Dementia Treatment Guidelines
Explore comprehensive dementia treatment guidelines and use Carepatron's free PDF download of an example plan. Learn about effective strategies and interventions for dementia care.


What is dementia?
Dementia is a term used to describe a group of conditions characterized by cognitive decline severe enough to interfere with daily life. It is not a specific disease but rather an umbrella term encompassing a range of symptoms that affect memory, thinking, and social abilities to varying degrees. One of the most common types of dementia is Alzheimer's disease, accounting for approximately 60-80% of cases.
At its core, dementia involves a decline in cognitive function beyond what might be expected from normal aging. This decline can manifest in various ways, including memory loss, difficulty with language and communication, impaired judgment, and changes in mood or behavior. These behavioral and psychological symptoms can have a profound impact on both individuals with dementia and their caregivers.
Importantly, dementia is not just about memory loss. It also encompasses a range of cognitive and behavioral symptoms that can significantly impact an individual's quality of life. In some cases, dementia may begin with mild cognitive impairment, where memory and thinking skills are impaired but not severe enough to interfere with daily functioning. However, as the condition progresses, cognitive decline becomes more pronounced, eventually leading to significant impairment in multiple areas of functioning.
Understanding dementia is crucial for healthcare professionals in clinical practice, caregivers, and family members. Additionally, raising awareness about dementia helps reduce stigma and promotes a more supportive environment for individuals living with the condition.
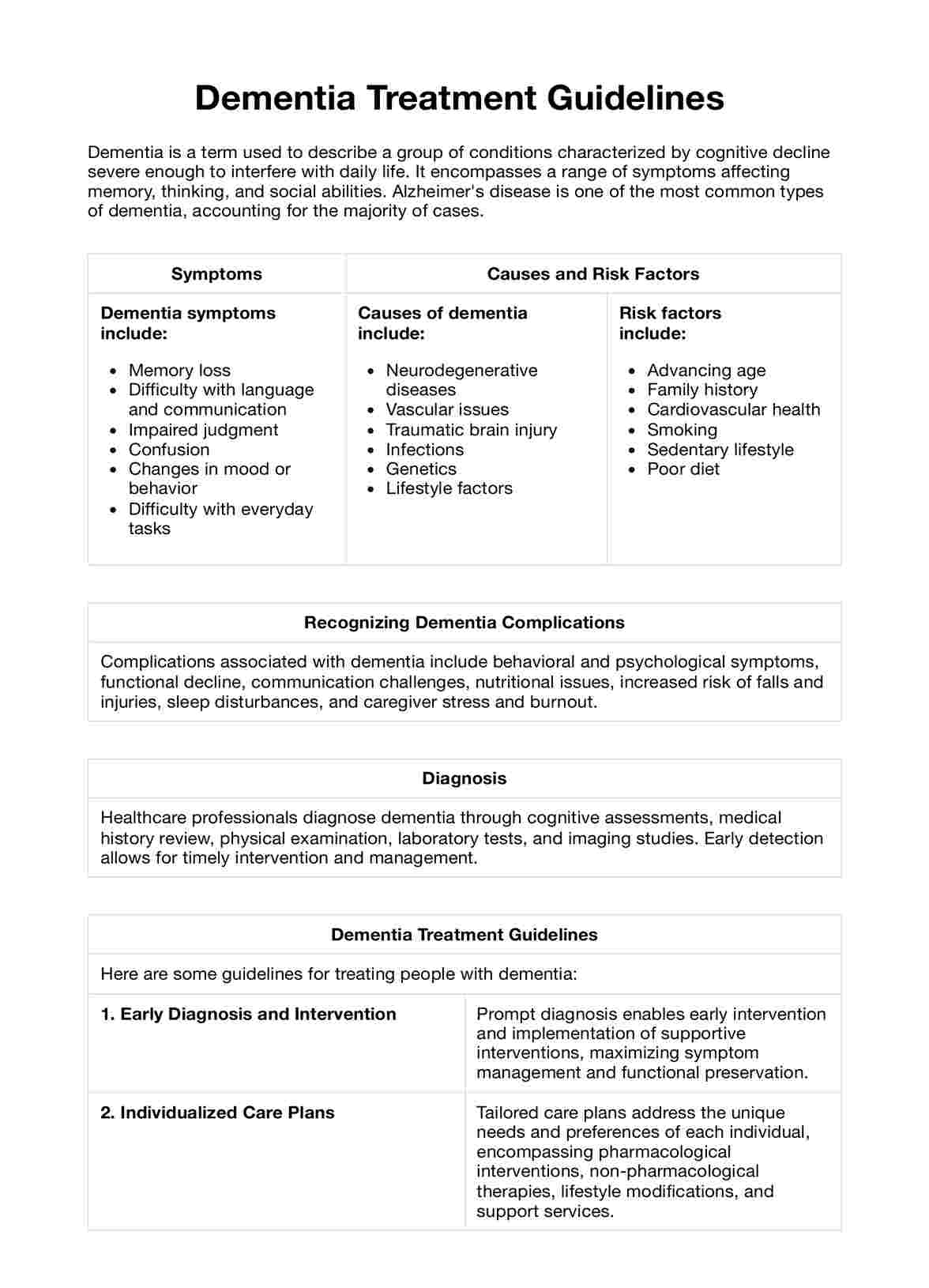
Dementia symptoms
Dementia symptoms vary depending on the underlying cause and the stage of the condition. It's important to recognize these symptoms early to facilitate timely intervention and support. Below are some common signs and symptoms associated with dementia:
- Memory loss: Forgetfulness, particularly of recent events or important dates.
