Using an Occupational Therapy (OT) Documentation Cheat Sheet streamlines the documentation process, ensures consistency and accuracy in recording patient data, saves time, and facilitates compliance with regulatory standards. It provides a structured framework for therapists to document essential information during therapy sessions.
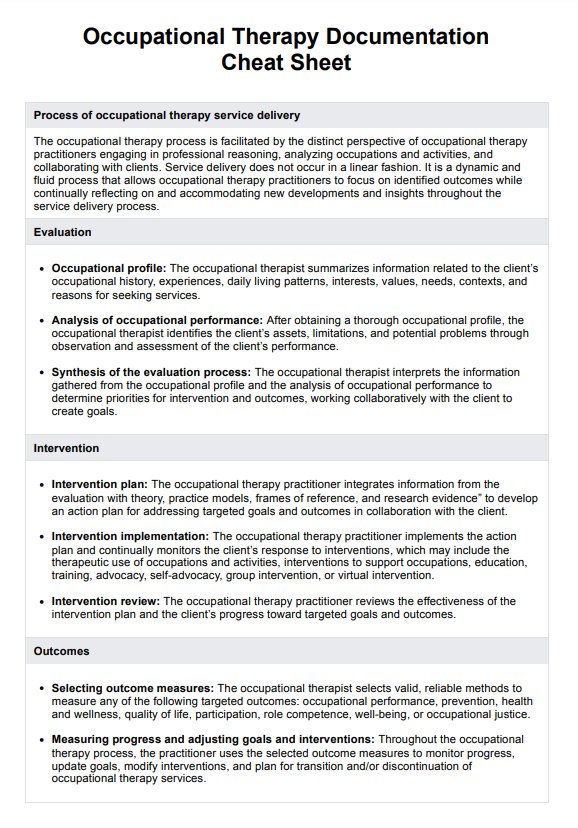
Occupational Therapy Documentation Cheat Sheet
Streamline healthcare workflows with our Occupational Therapy Documentation Cheat Sheet, ensuring accurate, efficient record-keeping for improved patient care.
Occupational Therapy Documentation Cheat Sheet Template
Commonly asked questions
An Occupational Therapy (OT) Documentation Cheat Sheet offers several benefits to therapists, including improved workflow efficiency, enhanced communication among healthcare professionals, better tracking of patient progress, reduced risk of errors or omissions, and compliance with documentation standards.
A practical Occupational Therapy (OT) Documentation Cheat Sheet should include guidelines and reference information to be used for effective OT documentation.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











