Insomnia Disorder DSM-5 Criteria
Learn about Insomnia Disorder DSM-5 Criteria to help you diagnose and treat insomnia disorder.


What is insomnia disorder?
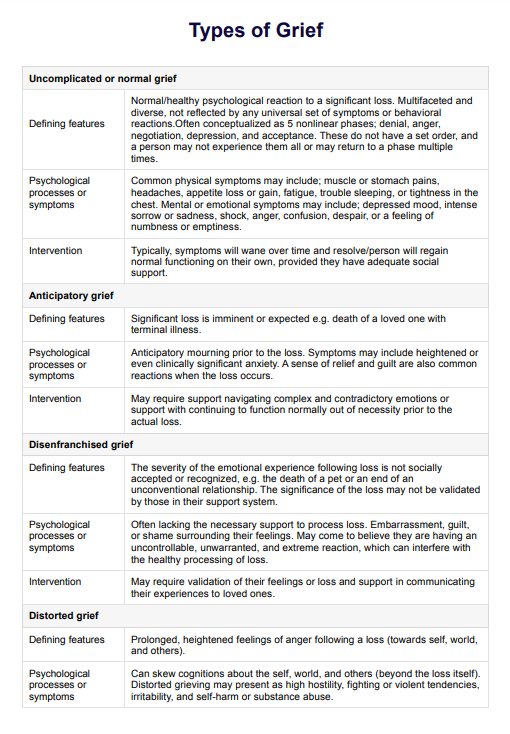
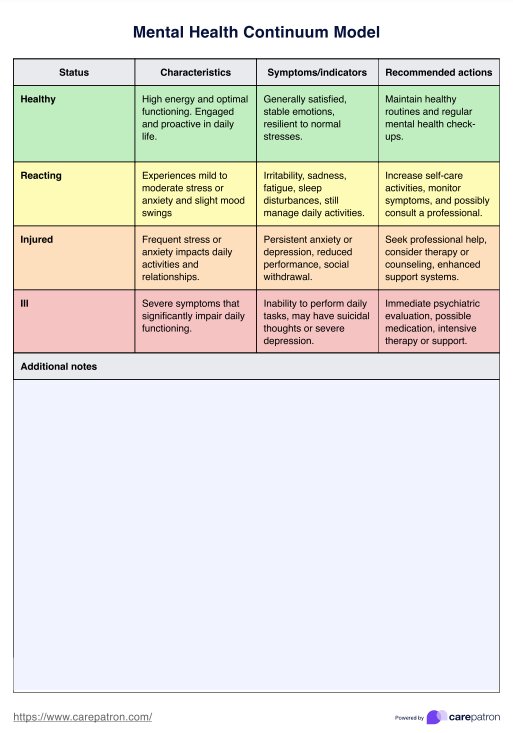
There are some instances when an individual cannot sleep at night. While it can be inevitable, it can be pretty concerning when it becomes frequent because poor sleep can significantly affect one's function, leading to fatigue, impaired performance, and excessive daytime sleepiness, among many others. Determining when sleep difficulty occurs is essential because a client might manifest insomnia symptoms.
