CMS 1450 Claim Form
Explore CMS 1450s, used by healthcare providers for billing Medicare and other insurers. Ensuring accuracy on these forms leads to efficient reimbursements.


What is a CMS 1450 Claim Form?
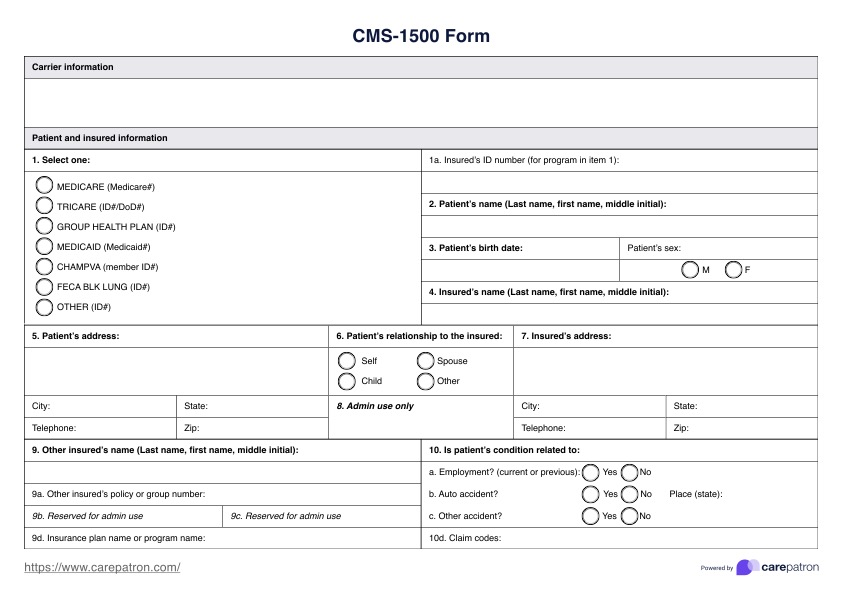
The claim form, or the UB-04 form, is a vital resource used within the healthcare industry. It is a standardized form that hospitals, nursing homes, and other institutional providers use to bill insurance companies for services rendered. This form is universally recognized across the healthcare sector by both government-run and private insurance companies.
