What is dermatomyositis?
Dermatomyositis is a rare autoimmune disorder characterized by muscle weakness and inflammation, often accompanied by skin rash. It falls under the umbrella of idiopathic inflammatory myopathies, a group of muscle diseases of unknown origin. This condition primarily affects the skeletal muscles, causing progressive muscle weakness and fatigue.
One of the distinguishing features of dermatomyositis is its unique skin manifestations, which include a distinctive rash on the face, eyelids, knuckles, elbows, knees, and other areas exposed to the sun.
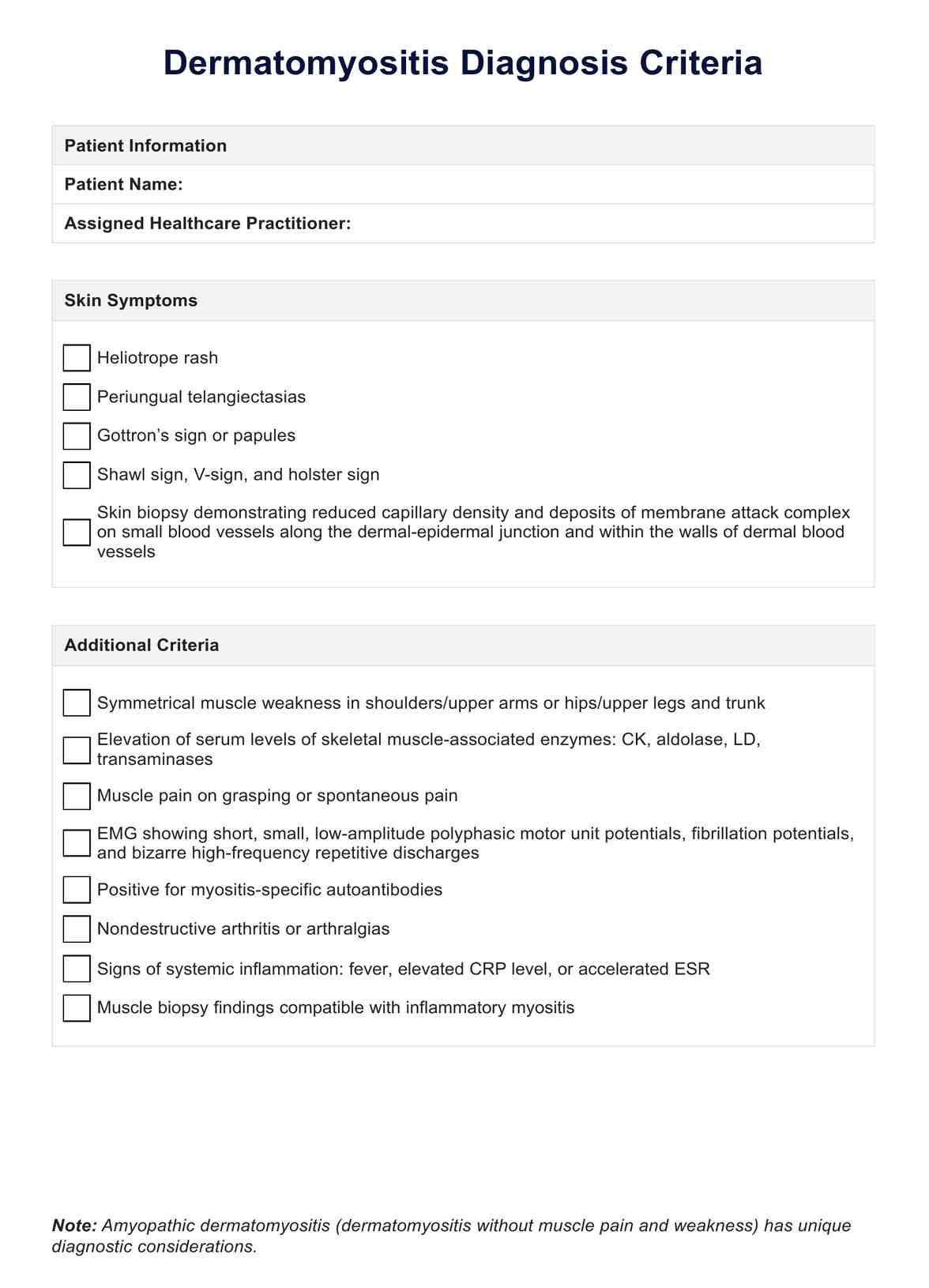
Muscle involvement in dermatomyositis can range from mild weakness to severe debilitation, impacting daily activities and quality of life. Diagnosis typically involves a combination of clinical evaluation, laboratory tests, imaging studies, and sometimes a muscle biopsy to confirm inflammation. Elevated levels of muscle enzymes such as creatine kinase (CK) and aldolase in the blood are often observed in dermatomyositis, indicating muscle damage.
In addition to muscle symptoms, dermatomyositis may also affect other organs, including the lungs. Interstitial lung disease is a common complication, leading to breathing difficulties and decreased lung function. Early detection and management of these complications are essential for optimal outcomes.
