Diabetes Mellitus Nursing Care Plan
Download our Diabetes Mellitus Nursing Care Plan Template to enhance patient care with structured assessments, personalized interventions, and comprehensive diabetes management.


What is diabetes mellitus?
Diabetes mellitus is a chronic condition where the body struggles to maintain blood glucose levels due to insufficient insulin (Type 1 diabetes) or insulin resistance (Type 2 diabetes). Insulin is crucial for moving blood glucose into cells, so when its function is impaired, this results in high blood sugar, which leads to various health complications. Effective diabetes management often includes a structured diabetes mellitus care plan to stabilize blood glucose and prevent further issues.
Causes of diabetes mellitus
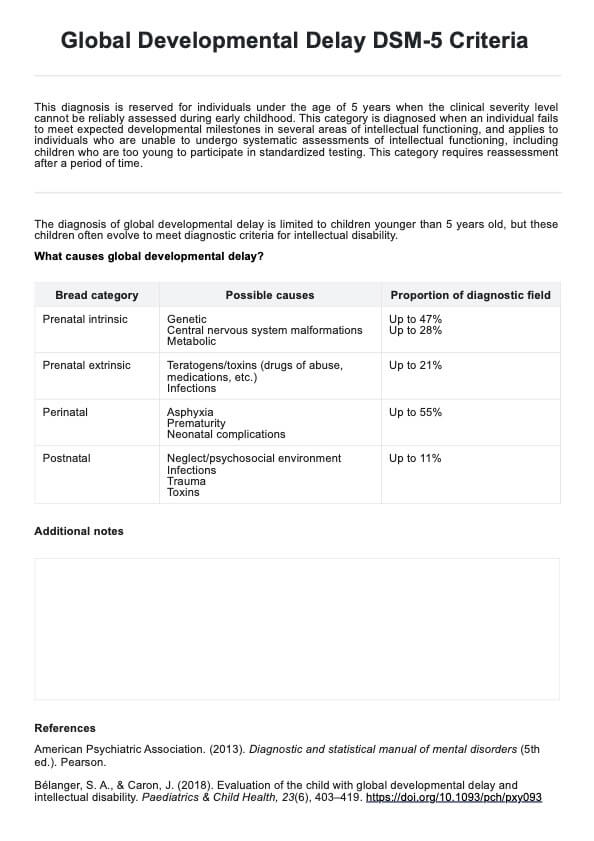
The causes of diabetes mellitus vary, with different risk factors affecting blood glucose regulation:
Type 1 diabetes
In Type 1 diabetes, an autoimmune response damages the insulin-producing cells, leading to low insulin levels and poor blood glucose control. Genetic factors and certain viral infections are key risk factors. Managing this type often requires insulin injections to maintain target blood glucose levels.
Type 2 diabetes
Type 2 diabetes is marked by insulin resistance, making it difficult for cells to use insulin effectively. Key risk factors include obesity, sedentary lifestyle, and genetics. Diabetes management for Type 2 focuses on blood glucose monitoring, lifestyle adjustments, and sometimes medication to reduce associated risks, such as cardiovascular disease.
Gestational diabetes
Gestational diabetes arises during pregnancy due to hormone changes that heighten insulin resistance. Risk factors include obesity and advanced maternal age, making blood glucose control critical to minimize risks to both mother and child.
Symptoms of diabetes mellitus
Recognizing diabetes symptoms early helps maintain blood glucose levels and reduce complications.
- Common symptoms: Frequent urination, excessive thirst, hunger, unintended weight loss, and fatigue are expected as the body attempts to manage excess blood glucose.