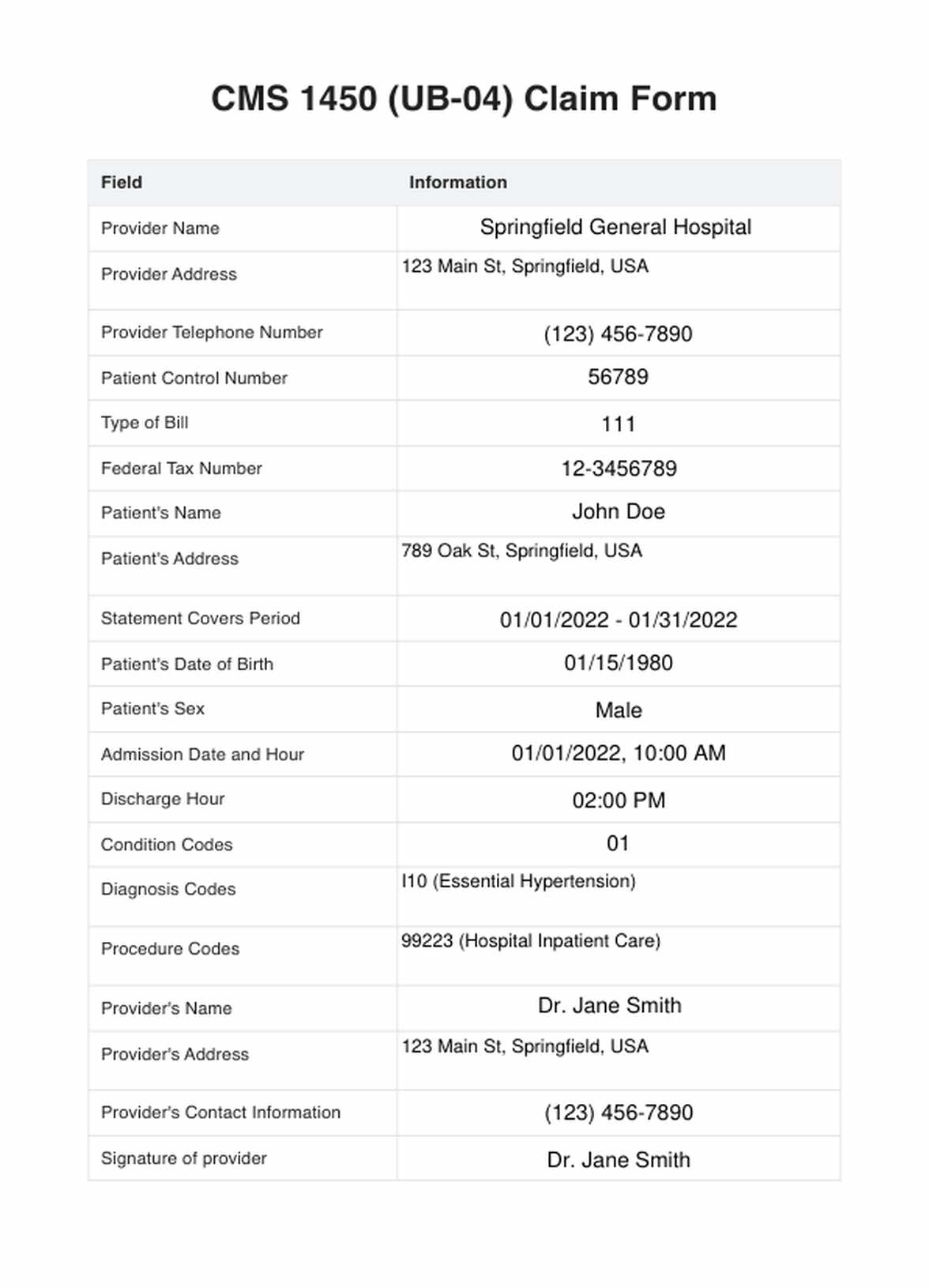
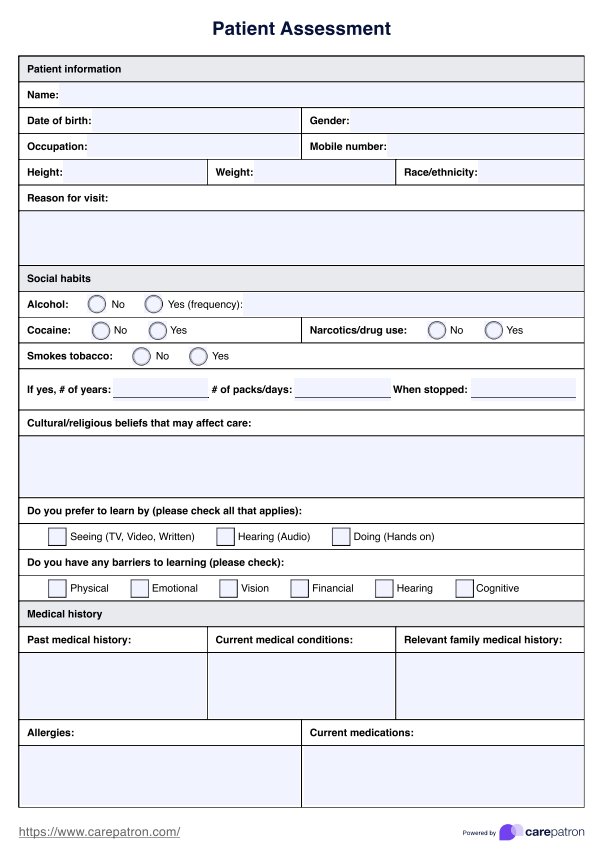
This form plays an essential role in medical billing, allowing healthcare providers to receive reimbursement for their services. The form contains comprehensive information about the patient, the healthcare provider, and the specifics of the service provided. This includes details like the patient's personal and demographic data, the provider's information, the diagnoses, the procedures performed, and the corresponding charges.