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM 5) by the American Psychiatric Association classifies insomnia disorder under sleep-wake disorders along with hypersomnolence disorder, narcolepsy, breathing-related sleep disorder, circadian rhythm sleep disorder, non-rapid eye movement (NREM) sleep arousal disorders, nightmare disorder, rapid eye movement (REM) sleep behavior disorder, restless legs syndrome, and substance/medication-induced sleep disorder.
Insomnia disorder affects about a third of the general population in the United States, with more prevalence among females. The International Classification of Sleep Disorders, Third Edition (ICSD-3) by the American Academy of Sleep Medicine classifies insomnia into three: chronic insomnia disorder, short-term insomnia disorder, and other insomnia disorder (Kaur et al., 2023). Causes of insomnia include temperamental, environmental, genetic, and physiological factors, and understanding them is necessary to enhance sleep quality and identify sleep difficulties to help you provide your client with the best quality of care.
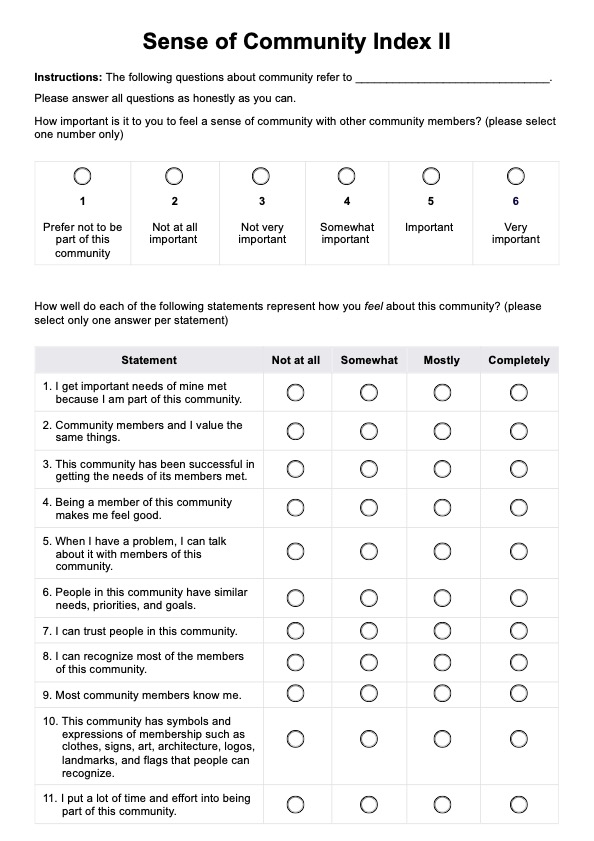
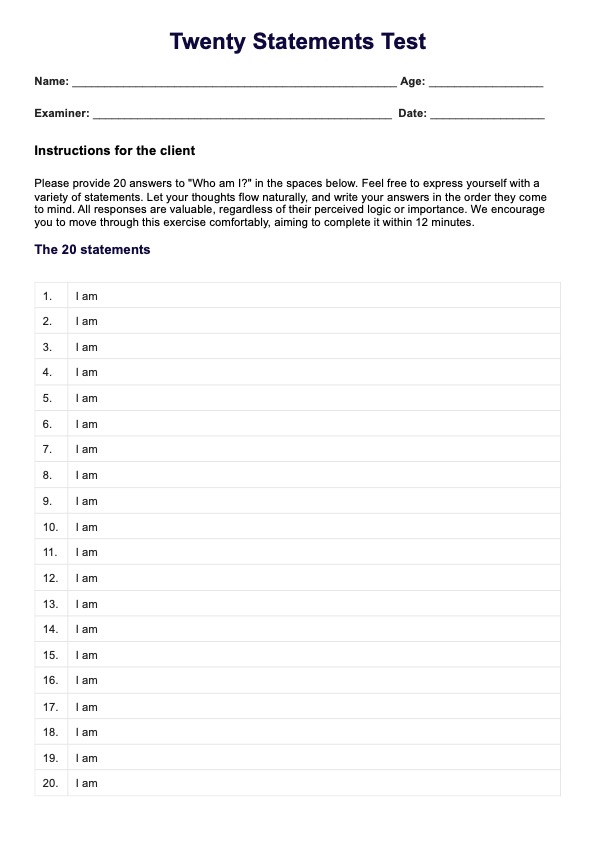
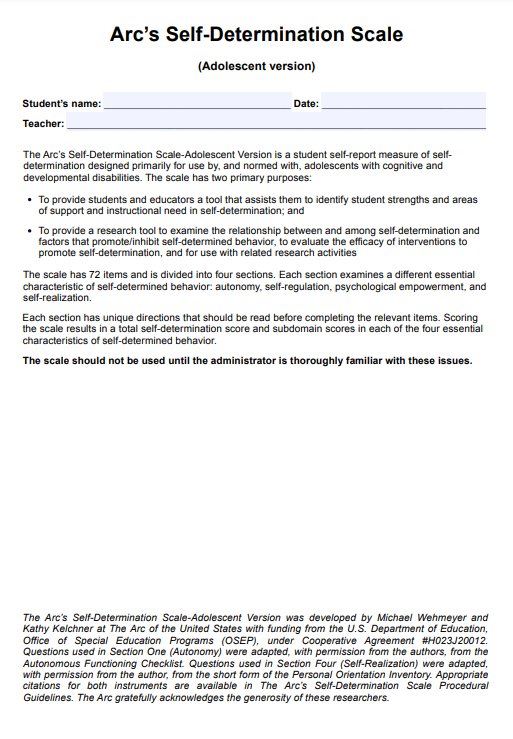
Insomnia Disorder DSM-5 Criteria Template
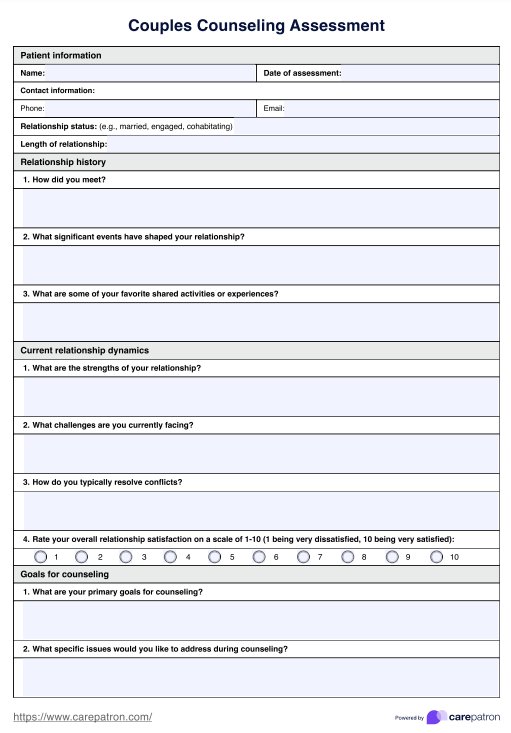
Insomnia Disorder DSM-5 Criteria Sample
How is insomnia disorder diagnosed?
Insomnia diagnosis is done through a series of evaluations to confirm its presence and differentiate it from other psychiatric disorders. Usually, the following are conducted:
Medical history and physical examination
