Cheat Sheet Hospice Documentation Template
Comprehensive guide to hospice documentation: ensure quality care, regulatory compliance, and effective interdisciplinary communication. Streamline your process with expert tips.


An introduction to hospice documentation for hospice nurses
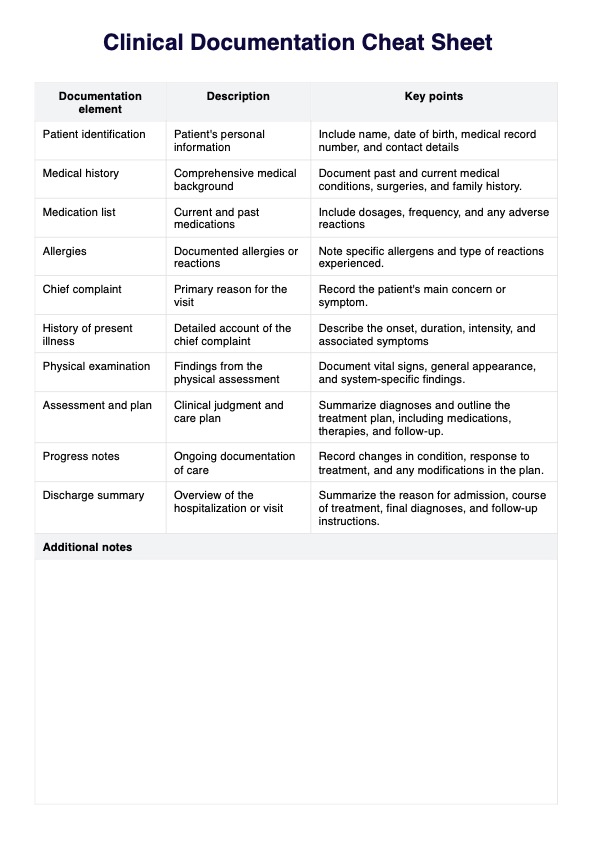
Hospice documentation serves as a comprehensive record-keeping system, capturing the intricate care provided to hospice patients approaching the end of life. This documentation is vital for healthcare professionals, ensuring continuity of care, facilitating communication among the interdisciplinary team, and meeting regulatory requirements.
The documentation begins with an admission assessment, where the patient's medical history, patient's condition, and unique needs are meticulously documented on an admission nursing note or hospice admission note. This foundational information sets the stage for developing an individualized care plan, aligning resources with the patient's preferences and goals.
Hospice documentation goes beyond the physical aspects of care for terminal illness. It encapsulates the psychosocial dimensions of the patient's experience, delving into their emotional and spiritual well-being. It highlights the interventions employed to address psychological distress, foster spiritual support, and enhance the overall quality of life during this profound stage.
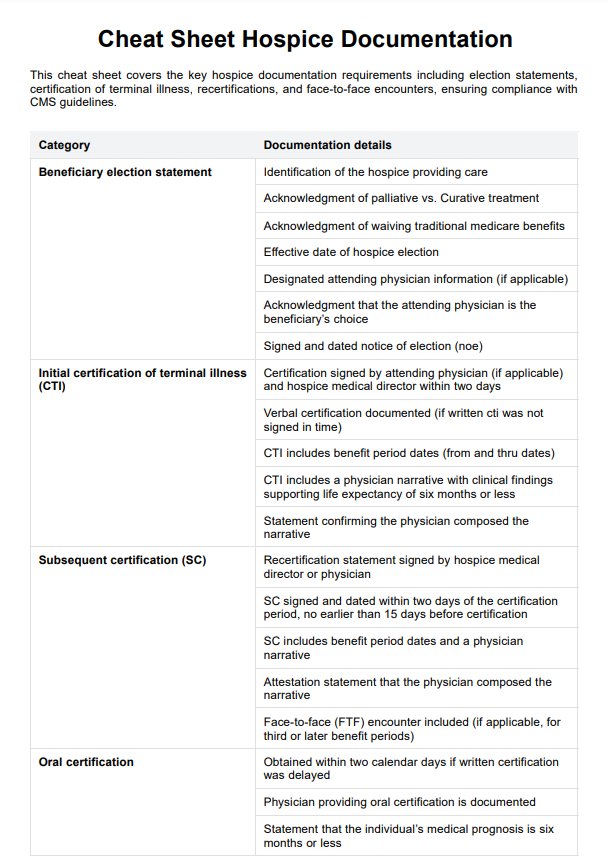
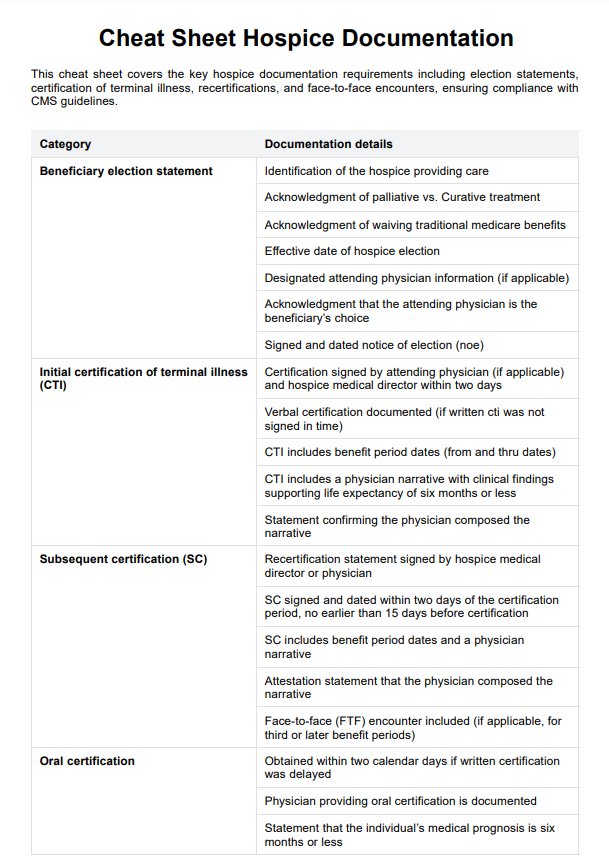
Cheat Sheet Hospice Documentation Template
Cheat Sheet Hospice Documentation Template Example
How to use this Cheat Sheet Hospice Documentation Template
Carepatron's Cheat Sheet for Hospice Documentation provides essential information on documentation requirements, including election statements, certification of terminal illness, recertifications, and face-to-face encounters. This template ensures compliance with CMS guidelines, making it an invaluable resource for hospice providers.
Step 1: Download the resource
Get a copy of the Cheat Sheet Hospice Documentation Template by clicking "Use Template" for the in-app file or "Download" for a PDF version. This page also offers a cheat sheet hospice documentation sample you can use as a guide.
