Bronchitis Treatment Guidelines
Explore bronchitis treatment guidelines for both acute and chronic forms, focusing on diagnosis, management, and preventive measures.


What is bronchitis?
Bronchitis is an inflammation of the lining of your bronchial tubes, which carry air to and from your lungs. People with bronchitis often cough up thickened mucus, which can be discolored.
Bronchitis may be either acute or chronic. An uncomplicated acute bronchitis is more common and usually caused by acute cough or viral infection, often following acute respiratory tract infections or upper respiratory tract infections. It typically improves within a week to 10 days without lasting effects, although the cough—which can be a sign of an acute respiratory illness—may linger for weeks.
Chronic bronchitis, a condition included in chronic obstructive pulmonary disease (COPD), is a long-term inflammation of the bronchi, resulting in chronic cough and sputum (mucus) production. This condition requires ongoing management and can be exacerbated by various triggers.
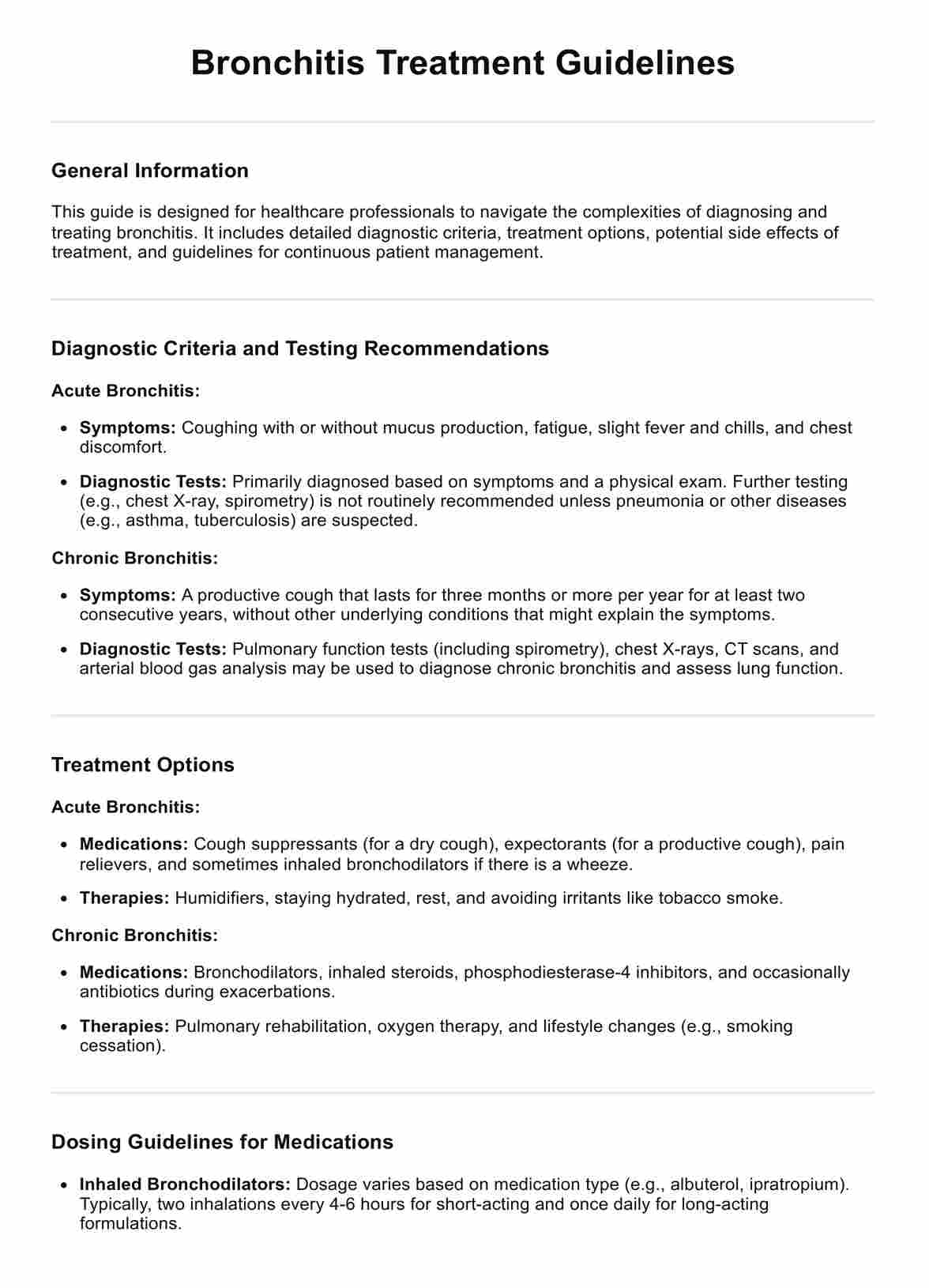
Bronchitis Treatment Guidelines Template
Bronchitis Treatment Guidelines Example
Bronchitis symptoms
The symptoms of bronchitis include:
- Persistent cough, which may produce clear, white, yellowish-gray, or green mucus (though green or yellow mucus does not necessarily mean a bacterial infection)
- Fatigue
- Shortness of breath
- Slight fever and chills
- Chest discomfort
These symptoms may last for a few weeks in patients with acute bronchitis. Still, in chronic bronchitis, they are more persistent, affecting the individual for months at a time, and often recurring over several years.
Types of bronchitis
Bronchitis can be categorized into two main types: acute and chronic. Each type has distinct characteristics, causes, and treatment approaches.
Acute bronchitis
Acute bronchitis is a shorter-term inflammation of the bronchial tubes and is often called a chest cold. It typically develops from a cold or other lower respiratory tract infection and is quite common. The main symptom is a cough, which may bring up clear, white, yellowish-gray, or green mucus. Other symptoms can include wheezing, chest tightness, and slight fever.