The clinician will ask about the client's sleep patterns, lifestyle, and any medical conditions they have. They may also perform a physical exam to check for signs of other conditions causing insomnia.
Diagnostic tests
Tests like actigraphy, which measures sleep-wake patterns using a wrist-worn device, and blood tests to rule out other health issues can help diagnose insomnia. These tests provide detailed information about your sleep habits and overall health.
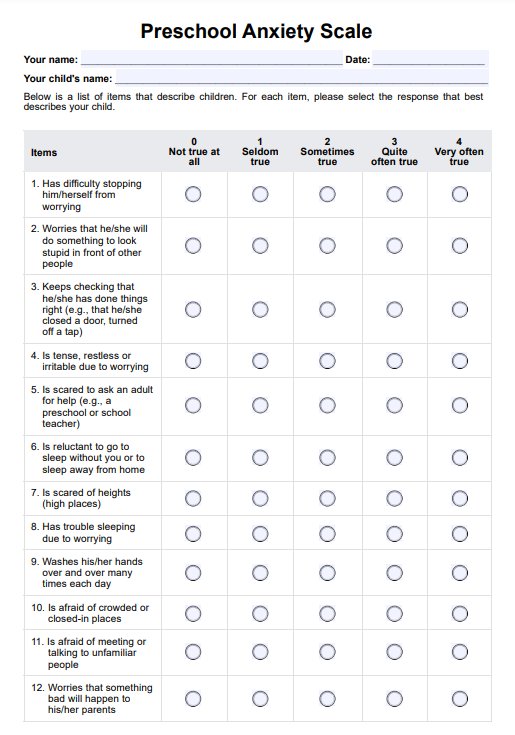
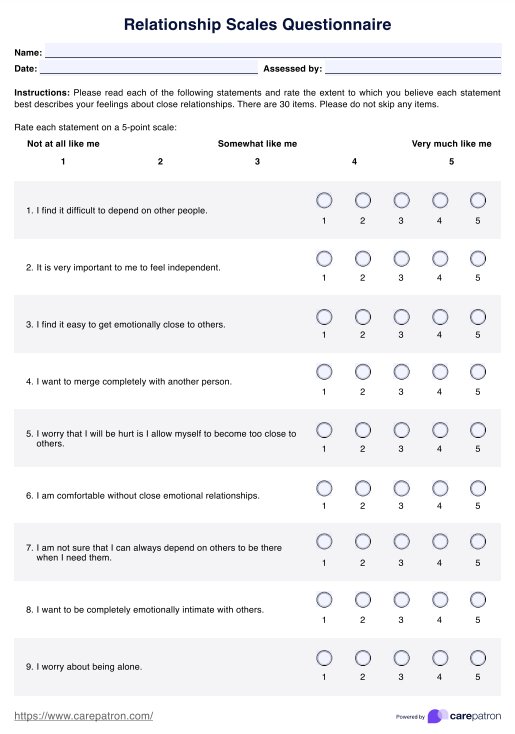
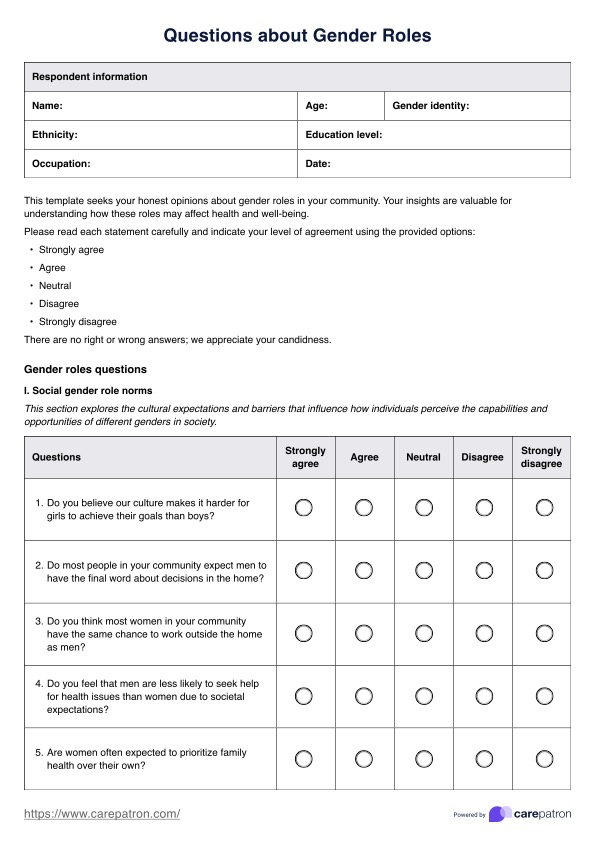
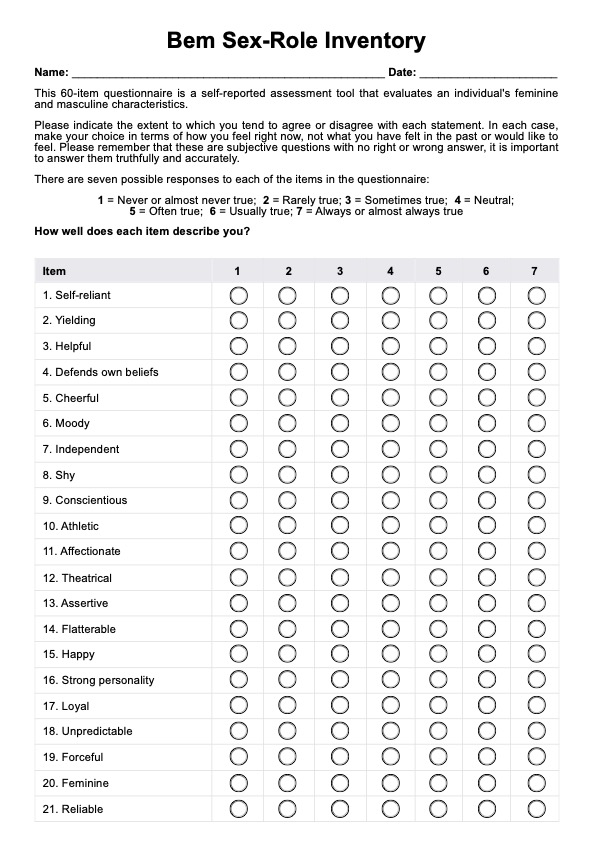
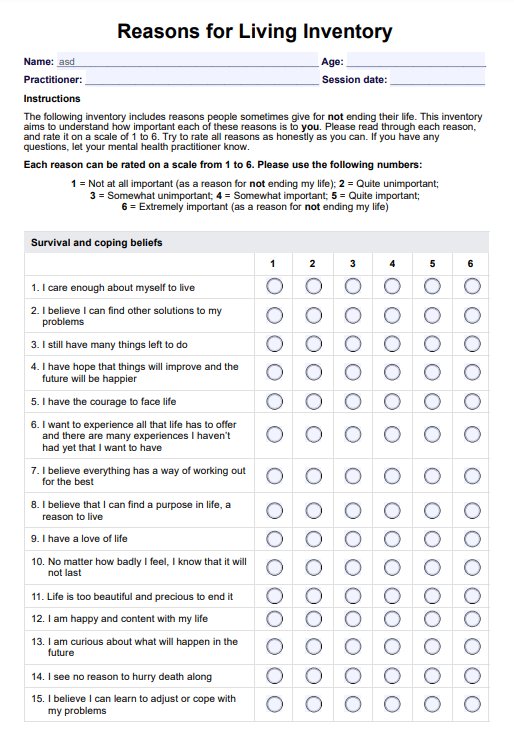
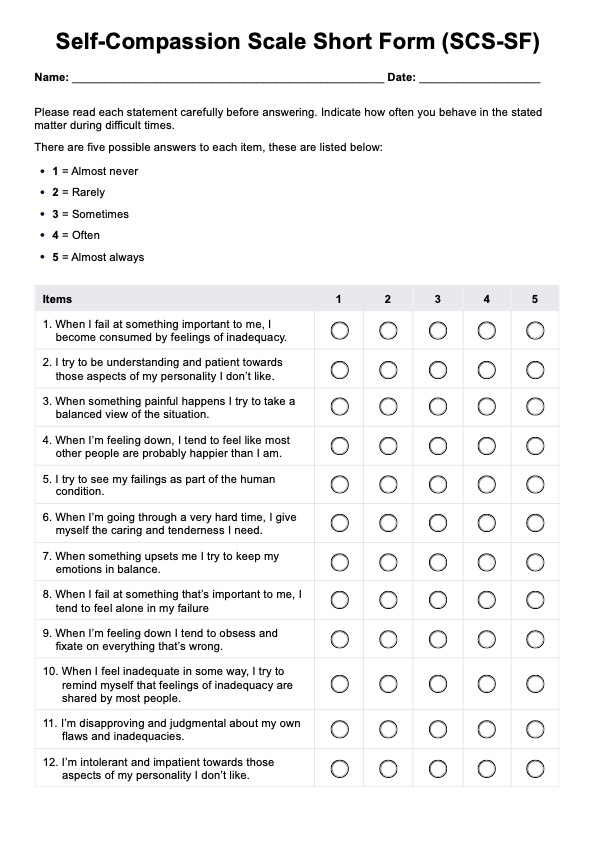
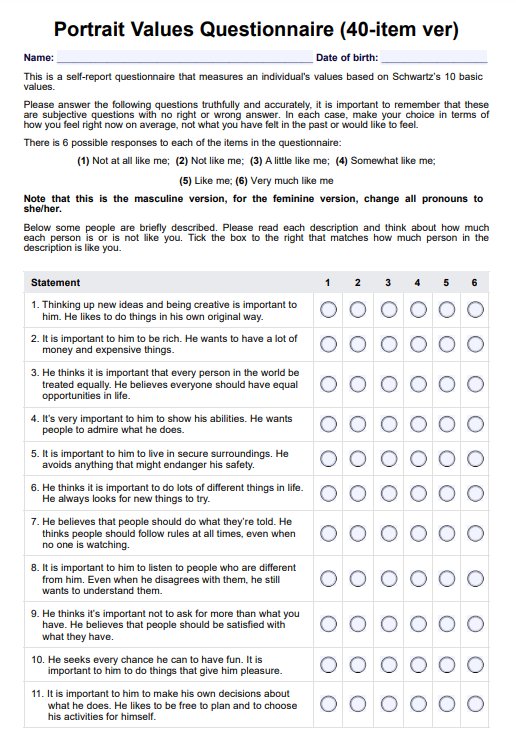