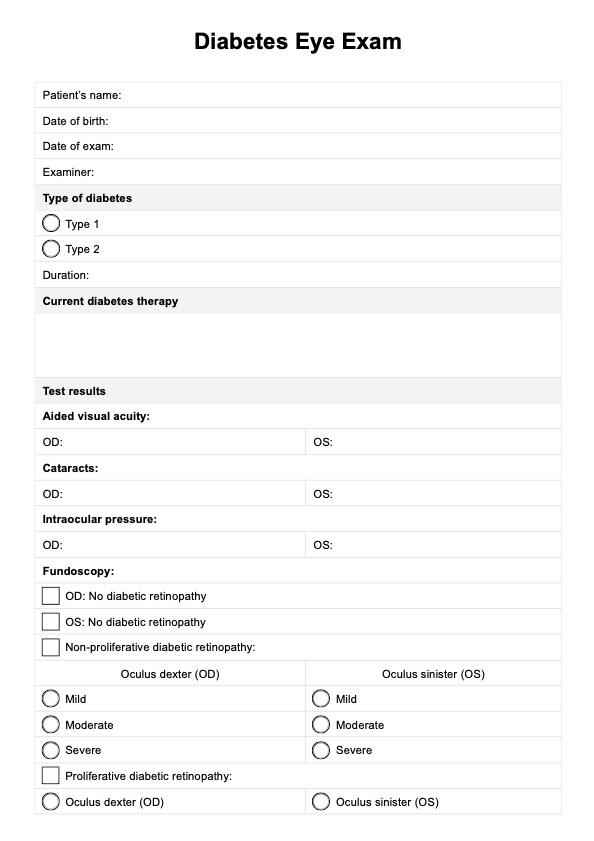
- Other symptoms: Diabetes can cause blurred vision, slow-healing wounds, and tingling or numbness, often due to poor circulation and nerve function.