In most cases, acute bronchitis resolves within 10 to 14 days, although the cough may linger for several weeks afterward. Viral infections are the primary cause of acute bronchitis, but bacteria can also be a culprit in rare cases. Treatment of acute bronchitis usually focuses on symptom relief, such as increased fluid intake, rest, and, if necessary, over-the-counter cough suppressants and pain relievers.
Chronic bronchitis
Chronic bronchitis is a more serious, long-term condition characterized by persistent inflammation of the lining of the bronchial tubes, leading to a constant cough that produces mucus for at least three months in a year for two consecutive years. It is one of the conditions grouped under chronic obstructive pulmonary disease.
Chronic bronchitis develops over time, and its primary cause is long-term exposure to irritants that damage the lungs and airways, with cigarette smoke being the most common. Other irritants include air pollution, dust, and chemical fumes from the environment or workplace.
Unlike acute bronchitis, which resolves relatively quickly, chronic bronchitis requires ongoing management. Treatments aim to relieve symptoms, reduce the severity and frequency of flare-ups, and improve quality of life. This may include quitting smoking, using inhaled steroids, and taking bronchodilators to widen the airways.
How do healthcare professionals diagnose bronchitis?
Diagnosing bronchitis typically involves a combination of medical history review, physical examination, and possibly some diagnostic tests. The process aims to determine whether a patient has bronchitis, differentiate between acute and chronic bronchitis symptoms, and identify any underlying conditions or complications. Here's an overview of how healthcare professionals diagnose bronchitis:
Medical history and physical examination
In the comprehensive process of diagnosing and understanding a patient's health issues, taking a thorough medical history and performing a physical examination are pivotal first steps.
- Medical history: The healthcare provider will ask about the symptoms, their duration, and any patterns or triggers noted. Questions might also cover the patient's medical history, including any recent illnesses, smoking habits, exposure to environmental irritants, and family history of respiratory diseases.
