Nursing interventions without an order, or independent nursing interventions, are actions that nurses assess and implement based on their professional judgment, without needing a physician’s directive. These include safety interventions, patient education, and active listening.
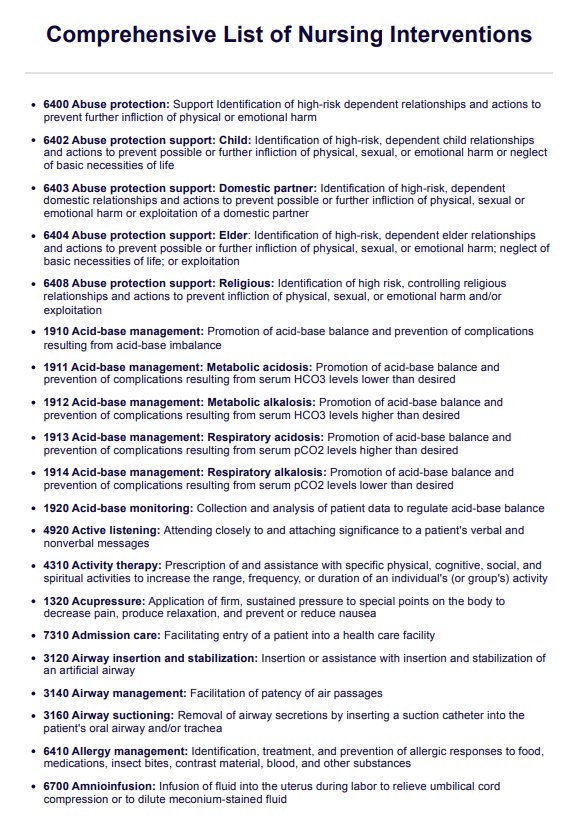
Comprehensive List of Nursing Interventions
Access our free List of Nursing Interventions PDF. Streamline patient care with this comprehensive, editable resource based on the NIC's l5th edition.
Comprehensive List of Nursing Interventions Template
Commonly asked questions
There are numerous types of nursing interventions, categorized into nursing intervention domains like community nursing interventions, physiological nursing interventions, and safety interventions. The NIC system identifies hundreds of specific interventions, each improving patient care.
These interventions range from administering medications to facilitating public health initiatives and community nursing interventions that promote overall health in the community.
The five main nursing actions used in a nursing practice include:
- Assessment: Nurses assess the patient’s condition, including medical diagnoses and physical health.
- Diagnosis: Identifying nursing diagnoses based on patient data.
- Planning: Developing nursing care plans to address the patient’s needs.
- Implementation: Applying key nursing interventions, like administering medication or collaborating with healthcare professionals and physical therapists.
- Evaluation: Evaluating the effectiveness of interventions, adjusting nursing care to achieve better outcomes and improve patient safety. These actions are fundamental to a nursing career and ensure the delivery of comprehensive care.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