Step 2: Familiarize yourself with the template
Take a few minutes to review the Cheat Sheet for Hospice Documentation Template and make sure you understand its sections, categories, and general structure. This will help you navigate through the document effortlessly.
Step 3: Use as a reference
You can use this template as a reference while documenting hospice care for patients. It includes all the necessary sections and categories, making it easier for you to ensure complete and accurate documentation.
Step 4: Customize to your needs
This template can be customized to suit your specific hospice documentation requirements. You can add or remove sections, modify categories, or include additional information that may be pertinent to your patient's care.
Benefits of Cheat Sheet Hospice Documentation Template
Our Cheat Sheet Hospice Documentation Template offers several benefits for hospice providers, including:
- Ensures compliance with CMS guidelines: Our Cheat Sheet Hospice Documentation Template is meticulously designed to align with CMS requirements, ensuring that your medical records are always in compliance. This helps prevent any regulatory issues and potential penalties, while also promoting optimal patient care through thorough and accurate documentation of the hospice patient’s progress.
- Saves time and effort: This template serves as a quick reference tool, streamlining the documentation process by allowing hospice care providers to easily and efficiently capture important patient care details. By saving valuable time on paperwork, the hospice care team can dedicate more attention to the patient's physical and emotional needs, ensuring the highest standard of care.
- Customizable to fit agency needs: You can tailor the template to reflect your agency’s specific policies and procedures, making it adaptable for any hospital setting or unique hospice environment. This flexibility ensures that your documentation aligns with both regulatory standards and your agency’s approach to patient care, facilitating seamless communication within the care team.
