The first-line treatment for cholecystitis often involves fasting, intravenous fluids, and pain medication to manage symptoms, and in severe or recurrent cases, surgery to remove the gallbladder (cholecystectomy) may be recommended.
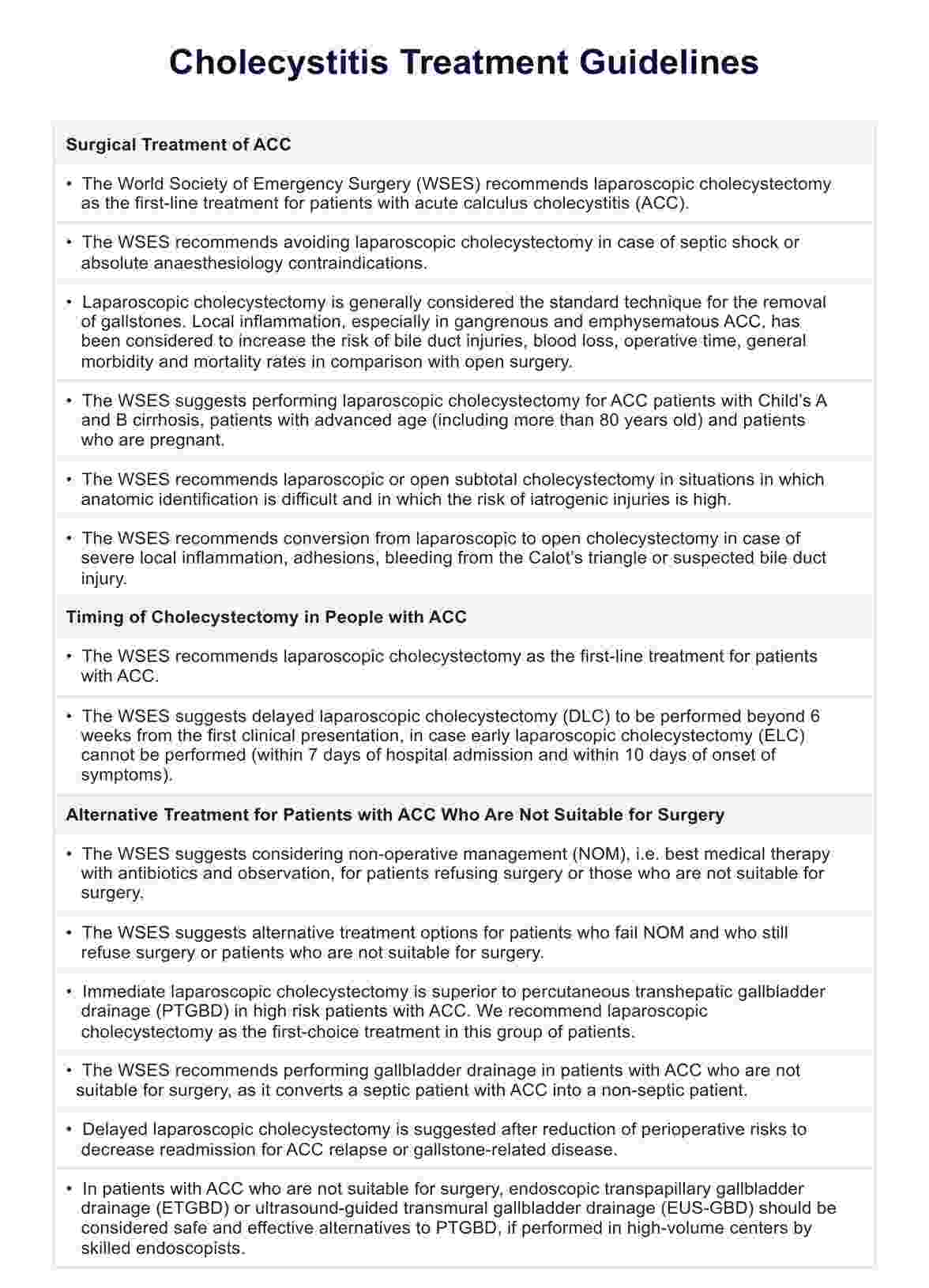
Cholecystitis Treatment Guidelines
Explore our Cholecystitis Treatment Guidelines for managing acute conditions. Download the PDF now.
Use Template
Cholecystitis Treatment Guidelines Template
Commonly asked questions
Common medications for managing cholecystitis include antibiotics to treat or prevent infection and pain relievers to alleviate abdominal discomfort.
Symptoms of cholecystitis typically include severe pain in the upper right abdomen that may radiate to the back or right shoulder, fever, nausea, vomiting, and tenderness over the gallbladder.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