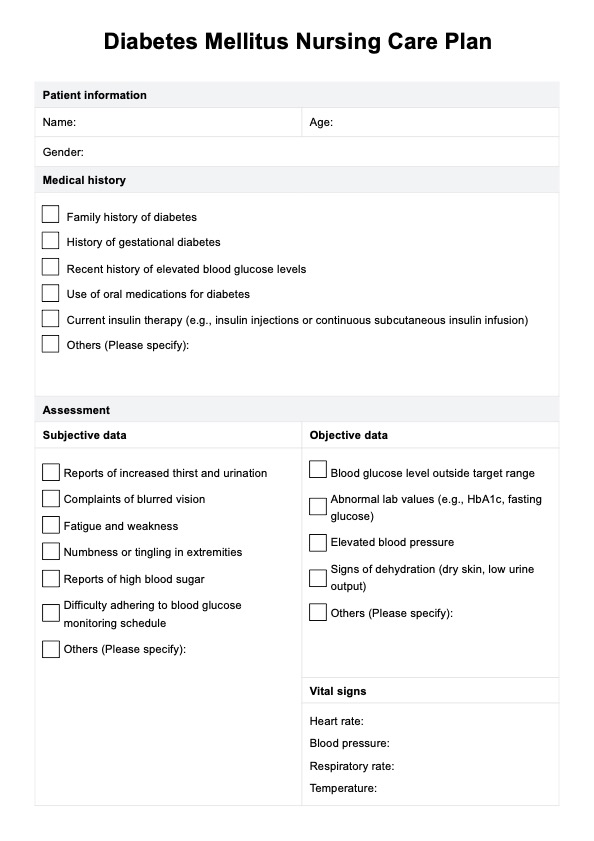
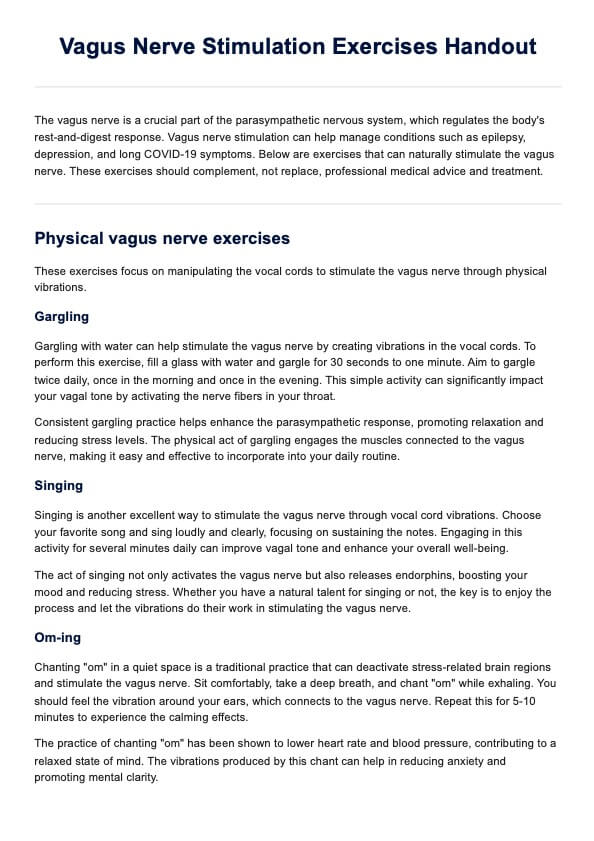
Diabetes Mellitus Nursing Care Plan Template
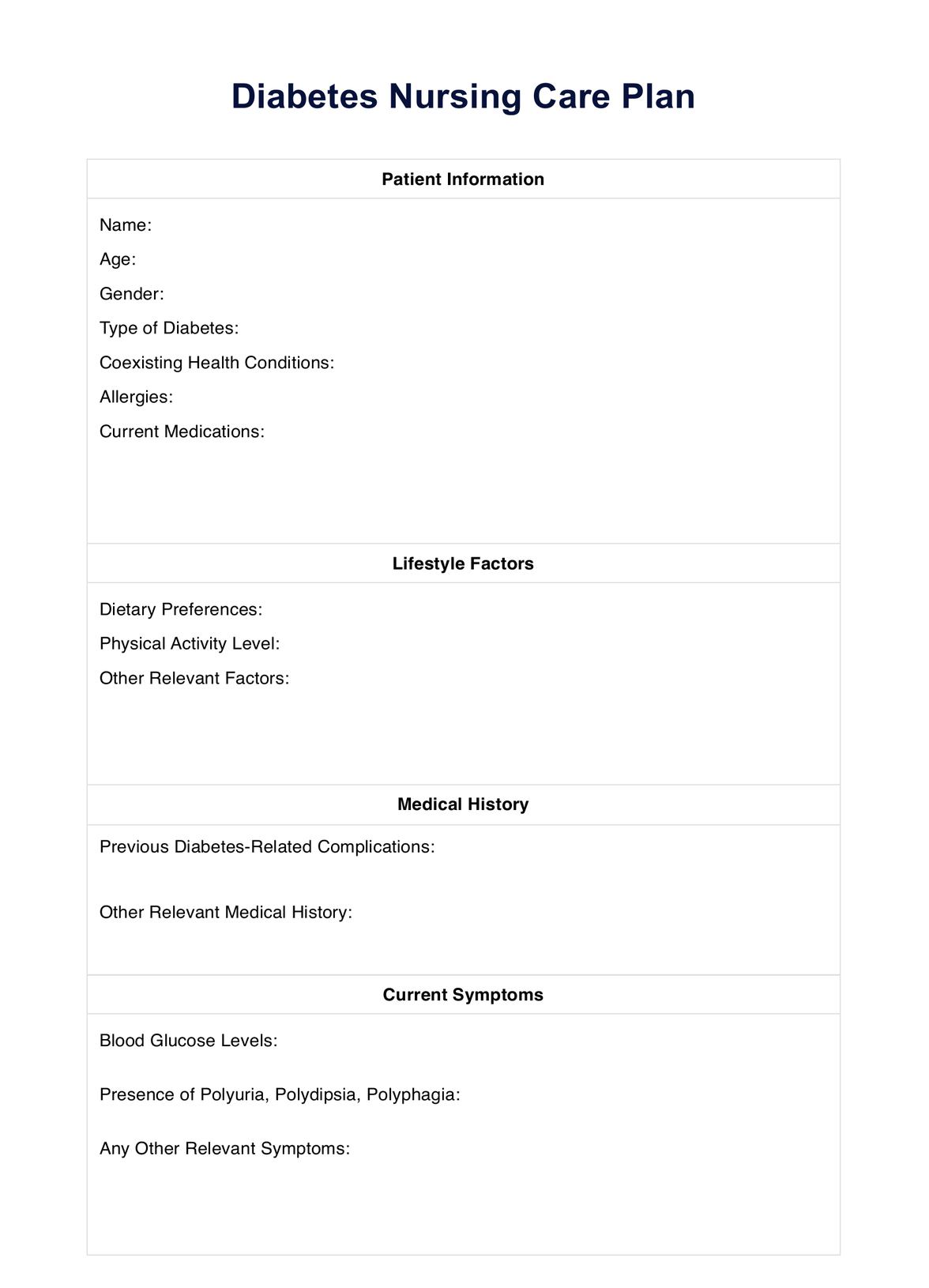
Diabetes Mellitus Nursing Care Plan Example
How does it work?