- Easy to use and navigate: Designed with user-friendliness in mind, the template allows hospice care providers to effortlessly input patient information without complications. Its straightforward layout promotes thorough documentation of the patient's progress, ensuring the medical record is always up-to-date and reflective of high-quality hospice care.
Hospice nurse documentation tips
Good documentation is crucial to hospice nursing, ensuring quality and compassionate end-of-life care. Here are some hospice documentation tips for hospice nurses to enhance their documentation:
Document at the bedside
Hospice nurses should always document care while at the bedside of the hospice patient. This ensures accuracy in recording vital signs, pain levels, and other symptom management efforts. Bedside documentation also helps the hospice team stay informed about the patient’s current condition, supporting better coordination within the interdisciplinary team (Hobson, 2022).
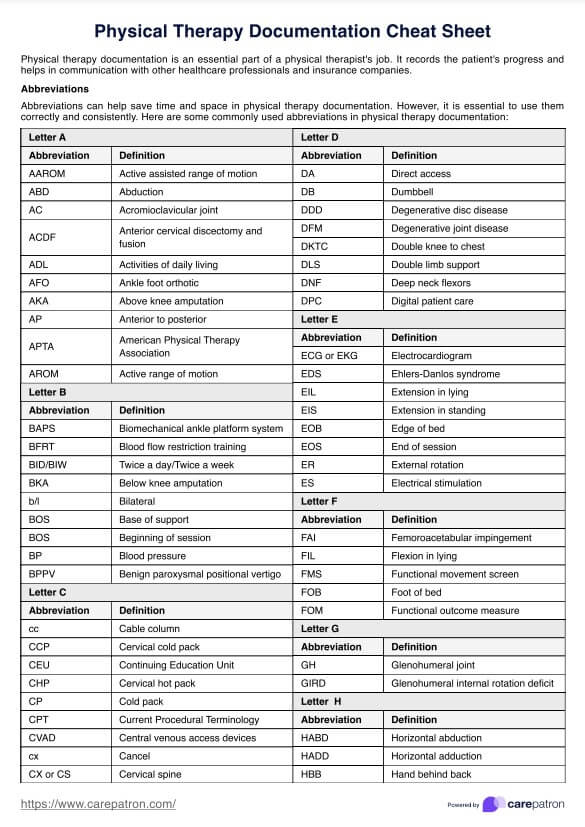
Be clear, concise, consistent, and accurate
Ensure that the documentation process uses clear, objective language, distinguishing between patient-reported statements and observed facts. Maintain consistent terminology and abbreviations. Document care activities promptly to capture accurate details and avoid jargon for better communication among healthcare providers.
Include relevant details
Document the patient's condition thoroughly, noting symptoms, responses to interventions, and any status changes. Include details on emotional and spiritual support, emphasizing the patient's preferences, goals, and how care aligns with their individualized plan.
Document collaboration and education
Document interactions and collaborations with other healthcare team members and highlight contributions from social workers, chaplains, and other team members to show a holistic approach to care.
Keep legal and ethical considerations in mind
Be aware of and adhere to legal and ethical standards in your documentation. Ensure that your documentation accurately reflects the care provided and meets regulatory requirements.
Regularly review and revise
Periodically review your documentation practices for continuous improvement. Stay updated on documentation standards or policy changes within your hospice organization.
Reference
Hobson, R. (2022, January 26). Hospice Documentation What You Need to Know. Hospice Nurse Hero. https://hospicenursehero.com/hospice-documentation/
Commonly asked questions
It serves as a legal record of the care provided and hospice eligibility, ensuring compliance with regulatory standards. Additionally, comprehensive documentation supports continuity of care by providing a clear and detailed history of the patient's condition and the interventions undertaken.
Documentation for pain management in hospice care should include the patient's self-reported pain levels, the effectiveness of prescribed medications, and any non-pharmacological interventions used.
Documenting emotional and spiritual support in hospice care involves recording interventions to address the psychosocial and spiritual aspects of the patient's well-being. This includes documenting conversations about the patient's emotional state, any counseling or therapeutic interventions provided, and support for the patient's family.