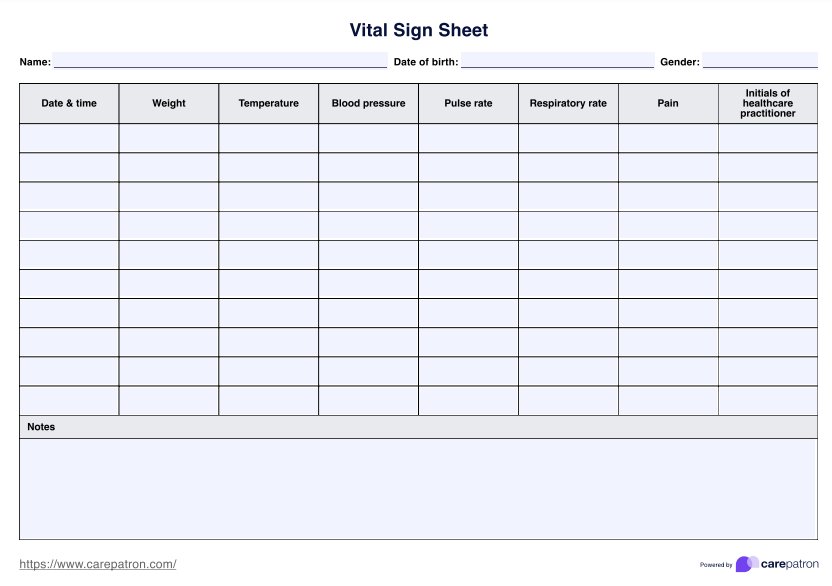
Step 6: Follow-up
Patients are scheduled for follow-up appointments to monitor treatment response, adjust management strategies as needed, and address any ongoing concerns. Continuous communication between patients and healthcare providers ensures optimal care and symptom management.
How are the results of this Vertigo Test interpreted?
Interpreting the results of the Vertigo Test involves a meticulous analysis of patient history, reported symptoms, and diagnostic test findings. For each result:
- Peripheral vertigo: If symptoms like positional vertigo and nystagmus are present, peripheral vertigo, such as benign paroxysmal positional vertigo (BPPV) or vestibular neuritis, may be suspected. Positive findings on the Dix-Hallpike maneuver indicate BPPV, while vestibular neuritis may present with abnormal head impulse test results.
- Central vertigo: Abnormalities on MRI scans or persistent vertigo despite negative positional tests suggest central vertigo, potentially indicative of brainstem lesions or cerebellar dysfunction. Further evaluation by a neurologist may be warranted to explore underlying central nervous system pathology.
- Mixed or atypical presentation: In some cases, patients may exhibit symptoms suggestive of peripheral and central involvement or present with atypical features. These cases require careful consideration and may necessitate additional diagnostic tests or specialist consultation for accurate diagnosis and tailored treatment approaches.
By meticulously analyzing each result and considering the broader clinical context, healthcare providers can formulate precise diagnoses and develop personalized treatment plans to manage vertigo and improve patient outcomes effectively.
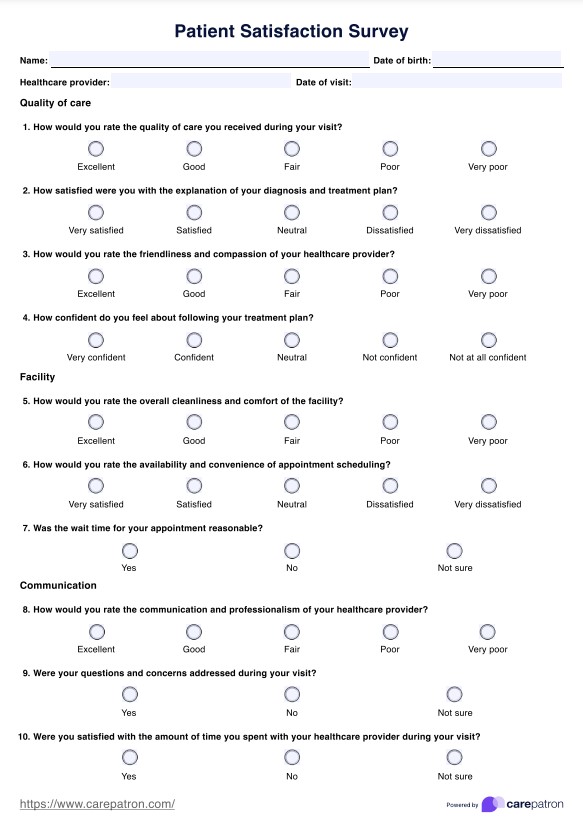
What are the benefits of our free Vertigo Test?
Here are some of the benefits of our free Vertigo Test template:
- Accurate diagnosis: The Vertigo Test helps pinpoint the underlying cause of vertigo, facilitating targeted treatment and symptom management.
- Tailored treatment: Healthcare providers can recommend personalized treatment options for optimal outcomes by identifying the specific type of vertigo.
- Early intervention: Prompt diagnosis through the Vertigo Test allows for timely initiation of treatment, preventing complications and improving patient prognosis.
- Symptom relief: Effective management strategies based on test results can alleviate vertigo symptoms, enhancing patient comfort and quality of life.
- Prevention of falls: Addressing balance problems identified through the Vertigo Test can reduce the risk of falls and related injuries in vertigo sufferers.
- Peace of mind: Knowing the precise diagnosis of vertigo reassures patients and empowers them to participate actively in their treatment journey.
- Long-term management: Regular monitoring and follow-up based on Vertigo Test results allow for ongoing management and adjustment of treatment plans as needed to maintain symptom control.
Commonly asked questions
A vertigo test is a diagnostic assessment used by healthcare practitioners to evaluate and diagnose vertigo, a spinning sensation or dizziness.
A vertigo test may involve a combination of patient history assessment, physical examination maneuvers (such as the Dix-Hallpike test), and diagnostic tests (such as audiometric tests or MRI scans).
Common symptoms of vertigo include a spinning sensation, balance problems, nausea or vomiting, sensitivity to movement, abnormal eye movements (nystagmus), and hearing loss or tinnitus.