- Difficulty with language and communication: Trouble finding the right words, following conversations, or understanding speech.
- Impaired judgment: Poor decision-making, inability to assess risks or understand consequences.
- Confusion and disorientation: Getting lost in familiar places, losing track of time, or difficulty recognizing people.
- Difficulty with everyday tasks: Struggling to complete routine tasks such as cooking, cleaning, or managing finances.
- Changes in mood or behavior: Mood swings, agitation, irritability, apathy, or withdrawal from social activities.
- Loss of interest: Decreased interest in hobbies or activities once enjoyed.
- Personality changes: Shifts in personality traits, such as becoming suspicious, paranoid, or impulsive.
- Difficulty with complex tasks: Challenges with planning, organizing, or problem-solving.
- Inability to recognize familiar objects or faces: Difficulty recognizing familiar objects or people, even close family members.
Dementia causes and risk factors
Dementia can arise from various factors, including neurodegenerative diseases, vascular issues, and lifestyle factors. Identifying these causes and risk factors can help implement preventive measures and targeted interventions to reduce the risk of dementia.
Causes:
- Neurodegenerative diseases: Conditions such as Alzheimer's disease, Parkinson's disease, and Lewy body dementia involve progressive damage to brain cells, leading to cognitive decline.
- Vascular issues: Conditions affecting blood flow to the brain, such as strokes, small vessel disease, or transient ischemic attacks (TIAs), can contribute to vascular dementia.
- Traumatic brain injury: Head injuries resulting from accidents, falls, or sports-related injuries can increase the risk of developing dementia, especially if repeated or severe.
- Infections: Certain infections, such as HIV/AIDS or chronic infections causing inflammation in the brain, may increase the risk of dementia.
- Genetics: Family history and genetic factors can play a role in certain types of dementia, such as early-onset Alzheimer's disease or frontotemporal dementia.
- Lifestyle factors: Unhealthy lifestyle choices, including poor diet, lack of exercise, smoking, excessive alcohol consumption, and untreated hypertension or diabetes, can increase the risk of developing dementia.
Risk factors:
- Age: Advancing age is the most significant risk factor for dementia, with the risk increasing significantly after the age of 65.
- Family history: Having a family member with dementia increases the risk of developing the condition.
- Cardiovascular health: Conditions such as high blood pressure, high cholesterol, obesity, and diabetes can increase the risk of vascular dementia.
- Smoking: Tobacco use is associated with an increased risk of dementia due to its detrimental effects on cardiovascular health and brain function.
- Sedentary lifestyle: Lack of physical activity is linked to a higher risk of cognitive relapse and dementia.
- Poor diet: Diets high in saturated fats, sugars, and processed foods and low in fruits, vegetables, and omega-3 fatty acids may increase the risk of dementia.