One significant aspect of the CMS 1450 form is its use of specific codes for diagnoses and procedures. These codes are based on the International Classification of Diseases (ICD) system - a critical tool in modern healthcare that standardizes the classification of medical conditions and treatments. This standardized coding helps ensure clear communication between healthcare providers and insurers, reducing the chances of misunderstandings or errors.
Submitting a correctly filled CMS 1450 form is a key step in ensuring the healthcare provider receives appropriate compensation from the insurance company. However, it's important to note that different insurance companies may have unique guidelines for filling out and submitting this form.
Furthermore, the CMS 1450 form is integral to managing electronic health records (EHRs). EHRs are digital versions of traditional patient charts, updated in real-time, providing a comprehensive and up-to-date patient care history. The data captured on the CMS 1450 form feeds into these EHRs, contributing to accurate and efficient patient information management.
To find out more about streamlining medical billing, feel free to watch this video:
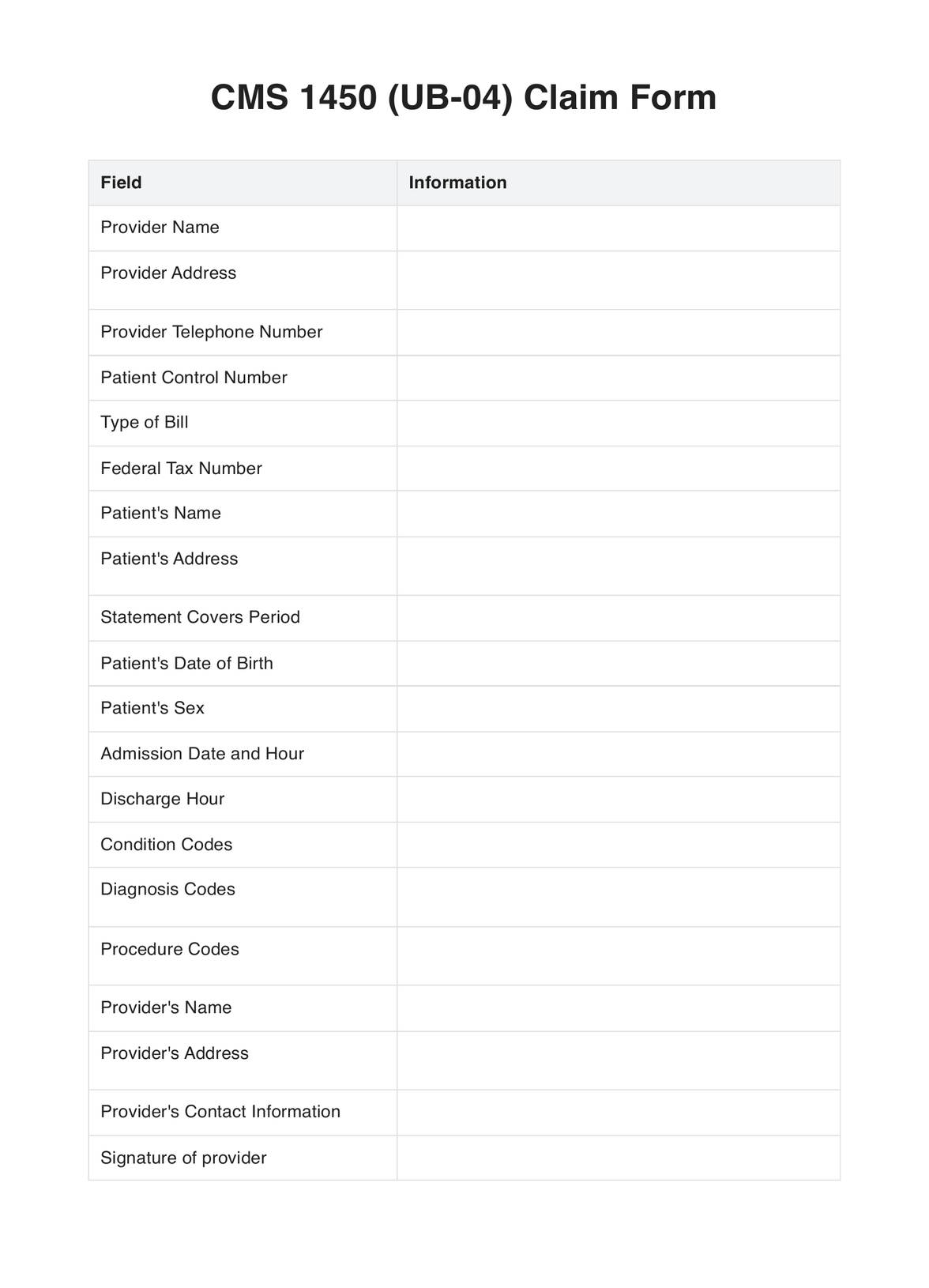
CMS 1450 Claim Form Template
CMS 1450 Claim Form Example
How does it work?
Understanding the process of filling out a printable CMS 1450 form is crucial for healthcare providers. Here's a comprehensive guide on how to use this form:
Step 1: Obtain the Printable CMS 1450 Form
Start by acquiring the printable CMS 1450 form from the official CMS website or other trusted sources. Ensure the printout is clear and legible to prevent complications during completion and submission.
Step 2: Fill in the Patient's Information
Next, fill in the patient's details on the form. This includes their full name, address, date of birth, social security number, and insurance policy number for accurate identification and insurance verification.
Step 3: Input the Provider's Details
On the printable CMS 1450 form, input the healthcare provider's details, such as name, address, and NPI number. This information is necessary to verify the provider's identity and ensure correct reimbursement processing.
Step 4: Provide Diagnosis and Treatment Details
In the relevant section of the form, enter diagnosis and treatment details using specific ICD codes. These codes standardize medical conditions and treatments across healthcare platforms.