Here's a quick reference for effectively using the Diabetes Mellitus Nursing Care Plan Template for patient care.
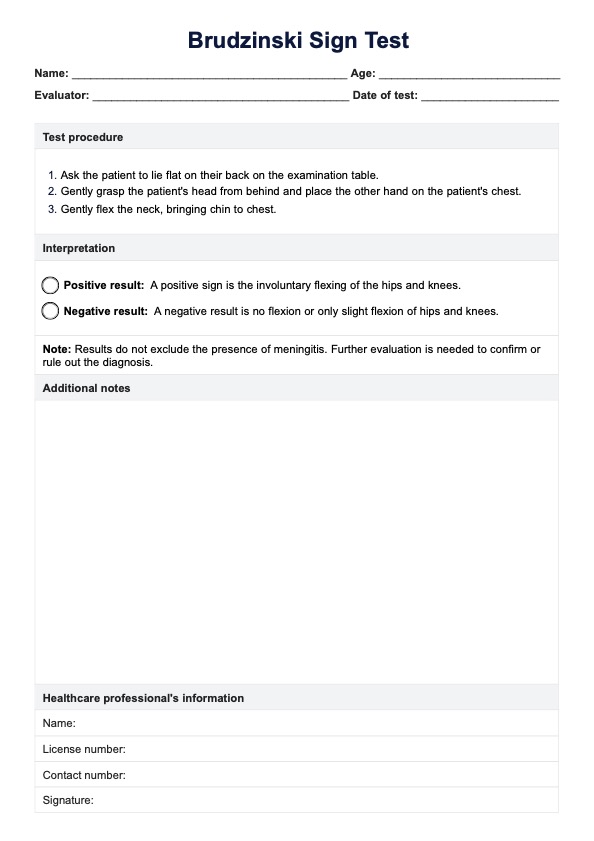
Step 1: Download the template
Begin by downloading the Diabetes Mellitus Nursing Care Plan Template. You can access it on Carepatron’s website or app by selecting “Download Template” or “Use Template” or by typing "Diabetes Mellitus Nursing Care Plan" into the template library search bar.
Step 2: Gather patient information
Start by completing the patient’s basic information in the template, including medical history and current assessments. Ensure details like insulin doses, blood glucose levels, and risk factors are accurately documented to support individualized care planning.
Step 3: Perform a comprehensive assessment
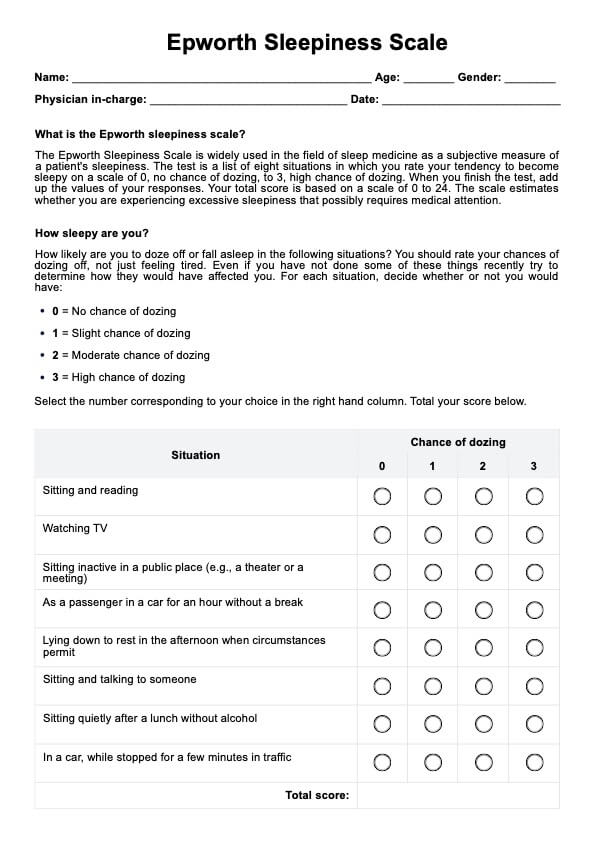
Conduct a full patient assessment, noting subjective symptoms (like fatigue and thirst) and objective signs (such as elevated blood glucose and blood pressure). Record all relevant vital signs to create a clear picture of the patient's health status.