- Physical examination: During the physical exam, the doctor listens to the patient's lungs with a stethoscope for any abnormal sounds, such as wheezing or a prolonged expiratory phase, which are common in bronchitis. The doctor may also check the throat, nasal passages, and ears, and feel the lymph nodes in the neck for swelling.
Diagnostic tests
While the diagnosis of acute bronchitis is primarily based on symptoms and physical examination, further tests may be needed to exclude other conditions, such as pneumonia, or to assess the severity of chronic bronchitis. These tests can include:
- Chest x-ray: This is used primarily to rule out pneumonia or other lung conditions.
- Pulmonary function test (PFT): For chronic bronchitis, PFTs can measure how well the lungs are working. This involves blowing into a spirometer, which measures the amount and speed of air a person can inhale and exhale. Results can help assess the extent of lung damage and determine the stage of COPD if present.
- Sputum tests: Analyzing the mucus (sputum) that's coughed up can help identify infections or the presence of allergens.
- Blood tests: Although not routinely done for bronchitis, blood tests can help identify signs of infection or inflammation and assess overall health.
More comprehensive assessments may be necessary in cases of chronic bronchitis or if COPD is suspected. This could involve detailed lung function tests, CT scans, and evaluations for oxygen therapy if low oxygen levels are a concern.
Treatment guidelines for chronic bronchitis
Managing chronic bronchitis requires a multifaceted approach, combining non-pharmacological strategies, pharmacological treatments, and patient education to alleviate symptoms, improve pulmonary function, and prevent complications.
Non-pharmacological interventions
Lifestyle changes and environmental control play a critical role in managing chronic bronchitis. Key strategies include:
- Environmental control: Minimizing exposure to tobacco smoke, pollutants, and other airborne irritants can help reduce bronchial inflammation and prevent exacerbations.
- Pulmonary rehabilitation: A program that includes patient education, exercise training, nutrition advice, and psychological support has been shown to improve the overall quality of life for patients with chronic bronchitis.
- Breathing techniques: Techniques such as pursed-lip breathing and diaphragmatic breathing can help patients manage dyspnea (shortness of breath) and increase oxygenation.
- Vaccinations: Annual influenza vaccination and pneumococcal vaccination are recommended to prevent infections that can exacerbate chronic bronchitis.
Pharmacological management
Effective pharmacological management is aimed at relieving symptoms, reducing the frequency of exacerbations, and slowing disease progression. Common medications include:
- Inhaled bronchodilators: These medications help to relax and open the airways, making breathing easier.
- Inhaled corticosteroids: These are used to reduce inflammation in the airways and can help decrease the frequency of exacerbations.
- Mucolytics: These drugs can help to thin mucus, making it easier to clear from the lungs.
- Antibiotics: Prescribed during exacerbations caused by bacterial infections, antibiotics can help to clear the infection and reduce inflammation.
- Phosphodiesterase-4 inhibitors: A newer class of medication that can decrease inflammation and relax the airways, making breathing easier for some patients with severe COPD and symptoms of chronic bronchitis.
Symptom management and supportive care
Efficient management of chronic bronchitis symptoms and providing supportive care are crucial for enhancing the patient's quality of life. Ensuring adequate hydration and using a humidifier can help thin mucus, making it easier to cough up. Energy conservation techniques and physical activity tailored to the individual’s capability are essential for maintaining muscle strength and endurance.
Monitoring and follow-up
Regular follow-up and monitoring are crucial for adjusting treatment plans as needed and for early detection of potential complications. Spirometry, a test that measures lung function, is an important tool in monitoring disease progression.
Patient and caregiver education
Education is a cornerstone of managing chronic bronchitis. Patients and caregivers should be informed about the importance of smoking cessation, adherence to prescribed treatments, and strategies for managing flare-ups. Understanding when and how to use medications, especially inhalers, is crucial for effective treatment.
How does our Bronchitis Treatment Guidelines template work?