Step 5: Enter the Billing Information
In this printable CMS 1450 form section, input the service charges and detailed payer information. This data identifies who is financially responsible for the services provided.
Step 6: Review and Submit the Printable CMS 1450 Form
Lastly, thoroughly review the filled form for accuracy. Any inaccuracies or omissions can lead to claim denial or processing delays. After confirming all details are correct, submit the form to the insurance company.
When would you use this Template?
Here are scenarios when this template is exceptionally useful:
- Hospital Billing: If you work in a hospital billing department, the CMS 1450 form is indispensable. It's used to submit claims for services ranging from surgeries, diagnostics, and treatments to room and board charges.
- Outpatient Clinics: Outpatient facilities also frequently use the CMS 1450 form. Whether for routine medical examinations, minor surgical procedures, or diagnostic tests, this form helps streamline the billing process.
- Home Healthcare Agencies: Home healthcare providers use the CMS 1450 form to bill for nursing care, physical therapy, or health aide services provided at a patient's home.
- Nursing Facilities: Long-term care facilities and nursing homes use the CMS 1450 form to bill for room and board charges, rehabilitation, and other daily care services.
- Data Collection: Beyond billing, healthcare institutions use the CMS 1450 form for data collection and analysis. The form provides valuable insights into service usage patterns, cost of services, and the efficiency of the insurance claims process.
- Medical Coding and Billing Education: If you're a student or instructor in medical coding and billing, the CMS 1450 form serves as an excellent educational resource. It offers practical experience in accurately completing claim forms using standard coding systems like the International Classification of Diseases (ICD).
Correctly completing the CMS 1450 form is crucial to ensure timely service reimbursement. Regardless of your role in the healthcare sector - be it a medical coder, billing specialist, or healthcare provider, understanding when and how to use the CMS 1450 form effectively can significantly impact the financial health of your institution.