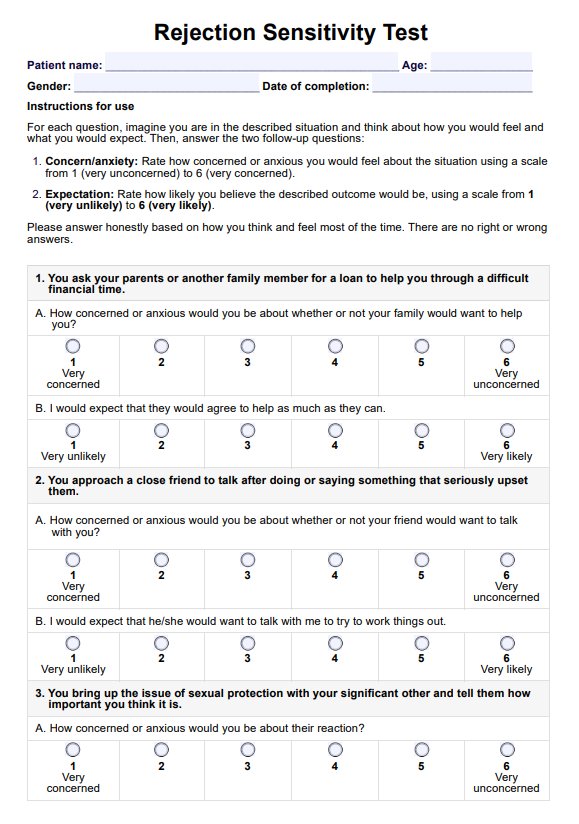
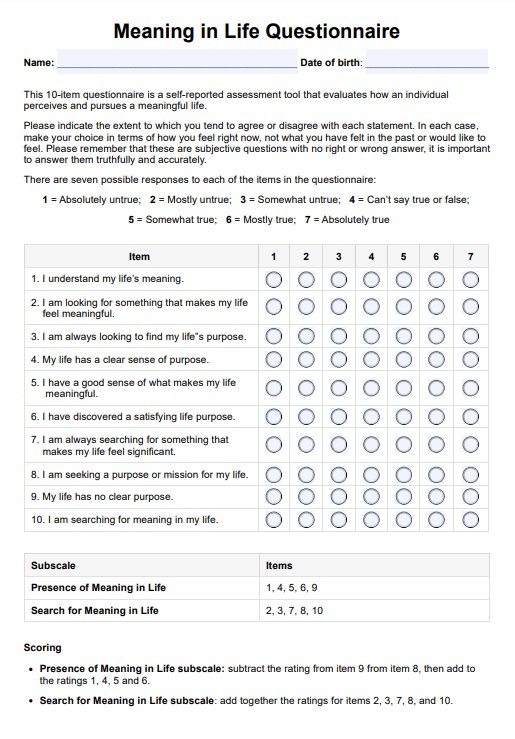
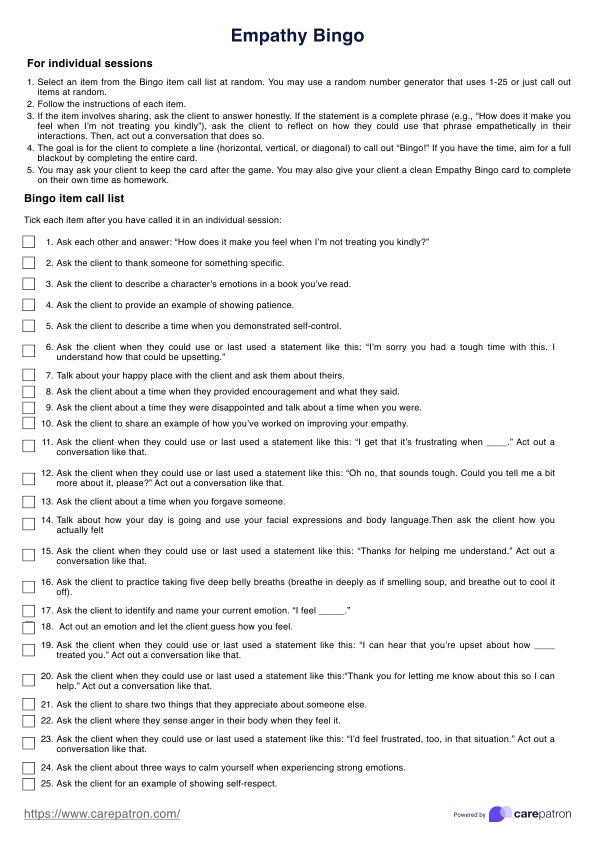
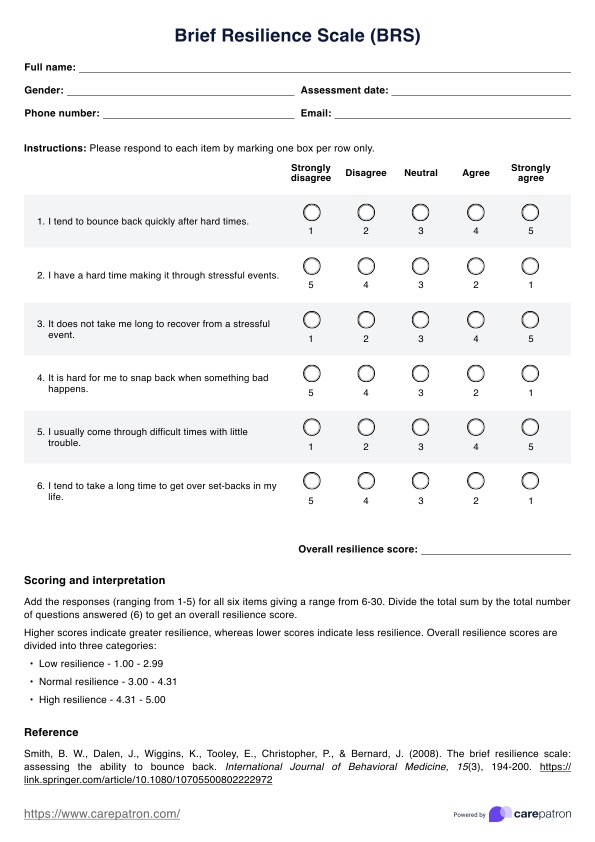
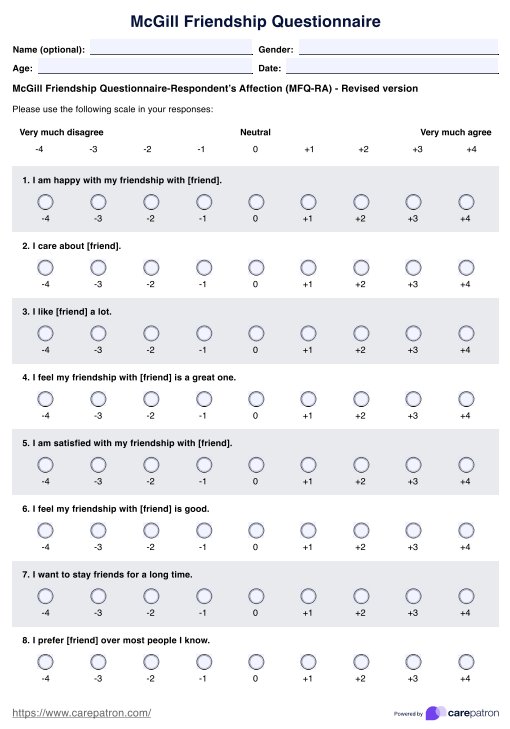
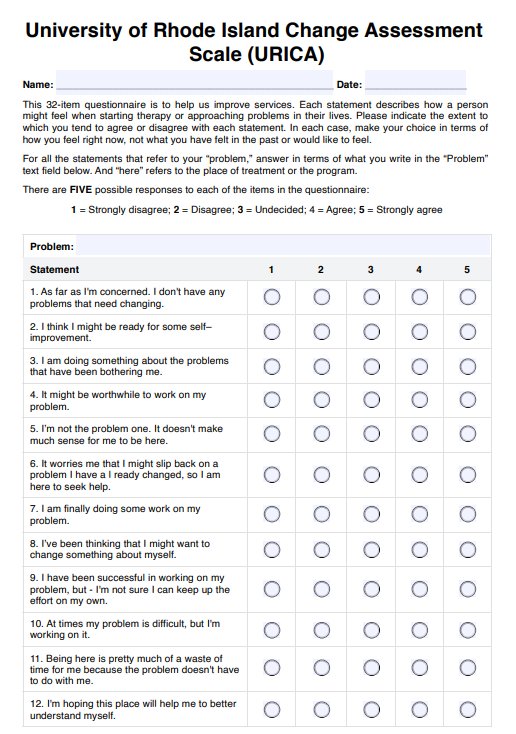
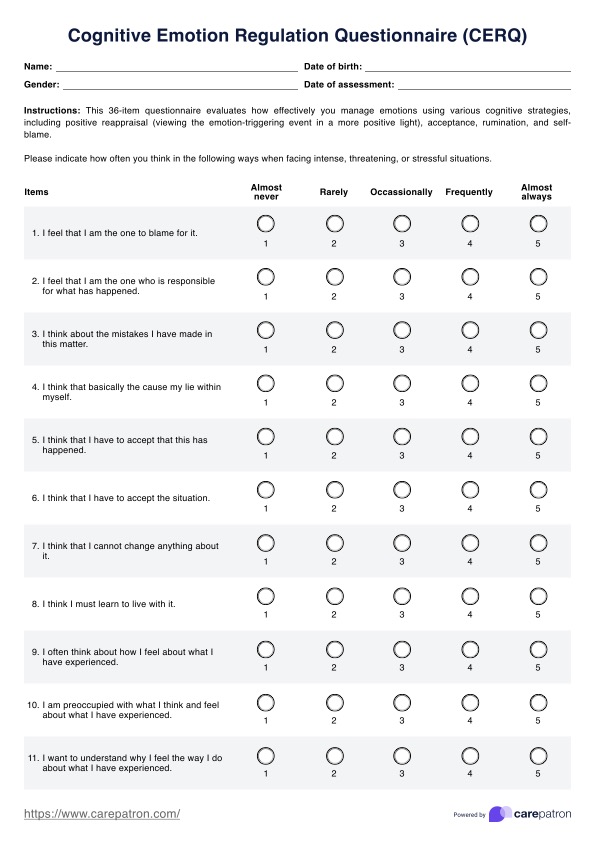
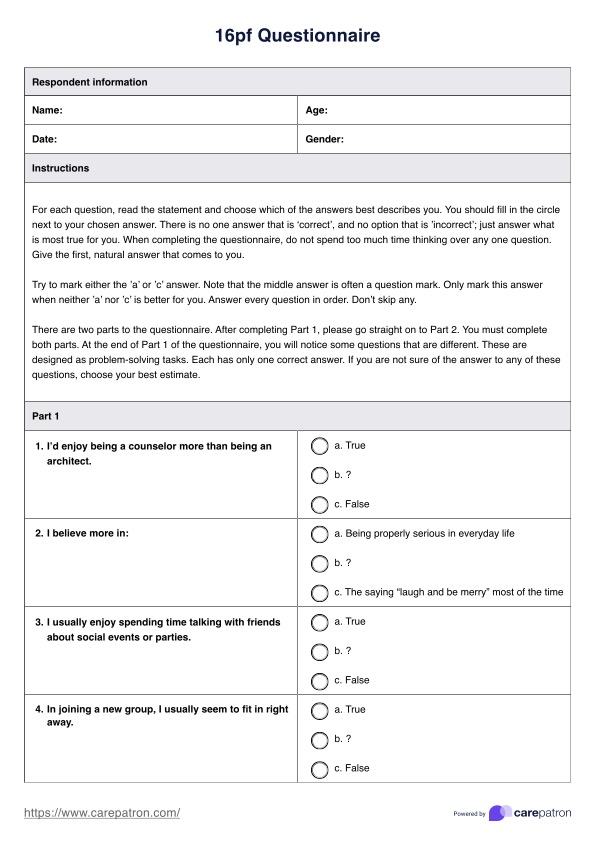
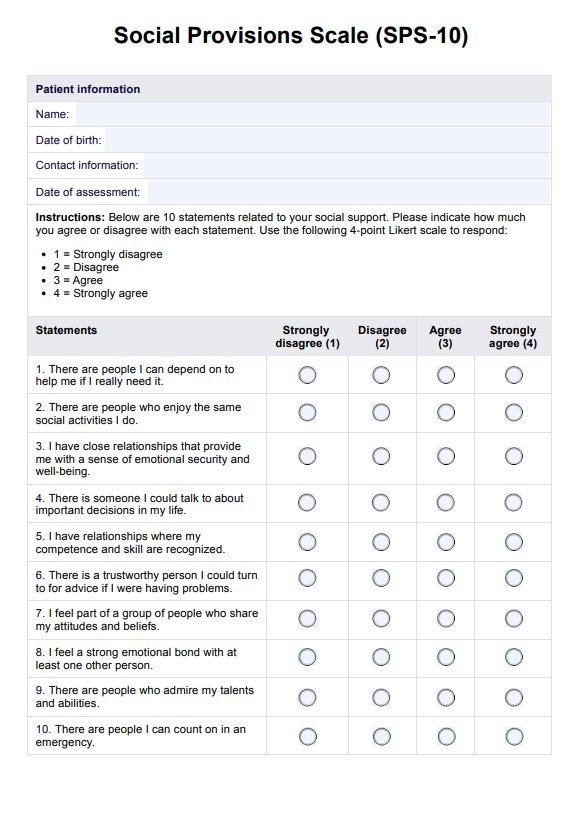
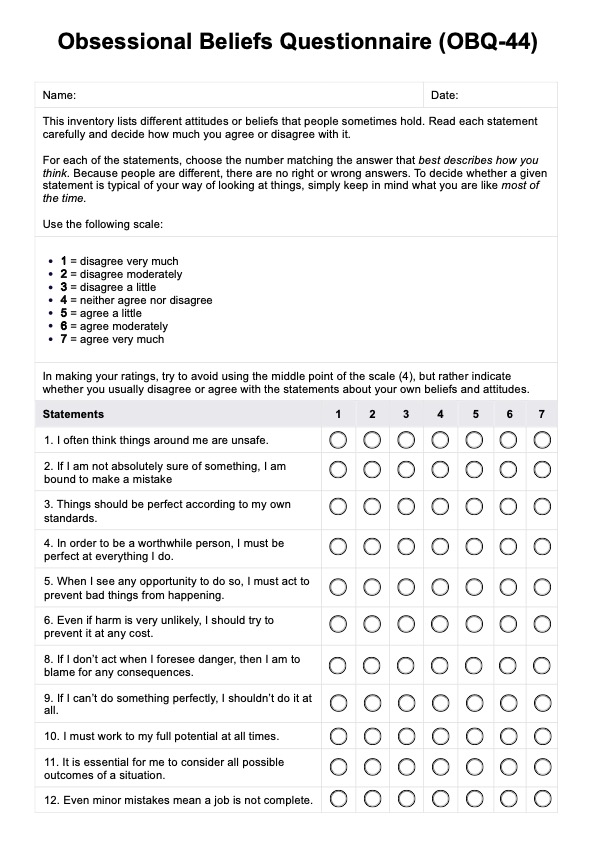
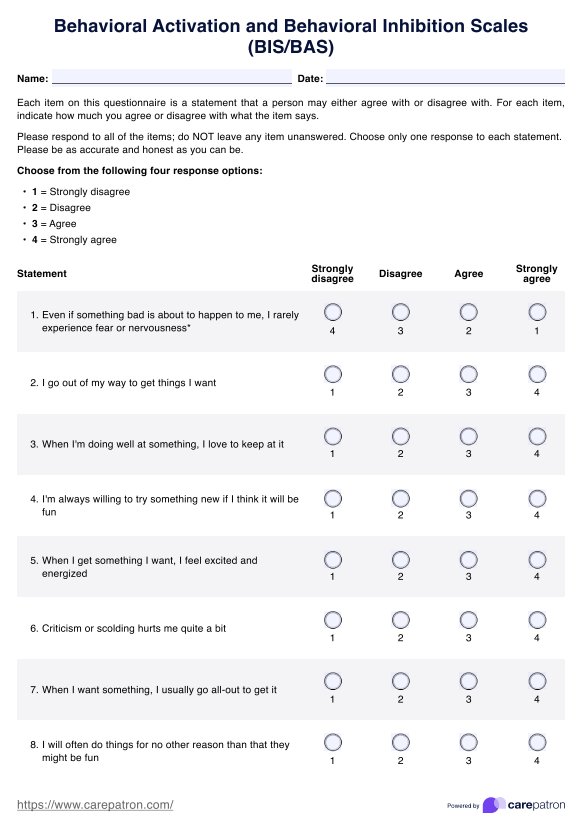
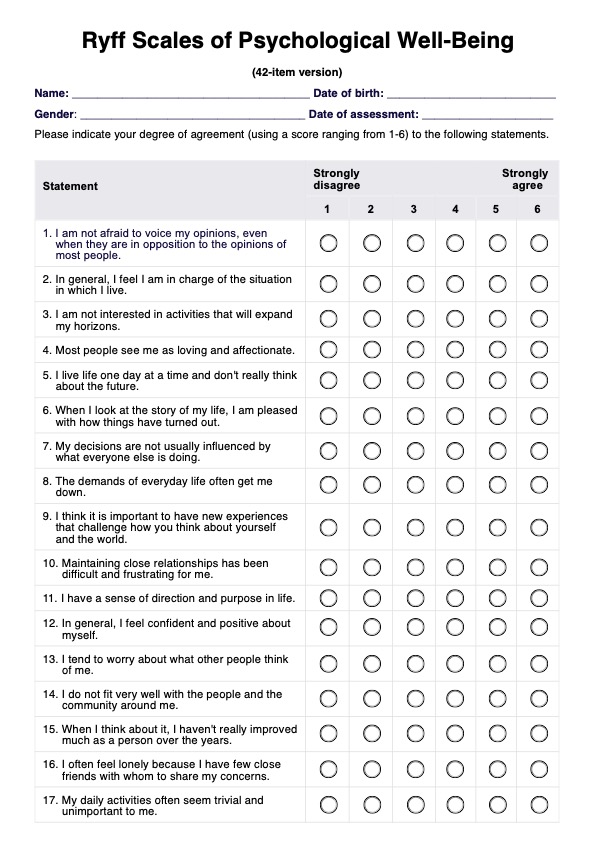
Questionnaires
Clients may be asked to fill out questionnaires like the Epworth Sleepiness Scale to learn about their sleep disturbances, habits, mood, and daily routines. These help them understand how insomnia affects their lives and can guide the diagnosis and treatment plan.
