Discharge Planning Checklist
Download our free Discharge Planning Checklist Template to streamline the transition process for patients leaving a healthcare facility.


What is discharge planning?
Discharge planning is a critical process where hospital staff develops a personalized plan assessing a patient's health and social needs prior to their hospital discharge (Gonçalves-Bradley et al., 2022). This plan ensures a smooth transition from the hospital to home or another care setting, facilitating the continuation of care and preventing complications. Effective discharge planning involves a comprehensive evaluation by healthcare providers, including the attending physician, to ensure the patient can safely leave the hospital.
Discharge planning may include arranging follow-up care such as physical therapy, wound care, and medical appointments. It may also require coordinating skilled nursing services or other personal care resources and ensuring the patient has the necessary medical equipment (Patel & Bechmann, 2023). Discharge instructions typically cover medication management, potential complications, and necessary lifestyle adjustments.
Discharge planning aims to support health and recovery and reduce the likelihood of hospital readmissions, which can incur financial penalties for healthcare institutions. A well-communicated discharge plan is essential for continuity of care and helps ensure that patients and their caregivers understand how to effectively manage their care at home.
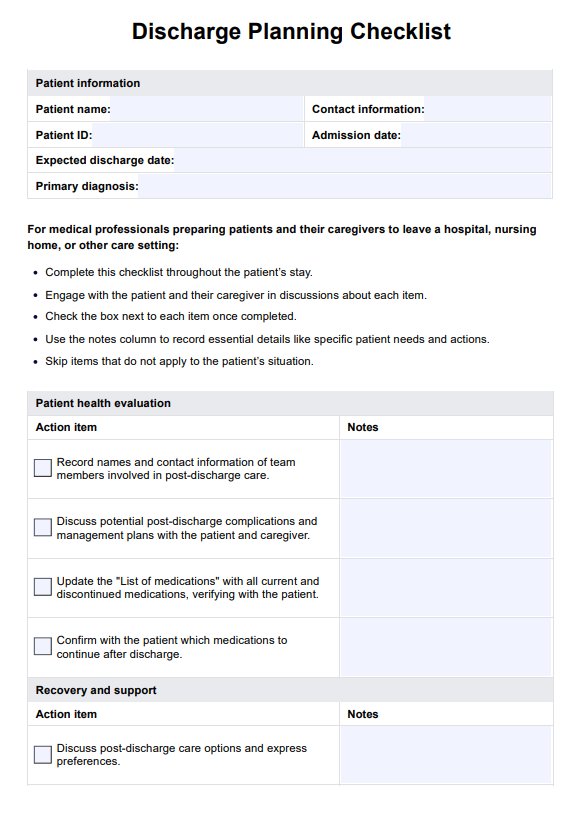
Discharge Planning Checklist Template
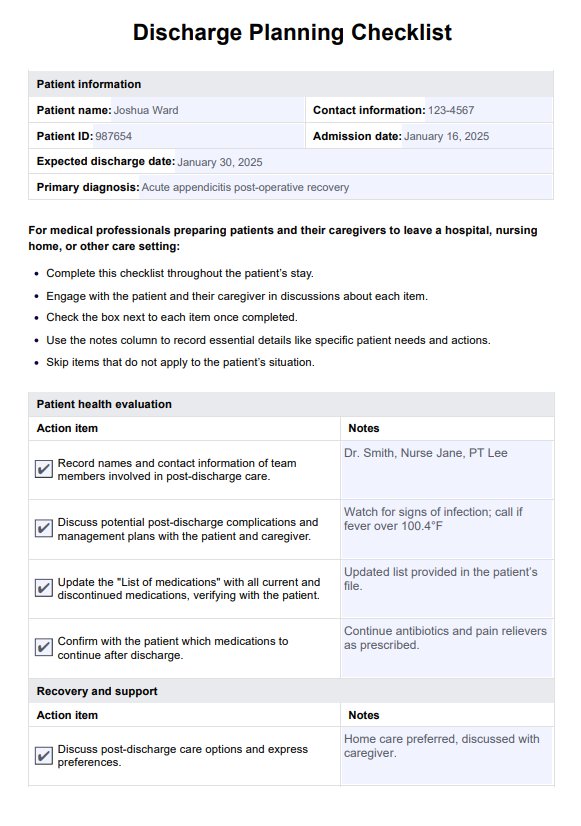
Discharge Planning Checklist Example
What is a discharge planning checklist?