The bronchitis treatment guidelines template is designed to streamline diagnosing, treating, and managing patients with bronchitis, providing healthcare providers with a structured format. Here's how it works:
- Distinguishing bronchitis types: The guidelines initially categorize bronchitis into acute and chronic types, providing details on their characteristics and common causes. This classification helps make accurate diagnoses and tailor treatments to the specific form of bronchitis encountered.
- Treatment options: The guidelines outline clear treatment objectives, including alleviating symptoms, enhancing function, preventing complications, and educating on self-management. These goals aim to ensure a comprehensive approach to patient care.
- Applying non-pharmacological and pharmacological treatments: It guides clinicians through various treatment options. Non-pharmacological strategies are detailed, such as environmental control, pulmonary rehabilitation, nutrition, breathing techniques, and vaccinations, complete with tips for implementation.
Pharmacological management is also extensively covered, recommending specific medications like antibiotics, bronchodilators, corticosteroids, mucolytics, and PDE4 inhibitors, each chosen to alleviate symptoms and tackle the underlying causes of bronchitis. - Ensuring ongoing monitoring and education: Emphasizing the importance of regular monitoring through activities like spirometry and staying up to date with vaccinations, the guidelines also advise on early specialist referrals for patients at risk and educate patients and caregivers about crucial aspects such as smoking cessation, proper inhaler technique, and recognizing exacerbation signs.
These guidelines offer a structured approach to bronchitis treatment, providing healthcare providers with the crucial information needed for comprehensive, evidence-based care delivery.
Common treatments for bronchitis
Bronchitis treatment aims to alleviate symptoms, improve breathing, and manage the condition effectively. The treatment approach varies between patients with acute and chronic bronchitis, focusing on symptom relief for the former and long-term management for the latter.
Antibiotic treatment
Antibiotic treatment is not standard for all bronchitis cases due to the viral nature of most acute bronchitis infections. However, antibiotics may be prescribed in certain situations:
- Bacterial infections: Antibiotics may be prescribed if the healthcare provider suspects or confirms a bacterial infection is causing or complicating the bronchitis.
- Chronic bronchitis exacerbations: People with chronic bronchitis may experience exacerbations (worsening of symptoms) due to bacterial infections, in which case antibiotics can effectively manage these episodes.
- Underlying conditions: Patients with certain risk factors or underlying conditions, such as a weakened immune system, may be more likely to receive antibiotics to prevent potential complications.
It's important for antibiotics to be used judiciously to avoid antibiotic resistance. If antibiotic therapy is prescribed, patients are advised to complete the full course of antibiotics, even if they start feeling better before finishing the medication.
Cough suppressants
Coughing is a common and often persistent symptom of bronchitis, serving the purpose of clearing mucus from the bronchial tubes. However, excessive coughing can be uncomfortable and interfere with sleep and daily activities, which is where cough suppressants can be helpful:
- OTC cough medicines: Over-the-counter cough suppressants, such as dextromethorphan, can help reduce the cough reflex and are often used for short-term relief, especially at night to improve sleep.
- Prescription cough medicine: A healthcare provider may sometimes prescribe stronger cough suppressants, particularly if the cough is severe.
- Honey: For adults and children over one-year-old, honey can be an effective natural remedy to soothe the throat and reduce the frequency of coughing.
While cough suppressants can offer relief, they are not suitable for everyone. They should be used cautiously, especially in children, and are not recommended for those with chronic bronchitis or COPD, where coughing helps clear the airways.
Commonly asked questions
While a cold primarily affects the nose and throat, bronchitis involves inflammation of the bronchial tubes in the lungs, leading to a persistent cough. Symptoms of a cold tend to be milder and resolve quicker than bronchitis.
Yes, especially in cases of acute bronchitis, if the infection spreads to the lungs, leading to pneumonia. However, this is more common among individuals with weakened immune systems, the elderly, or those with existing acute respiratory infections or conditions.
Acute bronchitis caused by viral infections can be contagious, similar to how colds and flu spread. Chronic bronchitis, linked to long-term irritation of the airways and not infections, is not contagious.