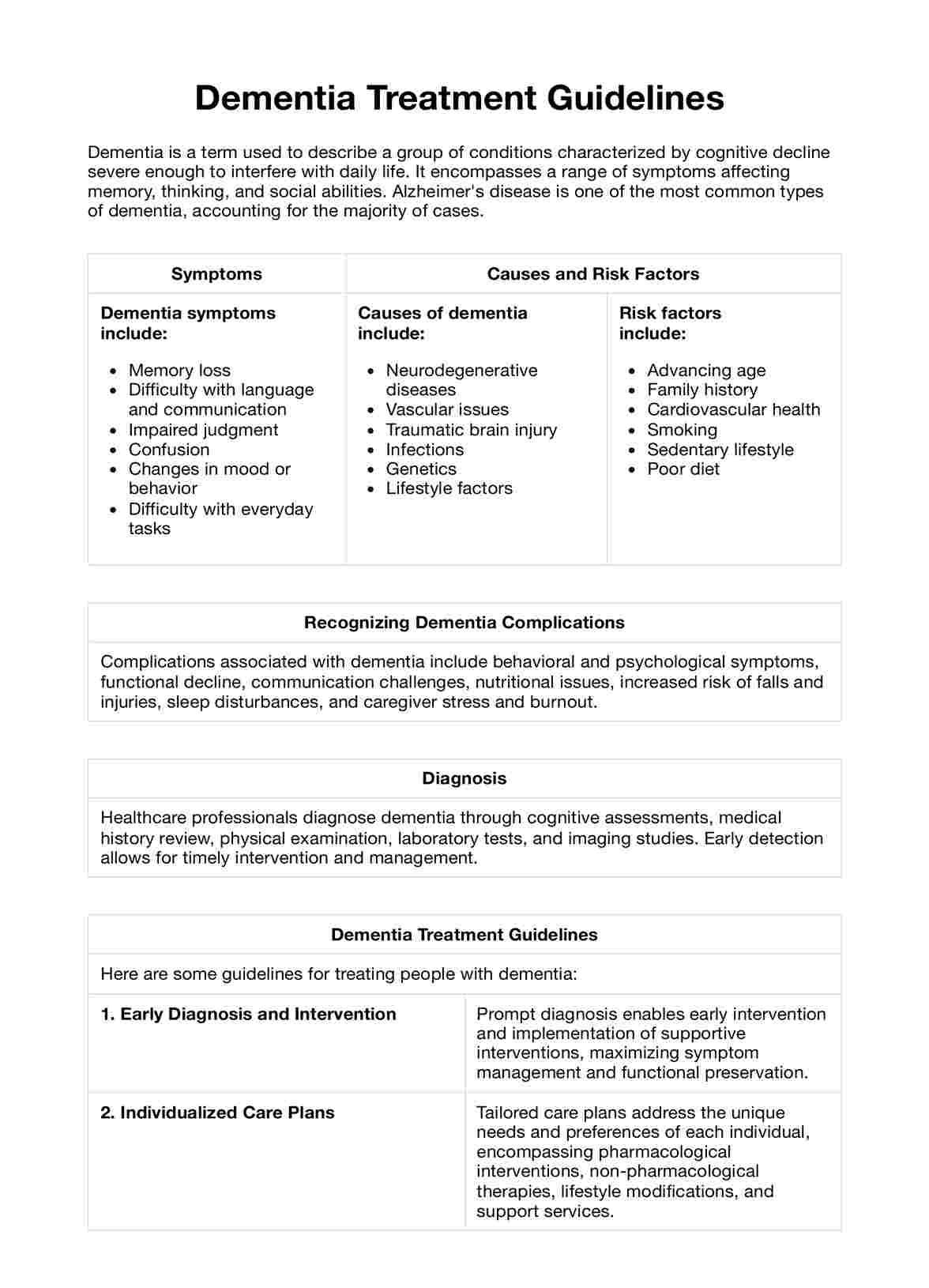
Examples of dementia complications
Living with dementia can lead to various complications that affect both the individual with the condition and their caregivers. Understanding these potential complications is crucial for providing comprehensive care and support.
Here are some common examples of complications associated with dementia:
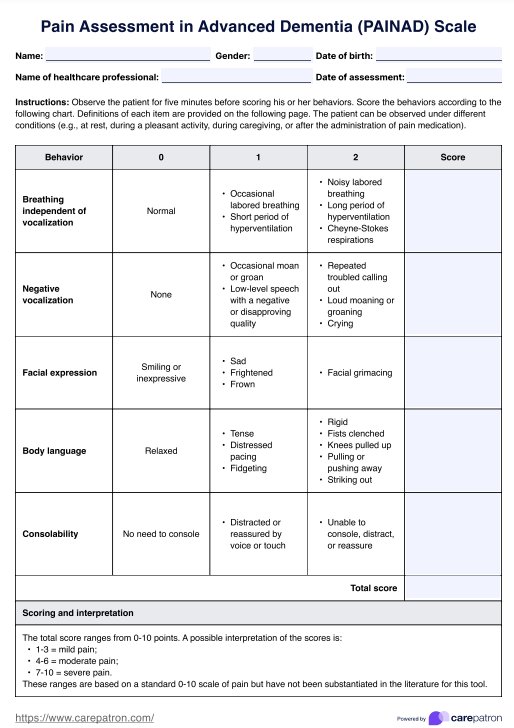
- Behavioral and psychological symptoms: Individuals with dementia may experience behavioral and psychological symptoms such as agitation, aggression, wandering, hallucinations, and delusions. These symptoms can be distressing for both the individual and their caregivers and may require specialized interventions for management.