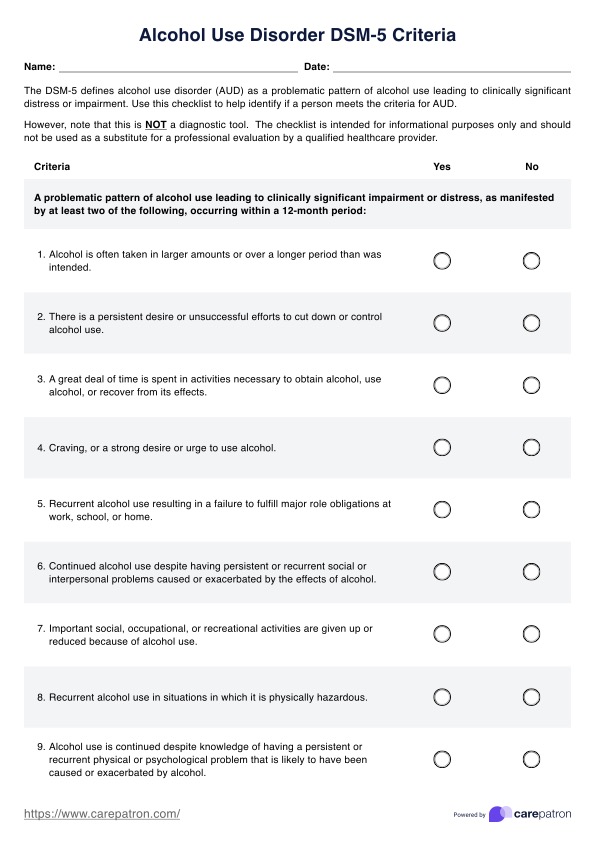
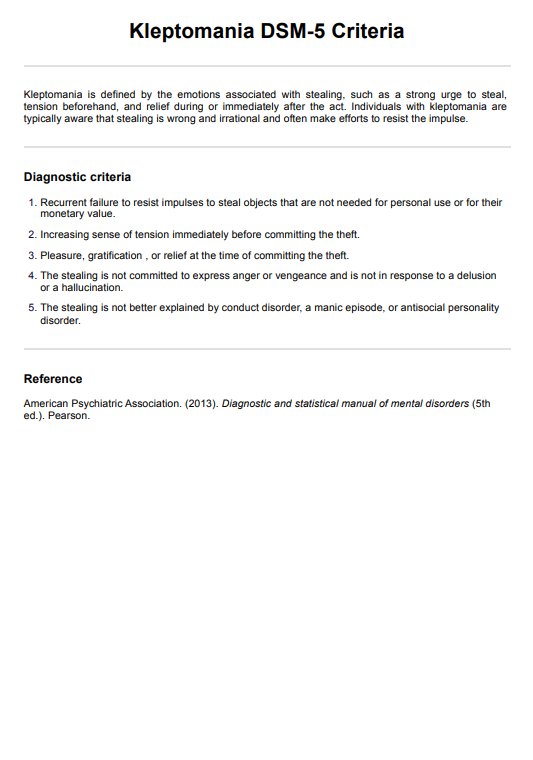
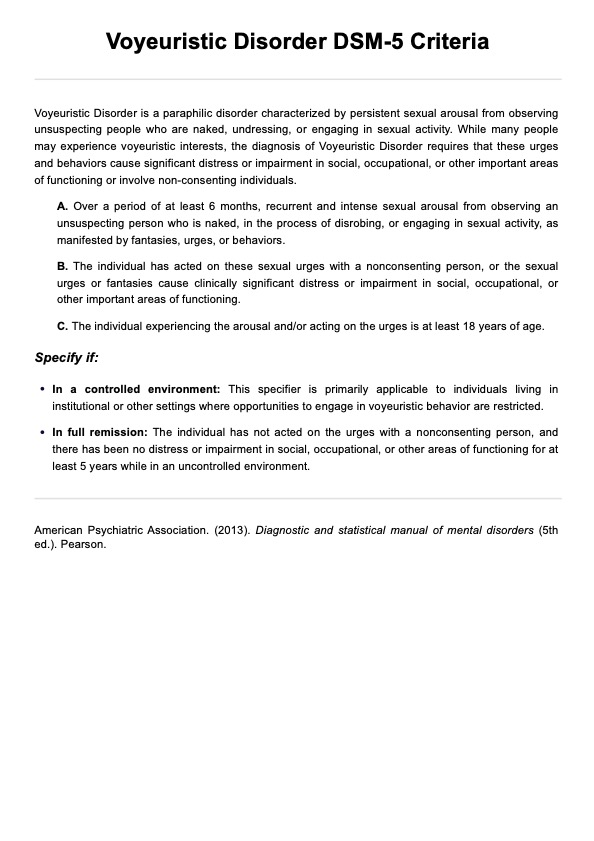
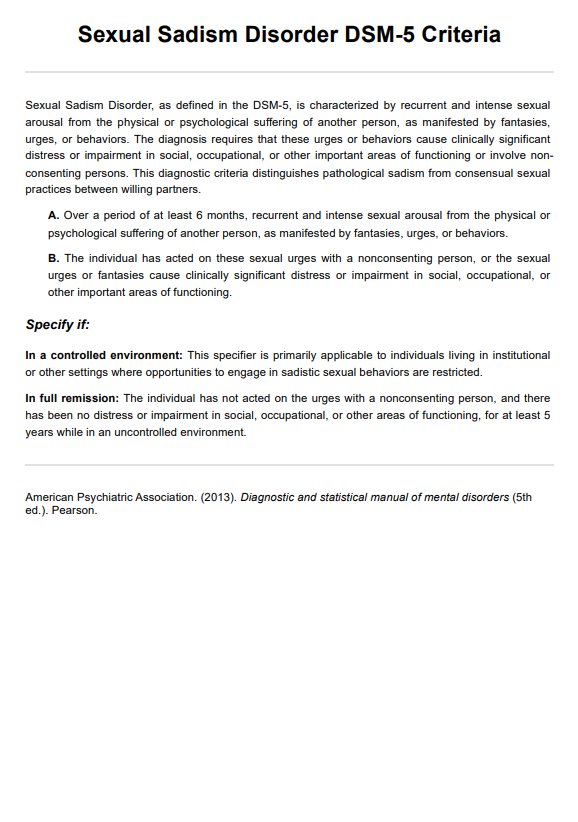
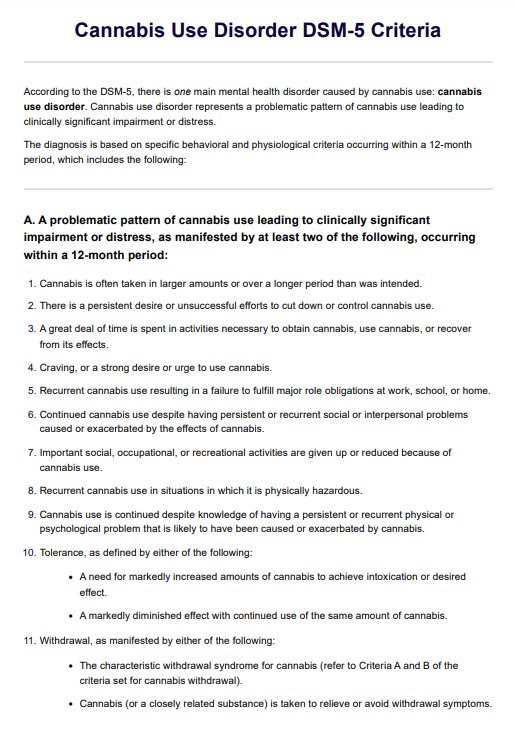
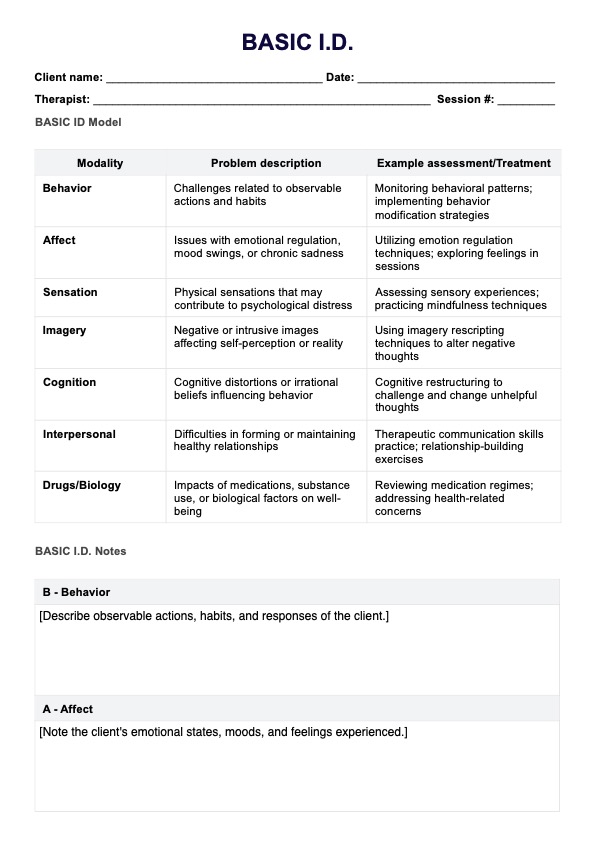
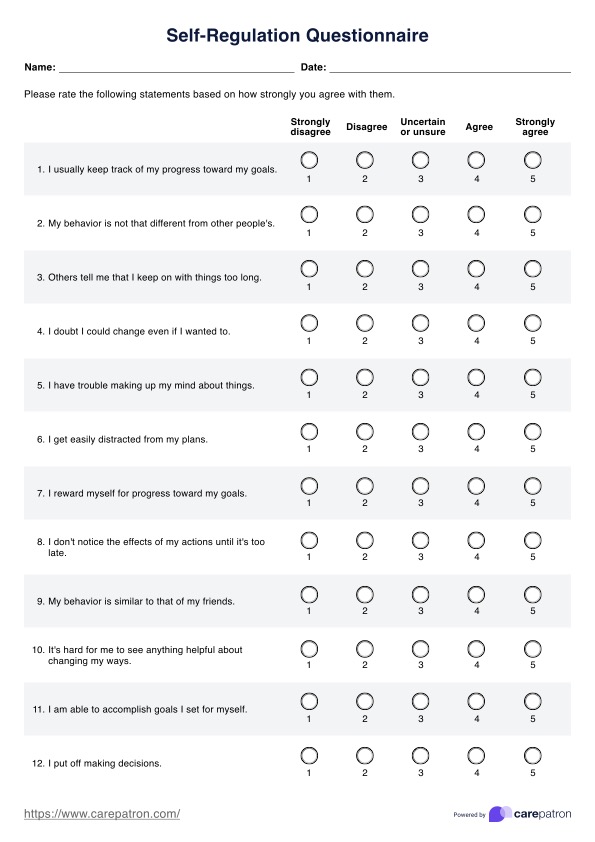
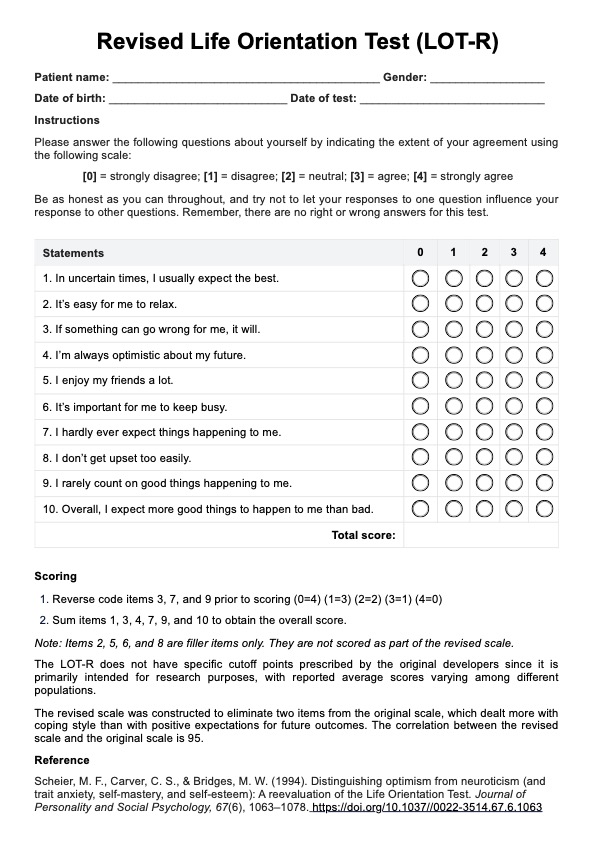
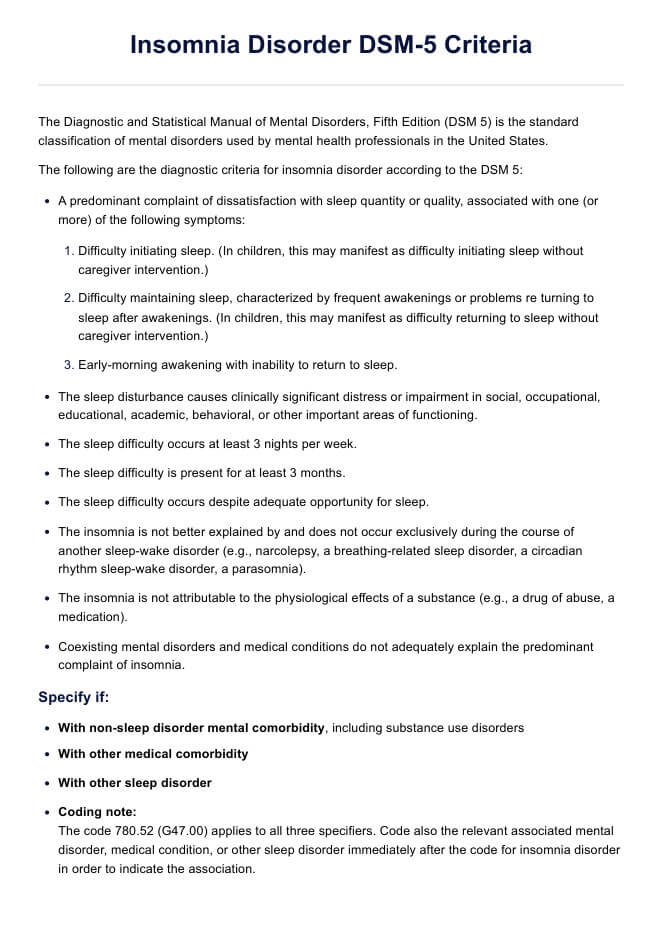
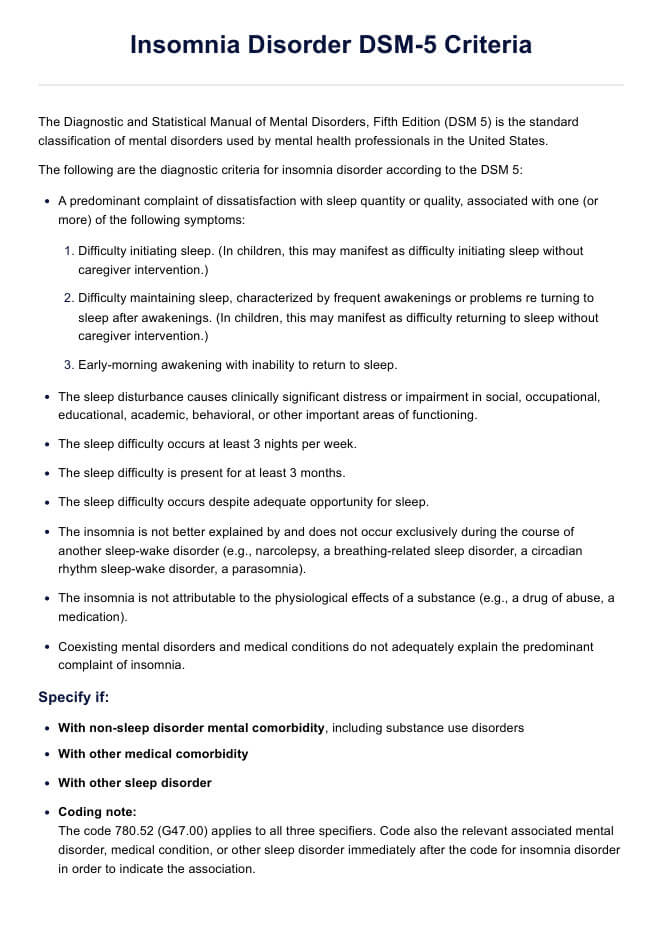
DSM-5 insomnia disorder diagnosis criteria
Together with the evaluations above earlier, the clinician compares the patient's symptoms following the diagnostic criteria outlined in the DSM 5, which are as follows:
Criterion A. A predominant complaint of dissatisfaction with sleep quantity or quality, associated with one (or more) of the following symptoms:
- Difficulty initiating sleep. (In children, this may manifest as difficulty initiating sleep without caregiver intervention.)
- Difficulty maintaining sleep, characterized by frequent awakenings or problems re turning to sleep after awakenings. (In children, this may manifest as difficulty returning to sleep without caregiver intervention.)
- Early-morning awakening with inability to return to sleep.
Criterion B. The sleep disturbance causes clinically significant distress or impairment in social, occupational, educational, academic, behavioral, or other important areas of functioning.
Criterion C. The sleep difficulty occurs at least 3 nights per week.
Criterion D. The sleep difficulty is present for at least 3 months.
Criterion E. The sleep difficulty occurs despite adequate opportunity for sleep.
Criterion F. The insomnia is not better explained by and does not occur exclusively during the course of another sleep-wake disorder (e.g., narcolepsy, a breathing-related sleep disorder, a circadian rhythm sleep-wake disorder, a parasomnia).
Criterion G. The insomnia is not attributable to the physiological effects of a substance (e.g., a drug of abuse, a medication).
Criterion H. Coexisting mental disorders and medical conditions do not adequately explain the predominant complaint of insomnia.
