Nightmare Disorder DSM-5 Criteria
Learn the diagnosis criteria and treatment options for nightmare disorder with this comprehensive guide on Nightmare Disorder DSM-5 Criteria.


What is nightmare disorder?
Besides helping us function, sleep makes it even more enjoyable because it allows us to dream. Dreaming is a normal part of falling asleep. However, not every night brings pleasant dreams. Sometimes, one can have nightmares.
Nightmares, which are vividly remembered upon waking, mainly occur during rapid-eye movement (REM) sleep and are more frequent in the second half of the night when dreams are more prolonged and intense. Sleep deprivation and fragmentation, jet lag, and certain medications can cause nightmares to occur earlier in the night (American Psychiatric Association, 2013a). Occasional nightmares are common, but recurring nightmares can be troubling and may lead to nightmare disorder.
Nightmare disorder involves frequent, vivid nightmares that cause distress or impair daily functioning. While common in children (onset usually between 3 and 6 years), about 4% of adults experience this disorder, often linked to stress, anxiety symptoms, or trauma. Adult males report nightmares less often than females, with themes of physical aggression or war, while females tend to have nightmares about sexual harassment or loss (American Psychiatric Association, 2013a; United Brain Association, n.d.). This disorder can make one wake up feeling alert and deeply distressed.
Nightmare Disorder DSM-5 Criteria Template
Nightmare Disorder DSM-5 Criteria Sample
How is nightmare disorder diagnosed?
Nightmare disorder is diagnosed through several evaluations. Usually, it starts with a physical exam and evaluation of the patient's family history to identify any underlying health issues, where patients are asked detailed questions about their sleep habits and nightmares.
A sleep study may also be conducted to monitor sleep patterns overnight and rule out other sleep disorders. The patient's symptoms are then compared to the criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders-5 (DSM-5) to diagnose the mental health condition. Based on all this information, the clinician can determine if the patient has nightmare disorder and provide the best course of treatment, especially if the disorder is associated with other conditions like post traumatic stress disorder.
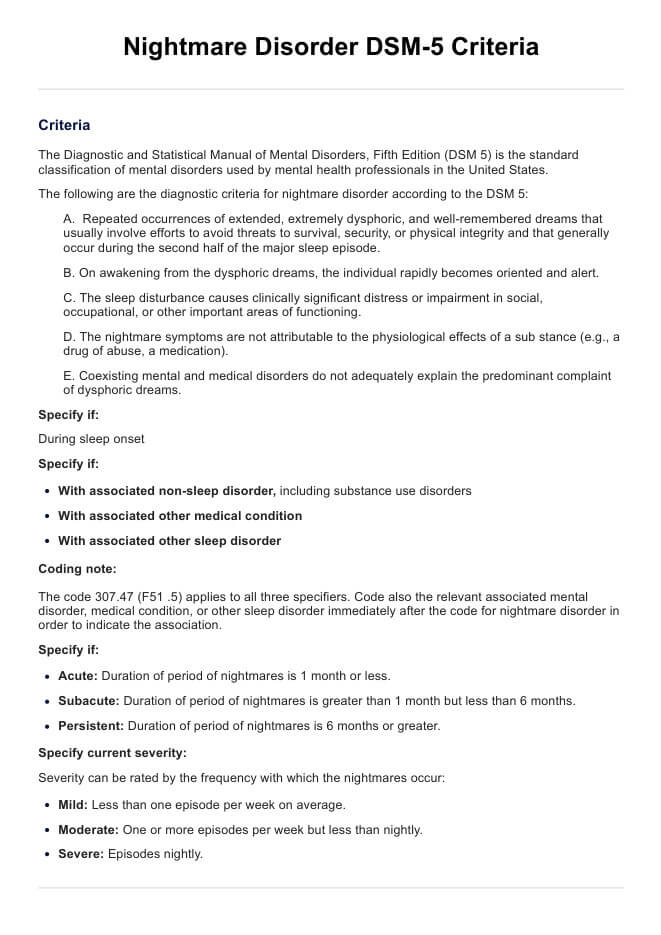
DSM-5 nightmare disorder diagnostic criteria
The following are the diagnostic criteria for nightmare disorder according to the DSM-5:
A. Repeated occurrences of extended, extremely dysphoric, and well-remembered dreams that usually involve efforts to avoid threats to survival, security, or physical integrity and that generally occur during the second half of the major sleep episode.
B. On awakening from the dysphoric dreams, the individual rapidly becomes oriented and alert.
C. The sleep disturbance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning.
D. The nightmare symptoms are not attributable to the physiological effects of a substance (e.g., a drug of abuse, a medication).
E. Coexisting mental and medical disorders do not adequately explain the predominant complaint of dysphoric dreams.
Specify if:
- During sleep onset
Specify if:
- With associated non-sleep disorder, including substance use disorders
- With associated other medical conditions
- With associated other sleep disorder
Coding note: The code 307.47 (F51 .5) applies to all three specifiers. Code also the relevant associated mental disorder, medical condition, or other sleep disorder immediately after the code for nightmare disorder in order to indicate the association.