A discharge planning checklist is a structured tool used by healthcare professionals to ensure all necessary preparations for a patient’s safe and effective transition from a hospital or care setting to a home or another facility. This checklist covers a comprehensive range of actions, from updating patient information and assessing patient health needs to setting up follow-up care like doctor's appointments and physical therapy.
Key components include coordinating with other involved health care providers, discussing durable medical equipment needs, and ensuring that any changes in medication are clearly communicated and understood.
The checklist also prompts discussions about the patient's ability to perform daily activities, the need for support groups, and access to community resources. It compiles a thorough discharge summary, including details such as the patient's health status, care instructions, and required home health services. This proactive approach facilitates continuity of care, minimizes the risk of readmission, and supports the patient’s recovery and well-being in their own environment.
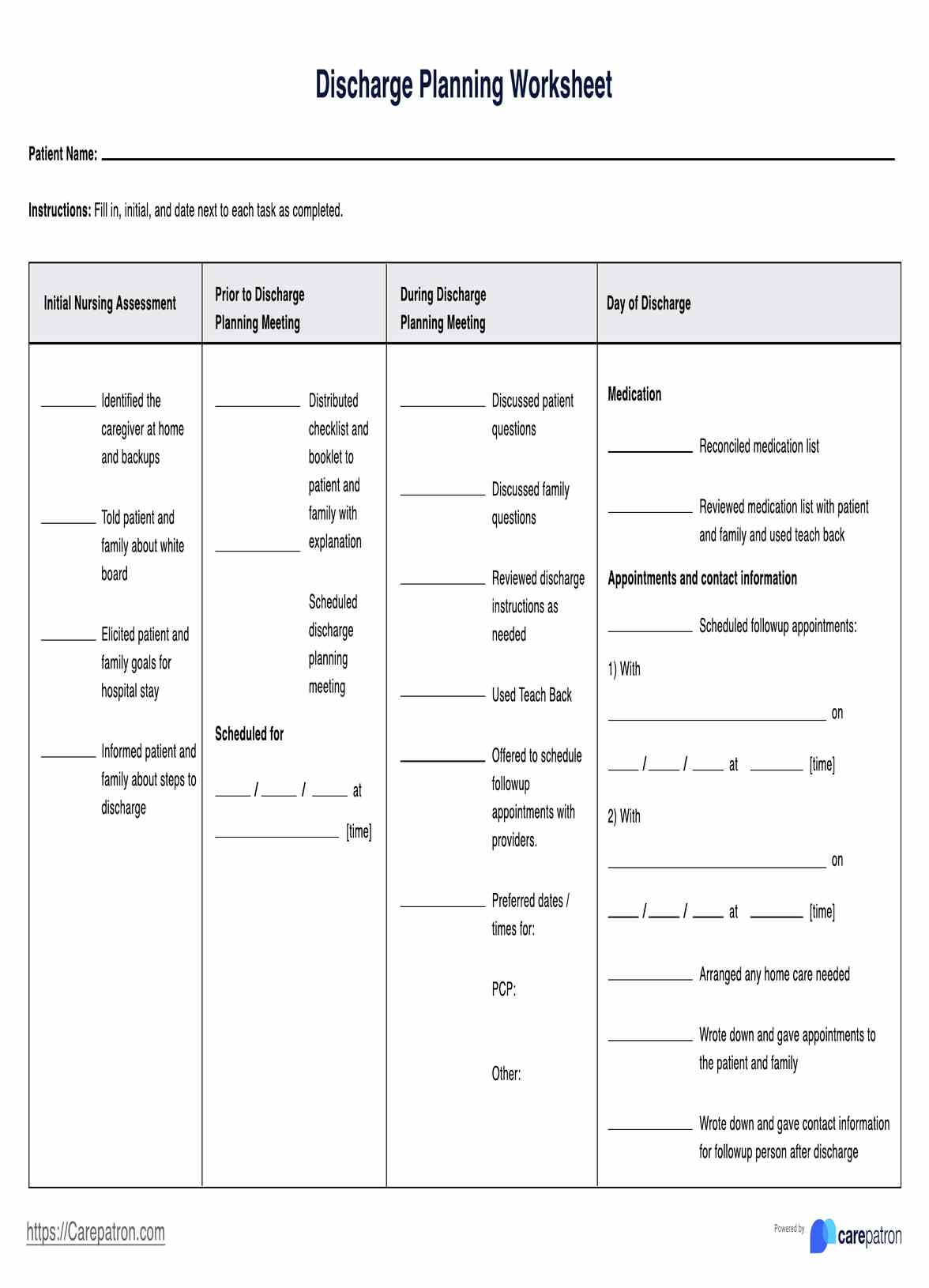
How does our Discharge Planning Checklist Template work
Discharge planning is essential in healthcare to ensure patients transition smoothly from care facilities to home. Carepatron provides a user-friendly checklist to streamline this process.