Step 4: Define nursing diagnosis, goals, and interventions
Based on your assessment, establish nursing diagnoses and short- and long-term goals for optimal blood glucose control. Outline necessary nursing interventions like blood glucose monitoring, administration of oral medications, insulin administration or insulin therapy, and patient education on diabetes self-care.
Step 5: Store and secure the care plan
Once complete, save the care plan in Carepatron’s HIPAA-compliant software to ensure secure access. This centralized storage keeps the Diabetes Mellitus Nursing Care Plan accessible to the healthcare team, supporting coordinated and secure care for the patient.
When would you use this template?
This template can be used alongside other resources, such as diabetes mellitus care plans and hyperglycemia nursing care plans, to monitor and improve patient help. This Diabetes Mellitus Nursing Care Plan Template is also helpful in the following situations:
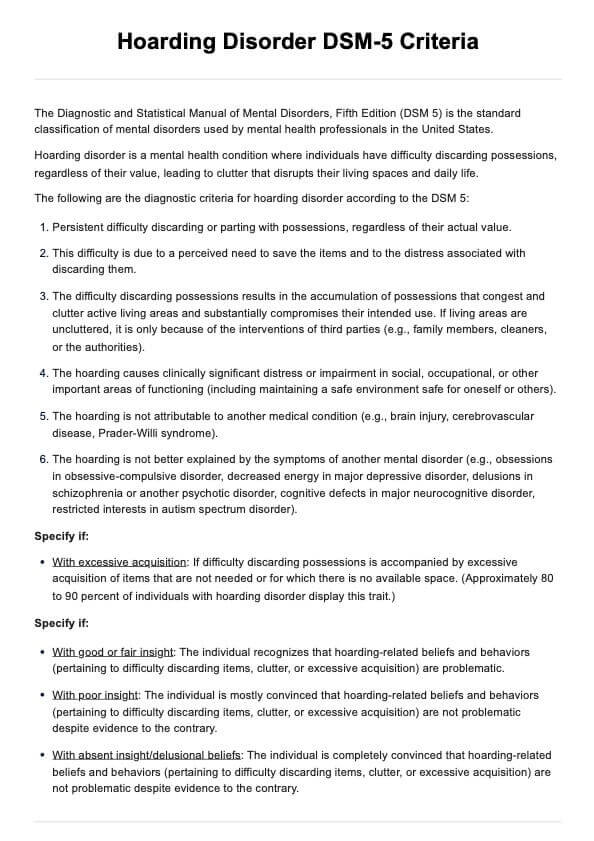
Newly diagnosed patients
For individuals recently diagnosed with diabetes, educating the patient about their condition and the importance of monitoring blood glucose is essential. A care plan assists them in understanding how to manage their health, including lifestyle changes, carbohydrate counting, and maintaining a healthy weight.
Patients with poorly controlled blood sugar levels
Patients experiencing unstable blood glucose levels require a tailored care plan emphasizing regular blood glucose monitoring. This includes tracking blood glucose readings and potential adjustments to their medication or lifestyle to help control blood glucose effectively and prevent complications like heart disease.
Patients with complications
Individuals with diabetes-related complications, such as neuropathy or diabetic retinopathy, benefit from specialized care plans that focus on managing these issues. Care plans aim to prevent further deterioration of blood vessels and improve quality of life while monitoring conditions like high blood pressure.