Benefits
Economical Solution
The CMS 1450 form is free, making it a cost-effective choice for healthcare providers. It eliminates the need to invest in expensive billing software or proprietary forms.
Universal Acceptance
This form is recognized by Medicare and widely accepted by many other insurance carriers. This universal acceptance makes the Free CMS 1450 form a versatile and convenient tool for institutional healthcare providers.
Streamlines Billing
The standardized format of the Free CMS 1450 form simplifies the billing process. It ensures a uniform billing system across different institutions, leading to smoother claim processing.
Enhances Accuracy
By employing standardized codes for diagnoses and treatments, the Free CMS 1450 form minimizes errors, enhancing claims' accuracy and expediting reimbursements.
Valuable for Data Collection
Aside from its primary function as a billing form, the Free CMS 1450 also serves as an effective tool for data collection. It provides valuable insights into service utilization, costs, and insurance claim trends.
Educational Tool
The Free CMS 1450 form is an excellent resource for students and educators in medical coding and billing. It provides hands-on experience in accurately filling out claim forms, a crucial skill in healthcare administration.
Research & Evidence
The CMS 1450 form, also known as the UB-04 form, was developed by the Centers for Medicare and Medicaid Services (CMS), a federal agency within the United States Department of Health and Human Services. The primary goal behind its development was to standardize and streamline the billing process for institutional providers.
Before the introduction of the CMS 1450 form, healthcare institutions used a variety of forms and formats to bill for their services, leading to inconsistencies and inefficiencies in the billing process. CMS introduced the UB-04 form in 2007 to address this issue, replacing the older UB-92 form.
The design of the CMS 1450 form is based on research into best practices in healthcare billing. It leverages standardized codes, such as those from the International Classification of Diseases (ICD) system, to represent diagnoses and treatments. This ensures uniformity in how healthcare services are reported and billed, regardless of the specific institution or provider.
Numerous studies and audits have demonstrated the effectiveness of the CMS 1450 form in enhancing the efficiency and accuracy of the billing process. For example, a study published in the Journal of Healthcare Management found that the standardization of billing forms like the CMS 1450 can significantly reduce errors and improve claim processing speed.
Moreover, the CMS 1450 form has been widely accepted and adopted by healthcare institutions across the U.S., further evidencing its utility. Today, it's used for billing Medicare and commercial insurers, making it a versatile tool for institutional healthcare providers.
References
- | Medicare Billing: Form CMS-1450 and the 837 Institutional. (n.d.). https://www.cms.gov/Outreach-and-Education/MLN/WBT/MLN7388180-MLN-WBT-1450/index.html
- A guide to the CMS 1450 claim form. (n.d.). http://www.mb-guide.org/cms-1450-instructions.html
- CMS 1450 | CMS. (n.d.). https://www.cms.gov/Medicare/CMS-Forms/CMS-Forms/CMS-Forms-Items/CMS1196256
- Institutional paper claim form (CMS-1450) | CMS. (n.d.). https://www.cms.gov/Medicare/Billing/ElectronicBillingEDITrans/15_1450
- Medicare billing: Form CMS-1450 and the 837 Institutional | Guidance Portal. (n.d.). https://www.hhs.gov/guidance/document/medicare-billing-form-cms-1450-and-837-institutional
Commonly asked questions
The CMS 1450, or the UB-04 form, is primarily used by institutional providers like hospitals, nursing facilities, and outpatient clinics. It's used to bill Medicare Administrative Contractors (MACs) when a paper claim is allowed.
The CMS 1450 form is used when an institutional provider must submit a reimbursement claim to Medicare or Medicaid. This could be due to providing healthcare services like treatments, procedures, or supplies. It's typically used when electronic billing is not feasible.
The CMS 1450 form is filled out with information about the institutional provider, the patient, and the services provided. This includes details like the patient's diagnosis, procedures performed, dates of service, and charges. Once completed, it's submitted to the relevant MAC for processing and payment. Software like Carepatron can help streamline completing and submitting these forms.