Specify if:
- Acute: Duration of period of nightmares is 1 month or less.
- Subacute: Duration of period of nightmares is greater than 1 month but less than 6 months.
- Persistent: Duration of period of nightmares is 6 months or greater.
Specify current severity:
Severity can be rated by the frequency with which the nightmares occur:
- Mild: Less than one episode per week on average.
- Moderate: One or more episodes per week but less than nightly.
- Severe: Episodes nightly.
Differences between DSM-4 and DSM-5
The DSM-5 criteria for Nightmare Disorder build on the DSM-4 by specifying that the nightmares involve efforts to avoid threats and are dysphoric. While both versions note that upon awakening the person is quickly oriented and that the nightmares cause significant distress or impairment, DSM-5 adds clarity by excluding symptoms caused by substances or other disorders. Additionally, DSM-5 introduces specifiers for the duration (acute, subacute, persistent) and severity (mild, moderate, severe) of the nightmares, which are absent in DSM-4, allowing for a more detailed and accurate diagnosis (American Psychiatric Association, 2000; American Psychiatric Association, 2013).
Management and treatment of nightmare disorder
While nightmares usually resolve on their own in children during adolescence, treatment of nightmare disorder involves various methods, which can include therapy and lifestyle modification like sleep hygiene (Summer & Singh, 2022; United Brain Association, n.d.).
In 2010, the American Academy of Sleep Medicine commissioned a task force to draft the Best Practice Guide for the Treatment of Nightmare Disorder in Adults. Following this, in 2018, another task force was convened to formulate AASM's position statements based on the literature review in the best practice guide. The position statements are as follows (Morgenthaler et al., 2018):
- The following therapy is recommended for the treatment of PTSD-associated nightmares and nightmare disorder: image rehearsal therapy.
- The following therapies may be used for the treatment of PTSD-associated nightmares: cognitive behavioral therapy; cognitive behavioral therapy for insomnia; eye movement desensitization and reprocessing; exposure, relaxation, and rescripting therapy; the atypical antipsychotics olanzapine, risperidone and aripiprazole; clonidine; cyproheptadine; fluvoxamine; gabapentin; nabilone; phenelzine; prazosin; topiramate; trazodone; and tricyclic antidepressants.
- The following therapies may be used for the treatment of nightmare disorder: cognitive behavioral therapy; exposure, relaxation, and rescripting therapy; hypnosis; lucid dreaming therapy; progressive deep muscle relaxation; sleep dynamic therapy; self-exposure therapy; systematic desensitization; testimony method; nitrazepam; prazosin; and triazolam.
- The following are not recommended for the treatment of nightmare disorder: clonazepam and venlafaxine.
- The ultimate judgment regarding propriety of any specific care must be made by the clinician, in light of the individual circumstances presented by the patient, accessible treatment options, and resources.
To help prevent nightmare disorder, encourage your clients to stick to a regular sleep schedule, practice relaxation techniques to manage stress, and address any underlying mental health concerns. After all, prioritizing good quality sleep is vital to improve overall well-being.
References
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.).
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Pearson.
Morgenthaler, T. I., Auerbach, S., Casey, K. R., Kristo, D., Maganti, R., Ramar, K., Zak, R., & Kartje, R. (2018). Position paper for the treatment of nightmare disorder in adults: An American Academy of Sleep Medicine position paper. Journal of Clinical Sleep Medicine, 14(06), 1041–1055. https://doi.org/10.5664/jcsm.7178
Semiz, U. B., Basoglu, C., Ebrinc, S., & Cetin, M. (2008). Nightmare disorder, dream anxiety, and subjective sleep quality in patients with borderline personality disorder. Psychiatry and Clinical Neurosciences, 62(1), 48–55. https://doi.org/10.1111/j.1440-1819.2007.01789.x
Summer, J., & Singh, A. (2022, December 16). What is nightmare disorder? Sleep Foundation. https://www.sleepfoundation.org/nightmares/nightmare-disorder
United Brain Association. (n.d.). Nightmare disorder.
Commonly asked questions
Night terrors and nightmares are both types of parasomnias. Nightmares usually occur during rapid eye movement (REM) sleep, whereas night terrors, also known as sleep terrors, typically happen during non-REM (NREM) or slow wave sleep.
Yes, though it can also be independently diagnosed, nightmare disorder can emerge alongside other issues like posttraumatic stress disorder (PTSD). It's also linked to mental health conditions like depression and anxiety and other sleep disorders like insomnia and sleep apnea.
A study found that individuals with BPD have more nightmares, higher levels of dream anxiety, and more disturbed sleep compared to people without the disorder (Semiz et al., 2008).


















-template.jpg)


















































