Specify if:
- With non-sleep disorder mental comorbidity, including substance use disorders
- With other medical comorbidity
- With other sleep disorder
Coding note: The code 780.52 (G47.00) applies to all three specifiers. Code also the relevant associated mental disorder, medical condition, or other sleep disorder immediately after the code for insomnia disorder in order to indicate the association.
Specify if:
- Episodic: Symptoms last at least 1 month but less than 3 months.
- Persistent: Symptoms last 3 months or longer.
- Recurrent: Two (or more) episodes within the space of 1 year.
Note: Acute and short-term insomnia (i.e., symptoms lasting less than 3 months but otherwise meeting all criteria with regard to frequency, intensity, distress, and/or impairment) should be coded as another specified insomnia disorder.
Differences between the DSM-4 and DSM-5 criteria
In the DSM-4, insomnia disorder was previously known as primary insomnia and was categorized as a sleep disorder. Changes were made in the DSM-4 criteria, which were expanded from five to eight in the DSM-5 version. Additionally, specifiers were introduced to provide more precise diagnoses, aiding in developing more effective treatments for each client (American Psychiatric Association, 2013b; Substance Abuse and Mental Health Services Administration, 2016).
How is insomnia disorder treated and managed?
Insomnia treatment and management can be done through non-pharmacological and pharmacological treatments (Kaur et al., 2023; National Heart, Lung, and Blood Institute, 2022):
Non-pharmacological
In this form of management, patients are advised to form healthy sleeping habits and sleep hygiene, like limiting their intake of caffeine and making adjustments to their bedroom environment. Cognitive behavioral therapy for insomnia (CBTi) is the most common form of therapy, which includes sleep education, relaxation techniques, sleep restriction therapy, stimulus control therapy, and cognitive and behavioral therapy. A licensed psychologist can administer this.
