Also known as hypervolemia, fluid overload happens when too much fluid is in one's body. Patients with kidney conditions often experience this.
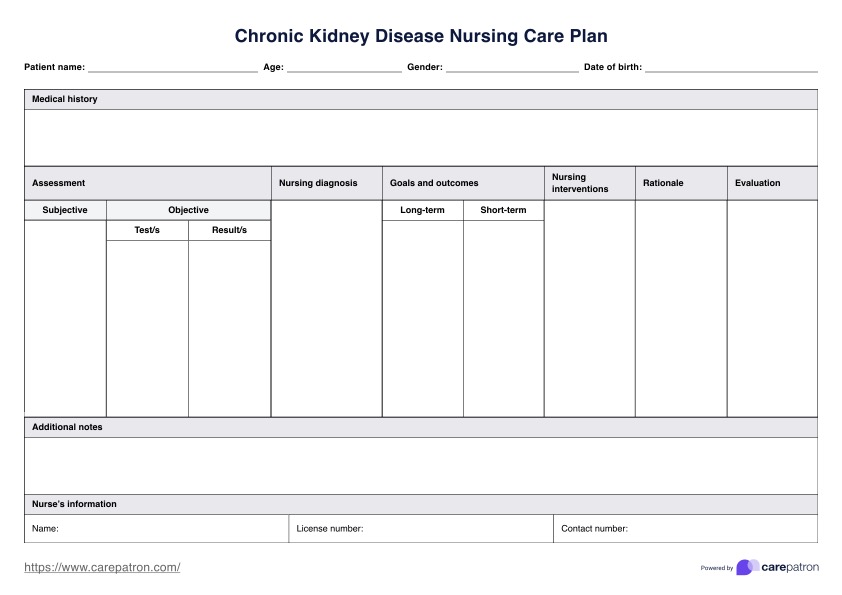
Chronic Kidney Disease Nursing Care Plan
Get comprehensive guidance on diagnosing and managing CKD. Download the Chronic Kidney Disease Nursing Care Plan for personalized patient support.
Chronic Kidney Disease Nursing Care Plan Template
Commonly asked questions
Primary care physicians evaluate patients initially. If kidney disease or abnormalities are confirmed, patients are referred to nephrologists for further assessment and specialized care.
Taking care of the kidneys involves maintaining a healthy lifestyle, including staying hydrated, eating a balanced diet low in salt and processed foods, exercising regularly, avoiding smoking, and managing conditions like diabetes and high blood pressure.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