Patients undergoing surgery or hospitalization
For patients undergoing surgery or experiencing hospitalization, a structured care plan is vital for managing blood glucose fluctuations and ensuring optimal insulin pump therapy or insulin injection administration during recovery. This plan aids in transitioning back to regular care while maintaining normal range blood glucose levels.
Benefits of using our Diabetes Mellitus Nursing Care Plan Template
Using our Diabetes Mellitus Nursing Care Plan template offers numerous advantages for healthcare practitioners managing patients with diabetes. Here are some key benefits:
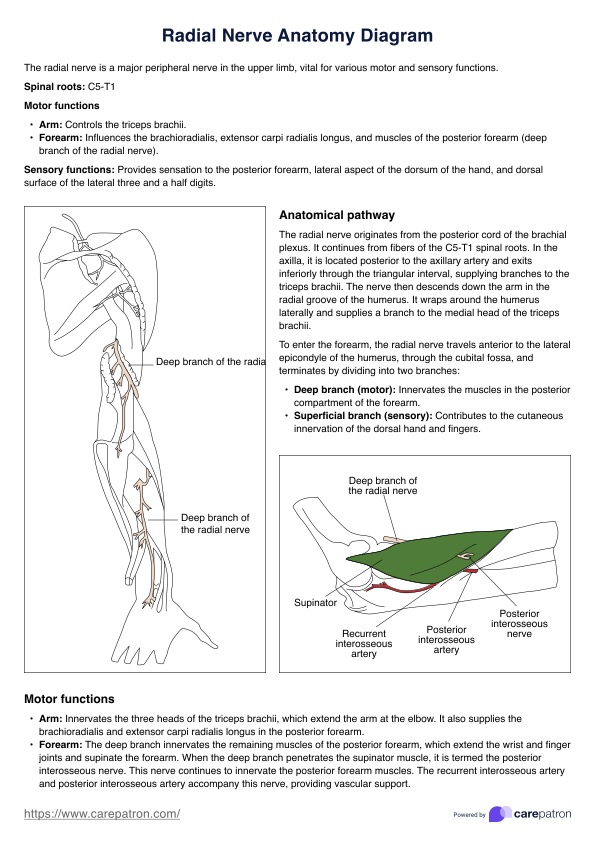
Comprehensive assessment
The template provides a structured framework to assess the patient's overall condition, including current blood glucose levels and factors contributing to high blood sugar. This comprehensive evaluation aids in identifying potential risks such as diabetic ketoacidosis.
Individualized care
With a focus on patient-specific needs, the template allows for the development of tailored interventions. This includes recommendations for a balanced diet, lifestyle modifications, and strategies to monitor blood pressure, ensuring holistic management of diabetes.
Effective management of complications
The template facilitates the identification and management of complications related to diabetes, including those arising from absolute insulin deficiency or relative insulin deficiency. This proactive approach helps prevent the progression of conditions like latent autoimmune diabetes.
Improved education and support
By using the template, healthcare providers can better educate patients about maintaining their blood glucose levels within the normal range, emphasizing the importance of monitoring, dietary adherence, and regular check-ups.
Enhanced patient outcomes
Overall, using our template improves patient outcomes by providing clear guidelines for intervention, helping manage high blood sugar, and reducing the risk of complications, ultimately promoting better health and quality of life.
Commonly asked questions
Self-monitoring of blood glucose levels is crucial for managing diabetes effectively. It helps individuals track their glucose levels, identify patterns, and make informed decisions about their treatment regimen to achieve optimal glycemic control.
Your dietary intake plays a significant role in determining your fasting blood glucose level. A balanced diet, rich in nutrients and low in refined sugars, can help maintain stable glucose levels and prevent spikes that could lead to complications.
Diabetes educators provide essential guidance and support for individuals managing diabetes. They offer education on proper dietary intake, self-monitoring techniques, and strategies for achieving better glycemic control, which can help prevent complications like peripheral neuropathy and heart failure.
Insulin-producing beta cells in the pancreas are vital for regulating blood sugar. In diabetes, these cells may be impaired or destroyed, affecting glucose levels. Understanding their function is essential for creating effective diabetes care plans and interventions.