Physical therapy plays a crucial role in maintaining muscle strength and function, improving mobility, and enhancing overall quality of life for individuals with dermatomyositis. It helps to preserve muscle mass, prevent contractures, and alleviate pain.
Dermatomyositis symptoms
Dermatomyositis symptoms can vary widely among individuals and may involve multiple body systems. Recognizing these symptoms is crucial for early diagnosis and effective management of the condition.
Here, we outline the key symptoms associated with dermatomyositis.
- Muscle weakness: Progressive muscle weakness, especially in the proximal muscles (muscles closest to the trunk), making it difficult to perform everyday tasks such as climbing stairs, getting up from a seated position, or lifting objects.
- Skin rash: Characteristic rashes may be red or purple, often accompanied by swelling and itching.
- Muscle pain: Pain and tenderness in muscles, particularly during movement or pressure on the affected muscles.
- Difficulty swallowing: Dysphagia or difficulty swallowing due to muscle weakness in the throat and esophagus.
- Fatigue: Persistent fatigue and weakness, which may not improve with rest.
- Joint pain: Joint pain and stiffness resembling symptoms of arthritis.
- Shortness of breath: Interstitial lung disease, leading to shortness of breath, cough, and decreased exercise tolerance.
- Fever: Low-grade fever, especially during periods of disease activity.
- Weight loss: Unintentional weight loss, often associated with decreased appetite and muscle wasting.
- Gottron's papules: Raised, scaly, reddish-purple patches over the knuckles, elbows, or knees, known as Gottron's papules.
- Heliotrope rash: Bluish-purple discoloration or swelling of the eyelids, known as a heliotrope rash.
- Mechanic's hands: Thickened, cracked, and fissured skin on the palms and fingers, resembling the hands of a mechanic.
Risk factors and causes of dermatomyositis
Understanding the risk factors and causes of dermatomyositis is essential for identifying individuals who may be at higher risk and for developing strategies for prevention and early intervention.
Below are some factors that may contribute to the development of dermatomyositis:
- Autoimmune factors: Dermatomyositis is believed to result from an abnormal immune response, where the body's immune system mistakenly attacks its own muscle and skin tissues.
- Genetic predisposition: While dermatomyositis can occur in individuals without a family history, there may be genetic factors that predispose certain individuals to develop the condition.
- Environmental triggers: Exposure to certain environmental factors, such as ultraviolet (UV) radiation from sunlight, infections, or medications, may trigger or exacerbate dermatomyositis in susceptible individuals.
- Age and gender: Although dermatomyositis can occur at any age, it most commonly affects adults between the ages of 40 and 60, as well as children between the ages of 5 and 15. Additionally, women are more commonly affected than men.
- Underlying conditions: Dermatomyositis may be associated with other autoimmune diseases, such as systemic lupus erythematosus, or with certain types of cancer, including ovarian cancer. Individuals with these conditions may have an increased risk of developing dermatomyositis.
- Muscle enzyme abnormalities: Elevated levels of muscle enzymes, such as creatine kinase (CK) and aldolase, in the blood may indicate muscle damage and inflammation, which are characteristic features of dermatomyositis.
- Symmetrical muscle weakness: The presence of this muscle weakness, particularly affecting the proximal muscles (muscles closest to the trunk), is a hallmark feature of dermatomyositis.
Complications it can lead to
While dermatomyositis primarily affects the muscles and skin, it can lead to various complications that affect multiple body systems. Understanding these potential complications is crucial for comprehensive management and improving outcomes for individuals with dermatomyositis.
Here are some of the complications associated with this condition:
- Interstitial lung disease (ILD): Dermatomyositis can lead to ILD, a group of lung disorders characterized by inflammation and scarring of the lung tissue. ILD can cause breathing difficulties, coughing, and decreased lung function, impacting respiratory health.
- Respiratory muscle weakness: In severe cases, progressive weakness of the respiratory muscles, including the diaphragm and intercostal muscles, can lead to respiratory failure and the need for mechanical ventilation.
- Aspiration pneumonia: Dysphagia (difficulty swallowing) due to muscle weakness can increase the risk of aspiration pneumonia, where food, liquids, or saliva are inhaled into the lungs, leading to lung infections.
- Dysphonia: The weakness of speech production muscles can cause dysphonia (hoarseness) or difficulty speaking clearly.
- Dysphagia and malnutrition: Severe dysphagia may lead to inadequate food intake, malnutrition, and weight loss, affecting overall health and well-being.
- Contractures: Prolonged muscle weakness and immobility can result in contractures, where the muscles and tendons become permanently shortened, leading to joint stiffness and limited range of motion.
- Ulcers and skin infections: Chronic skin involvement in dermatomyositis, characterized by skin manifestations such as ulcers, rashes, and sores, can increase the risk of skin infections and delay wound healing.
- Calcinosis: In some cases, calcium deposits may form in the skin and soft tissues (calcinosis), leading to pain, inflammation, and impaired mobility.
- Malignancy: Dermatomyositis has been associated with an increased risk of certain cancers, particularly ovarian and lung cancer. Regular screening for cancer may be recommended in individuals with dermatomyositis.