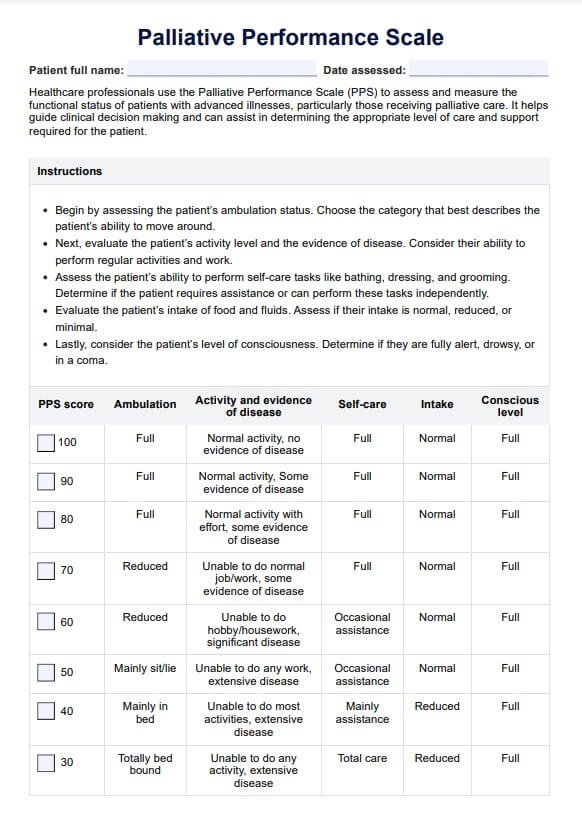
- Functional decline: As dementia progresses, individuals may experience a decline in their ability to perform activities of daily living independently. This decline can include difficulties with self-care tasks, mobility, and maintaining a safe environment, leading to increased dependency on caregivers.
- Communication challenges: Dementia can affect language abilities, making it challenging for individuals to express themselves effectively or understand others. Communication difficulties can lead to frustration, social isolation, and misunderstandings, impacting relationships and quality of life.
- Nutritional issues: Individuals with dementia may experience changes in appetite, taste perception, or swallowing difficulties, putting them at risk of malnutrition or dehydration. Poor nutrition can exacerbate cognitive downturn, weaken immune function, and increase the risk of other health complications.
- Increased risk of falls and injuries: Cognitive impairment, impaired balance, and gait disturbances associated with dementia can increase the risk of falls and injuries. Falls can result in fractures, head injuries, and other serious consequences, requiring appropriate preventive measures and safety interventions.