Step 1: Access and use the template
Click the "Use template" button to access the discharge planning checklist directly in the Carepatron app. This action will seamlessly guide you into the app so you can start tailoring the checklist for your patient's specific needs.
Step 2: Introduce the checklist to the patient
Introduce the checklist early during the patient’s stay to align expectations and ensure they understand the process. This step enhances the patient's engagement and compliance with the discharge plan.
Step 3: Utilize the checklist to arrange patient's discharge
Employ the checklist to methodically organize all aspects of the patient's discharge, from confirming medical equipment to scheduling follow-up care. This ensures no detail is overlooked.
Step 4: Provide patient education and next steps
Use the discharge checklist to educate the patient and their caregivers about post-discharge activities, such as medication management, home care instructions, and scheduling future appointments. This empowers them to manage their recovery effectively.
Benefits of using this Discharge Planning Checklist Template
For medical professionals, the discharge planning checklist is an invaluable tool that streamlines the complexities of care transitions. It ensures that every critical aspect of discharge is systematically addressed, reducing the risk of oversight and enhancing the quality of care provided. By using this checklist, discharge planners and care managers can effectively monitor and manage medication changes, including introducing new medications, which are pivotal in preventing adverse effects and ensuring continuity of care.
The checklist facilitates coordinating various services and appointments necessary for a smooth transition. It aids in accurately communicating new diagnoses and treatment plans to all involved healthcare providers and social services, ensuring that each party is informed and prepared to continue the care journey. This coordination is crucial, particularly when patients require complex care management involving multiple specialties.
Furthermore, the checklist is a communication bridge between healthcare providers and care managers, enabling a clear and comprehensive understanding of the patient’s needs. It helps in setting up follow-up appointments, connecting patients with necessary social services, and ensuring that all parties know the specifics of the care plan. For medical professionals, using this checklist means enhanced efficiency, improved patient outcomes, and a more seamless process of managing the detailed requirements of patient discharges.
References
Gonçalves-Bradley, D. C., Lannin, N. A., Clemson, L. M., Cameron, I. D., & Shepperd, S. (2022). Discharge planning from hospital. The Cochrane Database of Systematic Reviews, 2(2). https://doi.org/10.1002/14651858.cd000313.pub6
Patel, P., & Bechmann, S. (2023, April 3). Discharge planning. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK557819/
Commonly asked questions
The discharge planning process is a coordinated activity that prepares patients to leave a hospital or care facility and helps them transition safely back to their home environment or to another level of care. It involves evaluating the patient's specific healthcare needs and organizing the necessary support systems to ensure continuity of care and prevent readmission.
The 5 D's of discharge are key components that ensure a safe and effective transition from hospital to home: Diagnosis, Duration, Drugs, Devices, and Diet. These elements address the patient's condition, treatment duration, medication management, necessary medical equipment, and dietary restrictions or needs.
A discharge plan should include a comprehensive summary of the patient’s hospitalization, a detailed medication plan, follow-up care instructions, a list of potential signs of complications, and contact information for essential services. It should also address the patient's ability to perform daily activities and any support they might need at home.