Pharmacological
Prescription medicines like zolpidem and eszopiclone can be helpful, but they are typically intended for short-term use due to potential side effects. Additionally, off-label medications, such as certain antidepressants, may be prescribed to aid sleep. Over-the-counter options, including melatonin supplements and antihistamines, are also available. Remember that sleep medications should not be the first choice for treating insomnia.
References
American Psychiatric Association. (2013a). Diagnostic and statistical manual of mental disorders (5th ed.). Pearson.
American Psychiatric Association. (2013b). Highlights of changes from DSM-IV-TR to DSM-5. https://www.psychiatry.org/File%20Library/Psychiatrists/Practice/DSM/APA_DSM_Changes_from_DSM-IV-TR_-to_DSM-5.pdf
Kaur, H., Spurling, B. C., & Bollu, P. C. (2023). Chronic insomnia. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK526136/
Substance Abuse and Mental Health Services Administration. (2016). Table 3.36, DSM-IV to DSM-5 insomnia disorder comparison. Substance Abuse and Mental Health Services Administration (US). https://www.ncbi.nlm.nih.gov/books/NBK519704/table/ch3.t36/
Commonly asked questions
People with different anxiety disorders often have trouble sleeping. This includes those with generalized anxiety disorder (GAD), obsessive-compulsive disorder (OCD), and post-traumatic stress disorder (PTSD). These anxiety issues can make it hard to fall asleep, stay asleep, or get restful sleep, making their anxiety worse and affecting their daily life.
Obstructive sleep apnea is when the airway becomes blocked during sleep, causing an individual to stop breathing temporarily. If untreated, this can lead to loud snoring, daytime tiredness, and other health problems. Often, this sleep disorder co-exists with insomnia.
Yes, insomnia is often linked to major depressive disorder and is considered its core symptom. People with depression frequently have trouble falling asleep or staying asleep.






-template.jpg)