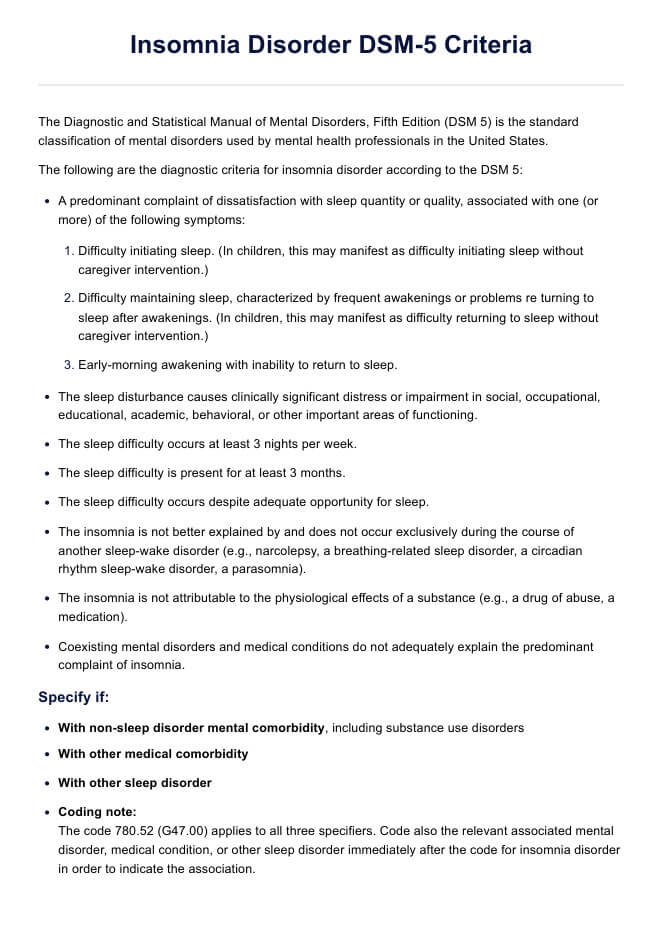
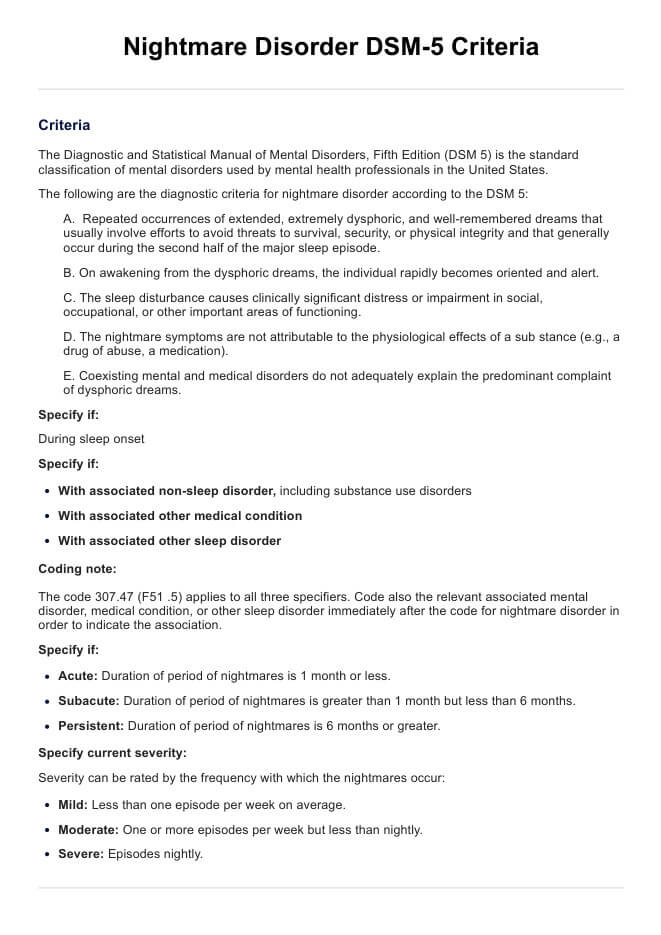
- Sleep disturbances: Sleep disturbances are common among individuals with dementia, including insomnia, nighttime wandering, and daytime sleepiness. Poor sleep quality can exacerbate cognitive impairment, mood disturbances, and behavior symptoms, affecting overall well-being and functioning.
- Caregiver stress and burnout: Providing care for a loved one with dementia can be physically, emotionally, and financially demanding. Caregivers may experience high levels of stress, depression, anxiety, and burnout, impacting their own health and well-being.
Dementia Treatment Guidelines Template
Dementia Treatment Guidelines Example
How do healthcare professionals diagnose dementia?
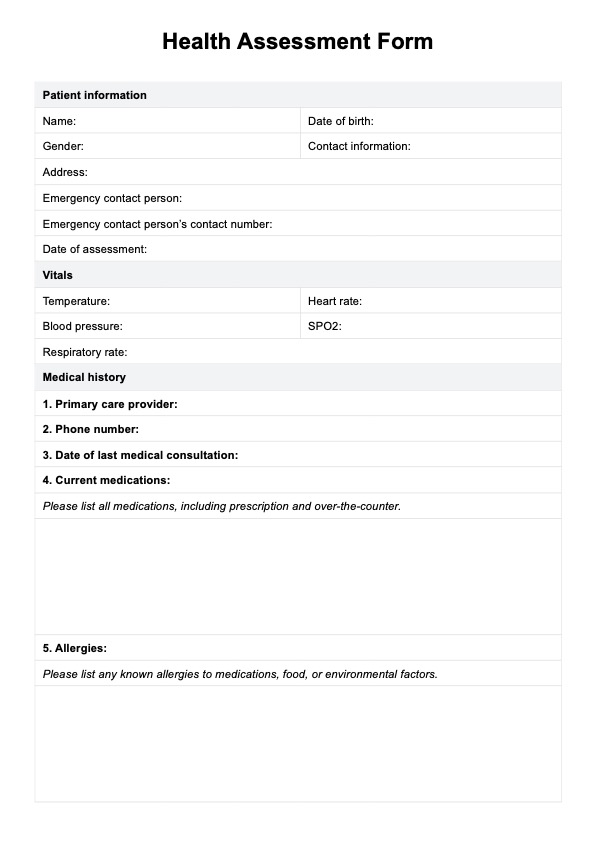
Diagnosing dementia involves a comprehensive evaluation of a person's cognitive and functional abilities, as well as consideration of medical history, laboratory tests, and imaging studies. Healthcare professionals, including primary care physicians, neurologists, geriatricians, and psychiatrists, play a crucial role in the diagnostic process. Below are the steps involved in diagnosing dementia:
Assessment of cognitive status
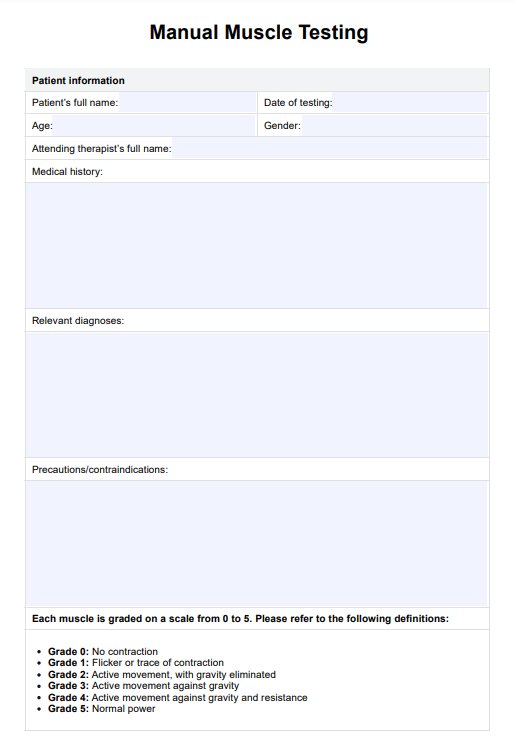
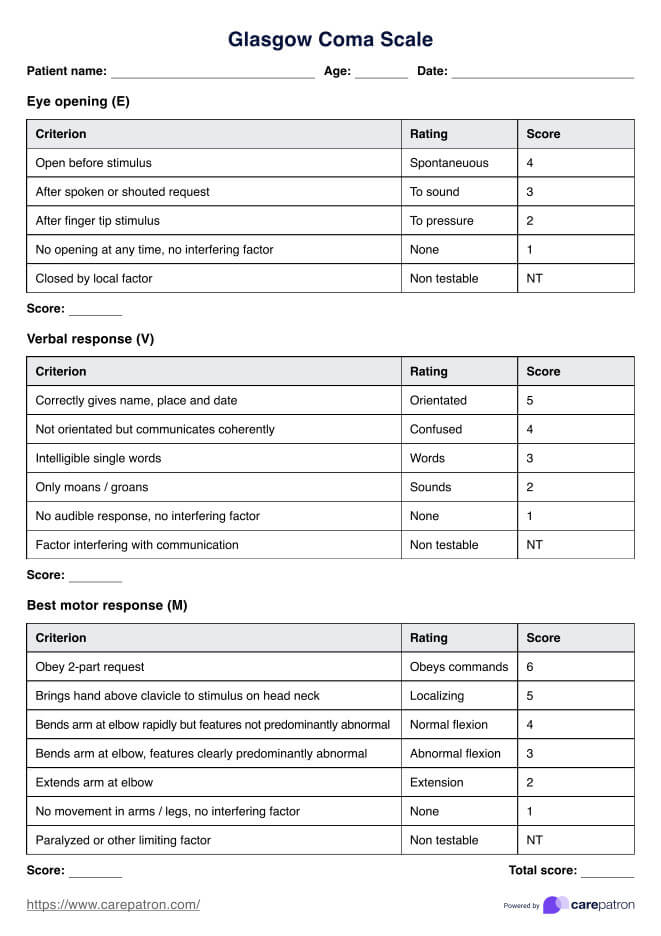
Healthcare professionals typically begin the diagnostic process by assessing the individual's cognitive status through various screening tools and assessments. These may include standardized tests such as the Mini-Mental State Examination (MMSE) or the Montreal Cognitive Assessment (MoCA), which evaluate memory, attention, language, and visuospatial abilities. Additionally, healthcare providers may conduct interviews with the individual and their family members to gather information about changes in cognitive function over time.
Evaluation of medical history and symptoms
A thorough review of the individual's medical history, including any past medical conditions, medications, and family history of dementia, is essential for identifying potential risk factors and underlying causes of cognitive relapse. Healthcare professionals also assess the individual's symptoms, including memory loss, language difficulties, changes in mood or behavior, and functional impairments in daily activities. This information helps guide further diagnostic testing and management.
