Stroke treatment guidelines provide healthcare providers with standardized protocols and best practices for optimal care for stroke patients. By following these guidelines, providers can ensure timely interventions, reduce treatment variability, and improve patient outcomes.
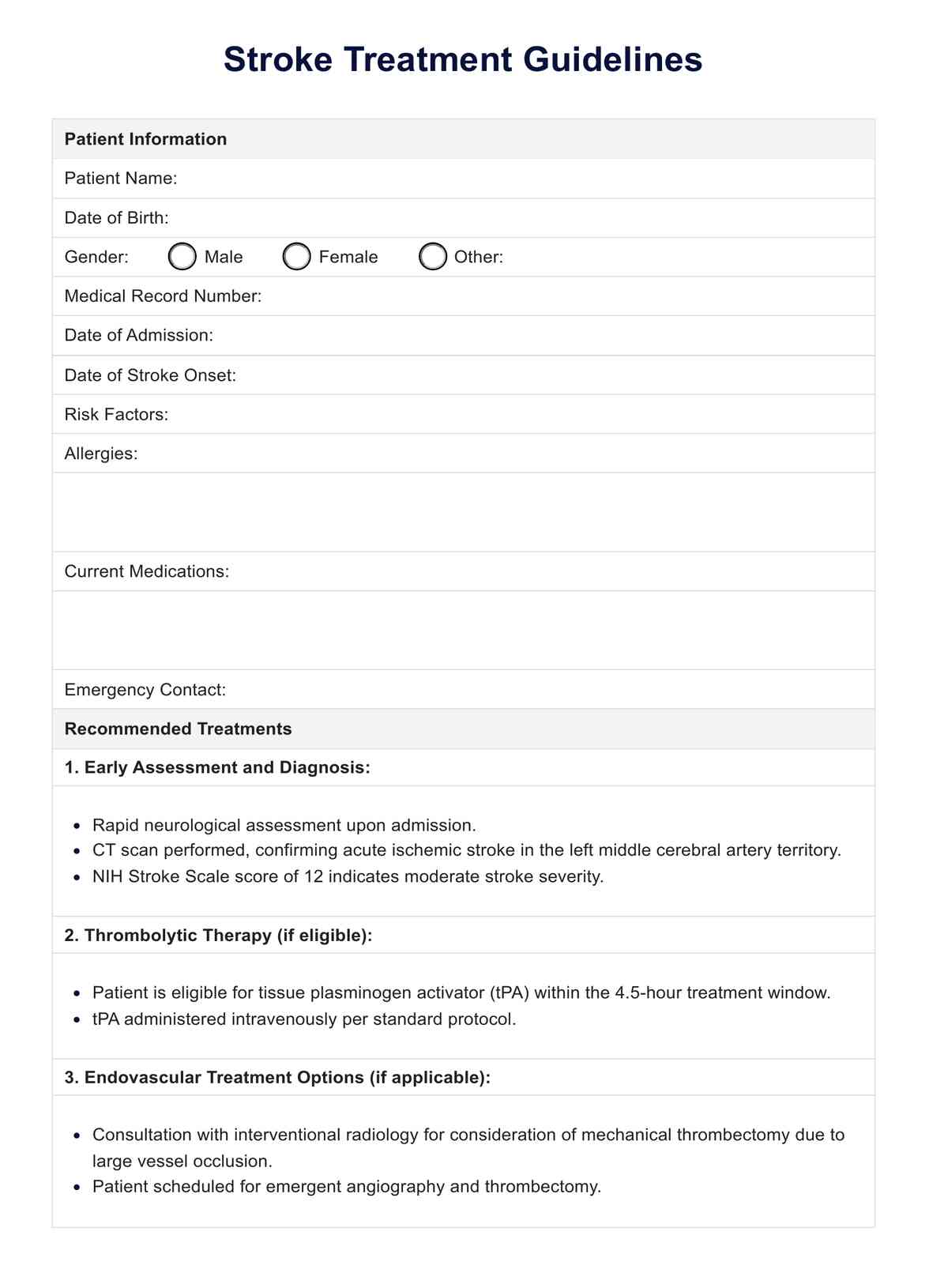
Stroke Treatment Guidelines
Explore evidence-based Stroke Treatment Guidelines for effective care. Expert recommendations to optimize stroke management.
Stroke Treatment Guidelines Template
Commonly asked questions
Healthcare professionals should familiarize themselves with the latest stroke treatment guidelines and incorporate them into their clinical practice. This involves following recommended early assessment, diagnosis, and treatment protocols and regularly consulting guidelines for updates and revisions.
While stroke treatment guidelines offer valuable guidance for most patients, healthcare providers must also consider individual patient factors and preferences when making treatment decisions. Guidelines should be used as a framework for care, with adjustments made based on patient-specific needs and circumstances.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