Physical examination and laboratory tests
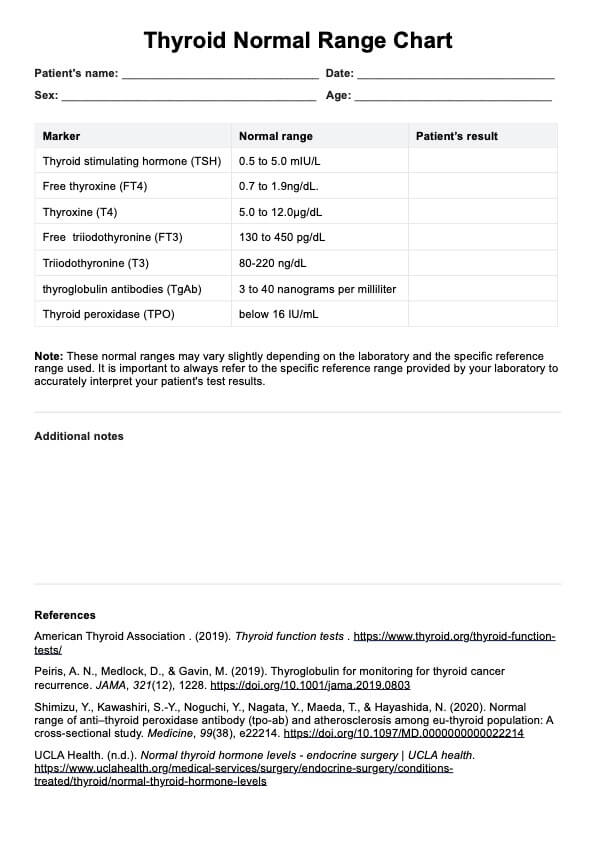
A comprehensive physical examination assesses overall health and identifies any underlying medical conditions that may contribute to cognitive impairment. Laboratory tests, including blood tests to evaluate thyroid function, vitamin B12 levels, and metabolic parameters, are often performed to rule out reversible causes of cognitive relapse. Additionally, imaging studies such as magnetic resonance imaging (MRI) or computed tomography (CT) scans may be ordered to assess for structural changes in the brain and rule out other neurological conditions.
Diagnostic criteria and clinical guidelines
Healthcare professionals follow established diagnostic criteria and clinical guidelines, such as those provided by organizations like the National Institute for Health and Care Excellence (NICE) or the American Academy of Neurology (AAN), to guide the diagnosis of dementia. These criteria outline specific cognitive and functional impairments required for a diagnosis of dementia and differentiate between different types of dementia, including Alzheimer's disease, vascular dementia, and Lewy body dementia.
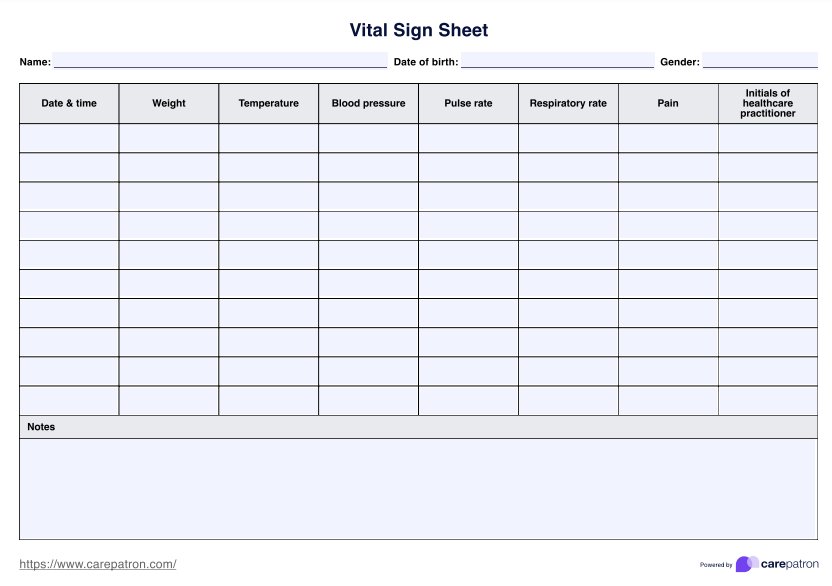
Monitoring and follow-up
Once a diagnosis of dementia is established, healthcare professionals work with the individual and their caregivers to develop a comprehensive care plan tailored to their needs. This may include medication management, cognitive rehabilitation, psychotherapy, and support services to address both mild cognitive impairment and behavioral symptoms. Regular monitoring of cognitive status, functional abilities, and overall health is essential for ongoing management and adjustment of treatment strategies.
Benefits of having dementia treatment guidelines
Dementia treatment guidelines serve as invaluable tools for healthcare professionals, caregivers, and individuals living with dementia, offering a structured framework for optimizing care and enhancing outcomes. The following are key benefits associated with the implementation of dementia treatment guidelines:
1. Standardized care practices
Dementia treatment guidelines provide standardized approaches to care delivery, ensuring consistency and quality across clinical practice settings. By adhering to established policies, healthcare professionals can streamline diagnostic procedures, treatment interventions, and care planning processes, ultimately improving the quality and efficiency of dementia care.
2. Early detection and intervention
Guidelines emphasize the importance of early detection and intervention in dementia management. By recognizing cognitive deficits and behavioral symptoms in the early stages, healthcare professionals can initiate timely interventions aimed at slowing disease progression, improving cognitive function, and enhancing overall quality of life for individuals living with dementia.
3. Evidence-based interventions
Dementia treatment guidelines are informed by current research evidence, including findings from clinical trials and meta-analyses. By incorporating evidence-based interventions into clinical practice, healthcare professionals can ensure that individuals with dementia receive the most effective and appropriate treatments, including pharmacological and non-pharmacological therapies.
4. Improved care coordination
Guidelines facilitate interdisciplinary collaboration among healthcare providers, caregivers, and support services, promoting seamless care coordination and continuity of care for individuals with dementia. By establishing clear roles, responsibilities, and communication channels, guidelines help ensure that all care team members are working together towards common treatment goals.
5. Enhanced quality of life
By optimizing symptom management, promoting functional independence, and addressing psychosocial needs, dementia treatment guidelines contribute to enhanced quality of life for individuals living with dementia and their caregivers. Through targeted interventions aimed to improve cognitive function, managing behavioral symptoms, and supporting mental health, guidelines help individuals with dementia live fulfilling and meaningful lives.
Common treatments for dementia
Dementia treatment encompasses a variety of approaches aimed at managing symptoms, improving cognitive function, and enhancing overall quality of life for individuals affected by the condition. Here are some common treatments utilized in dementia care:
Selective serotonin reuptake inhibitors
SSRIs are a class of antidepressant medications commonly used to manage mood and behavioral disturbances in patients with dementia. These medications work by increasing serotonin levels in the brain, which can help alleviate symptoms of depression, anxiety, and agitation commonly experienced by individuals with dementia.
Music therapy
Music therapy involves the use of music-based interventions to address cognitive, emotional, and social needs in individuals with dementia. Research has shown that music therapy can improve mood, reduce agitation, and enhance communication and social interaction in elderly patients with dementia. It can also stimulate memory recall and evoke positive emotions, providing a valuable therapeutic tool for individuals with cognitive impairment.
Behavioral therapy
Behavioral therapy focuses on modifying behaviors and addressing behavioral disturbances commonly observed in patients with dementia. This approach involves identifying triggers for problematic behaviors, implementing strategies to manage and reduce these behaviors, and providing support and guidance to caregivers. Behavioral therapy aims to improve the quality of life for both individuals with dementia and their caregivers by promoting adaptive coping strategies and enhancing communication and understanding.
Antipsychotic drugs
Antipsychotic medications may be prescribed to manage severe behavioral disturbances, such as agitation, aggression, and hallucinations, in patients with dementia. However, their use is often reserved for cases where non-pharmacological interventions have been ineffective due to the increased risk of adverse effects, including sedation, extrapyramidal symptoms, and cognitive decline, particularly in elderly patients with moderate to severe dementia.
Cholinesterase inhibitors
Cholinesterase inhibitors are a class of medications commonly used to treat Alzheimer's disease, the most common form of dementia. These medications work by increasing levels of acetylcholine, a neurotransmitter involved in memory and cognition, in the brain. Cholinesterase inhibitors can help improve cognitive function and reduce symptoms of memory loss and confusion in patients with mild to moderate Alzheimer's disease.
Occupational therapy
Occupational therapy focuses on helping individuals with dementia maintain independence and engagement in meaningful activities of daily living. Occupational therapists assess cognitive and functional abilities, identify barriers to independent living, and develop personalized strategies and interventions to optimize functional performance and promote well-being in patients with dementia.
Supportive care and education
Supportive care and education are essential components of dementia treatment, providing individuals with dementia and their caregivers with the knowledge, skills, and resources needed to navigate the challenges of living with the condition. Supportive care may include access to support groups, respite care services, and community resources. At the same time, education aims to enhance understanding of dementia, promote effective coping strategies, and improve communication and caregiving skills among caregivers and family members.
Commonly asked questions
The standard treatment for dementia involves a combination of pharmacological and non-pharmacological interventions aimed at managing symptoms and improving quality of life. This may include medications to address cognitive decline and behavioral symptoms and therapies such as cognitive stimulation and occupational therapy.
While there is no definitive cure for dementia, cholinesterase inhibitors (e.g., donepezil, rivastigmine) and N-methyl-D-aspartate (NMDA) receptor antagonists (e.g., memantine) are considered the gold standard of pharmacological treatment for Alzheimer's disease, the most common form of dementia. These medications may help improve cognitive function and alleviate symptoms in some individuals.
In the early stages of dementia, non-pharmacological interventions such as cognitive stimulation, physical exercise, and social engagement are often recommended as the first line of treatment. These interventions can help maintain cognitive function, promote independence, and enhance overall well-being.