Tumor Marker Blood
Discover the significance of the Tumor Marker Blood Test, its role in cancer diagnosis, monitoring, and the latest ICD-10 codes for accurate documentation.


What is a Tumor Marker Blood Test?
Tumor Marker Blood Tests are a crucial component in oncology diagnostics. These tests specifically target and identify substances in the blood known as tumor markers. Intriguingly, these markers can originate from two primary sources: directly from the tumor itself or produced by the body as a reactive response to the presence of cancerous cells.
The primary utility of these tests lies in their ability to diagnose certain types of cancers at their nascent stages. Furthermore, they play a pivotal role in tracking the efficacy of ongoing cancer treatments, providing insights into how well a patient's body responds to therapy. Another significant application of these tests is in the surveillance of patients who have completed their treatment, as they can help in early detection of cancer recurrence.
However, while Tumor Marker Blood Tests offer a wealth of information and insights, they are not standalone diagnostic tools. Their results need to be interpreted cautiously. Factors such as non-cancerous conditions, inflammation, or other benign diseases can also lead to elevated tumor marker levels. Hence, these tests are typically used with other diagnostic procedures and imaging techniques for a comprehensive and accurate diagnosis.
Tumor Marker Blood Tests guide healthcare professionals in the intricate maze of cancer diagnosis, treatment, and post-treatment monitoring, ensuring patients receive timely and appropriate care.
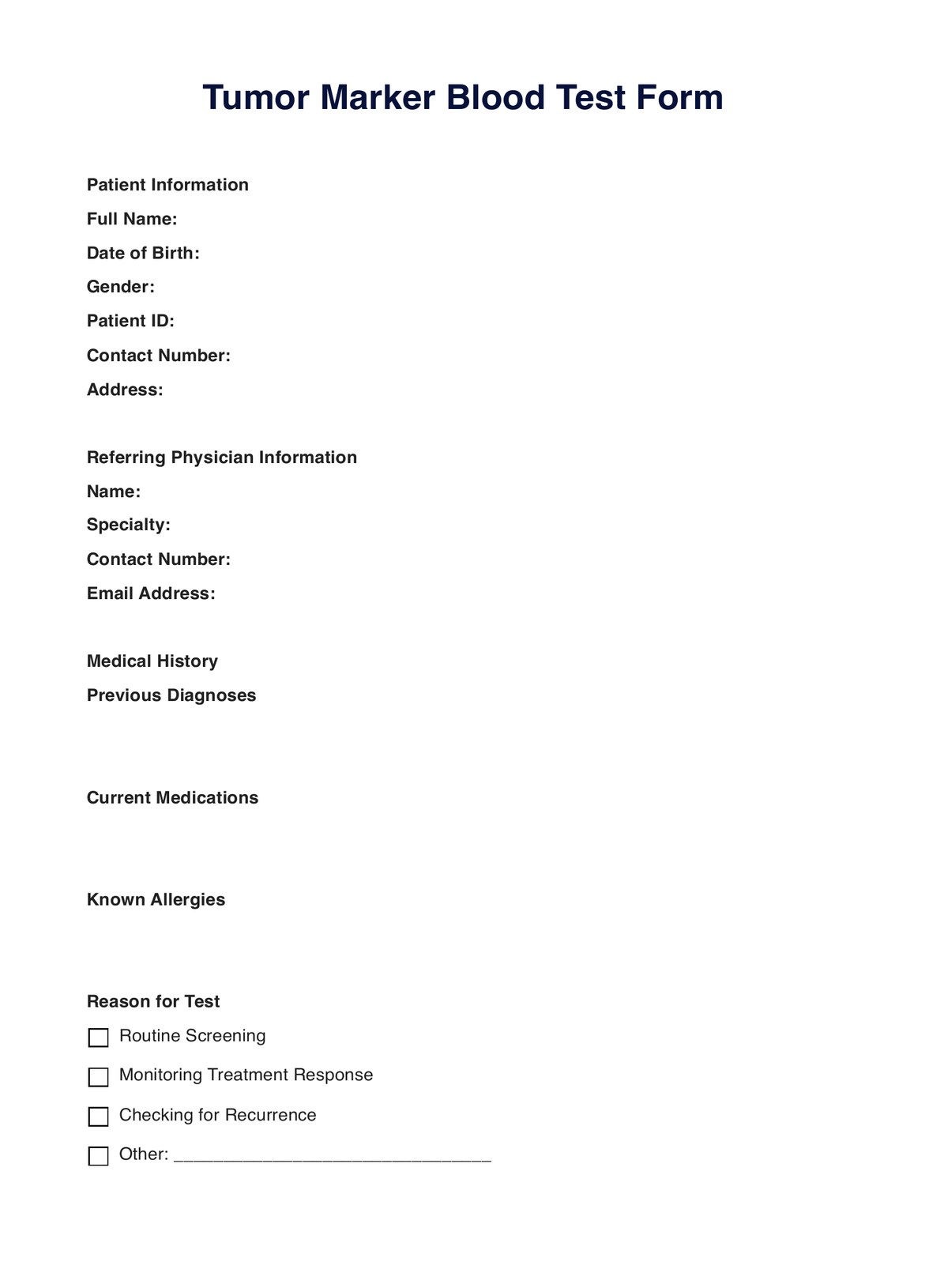
Tumor Marker Blood Template
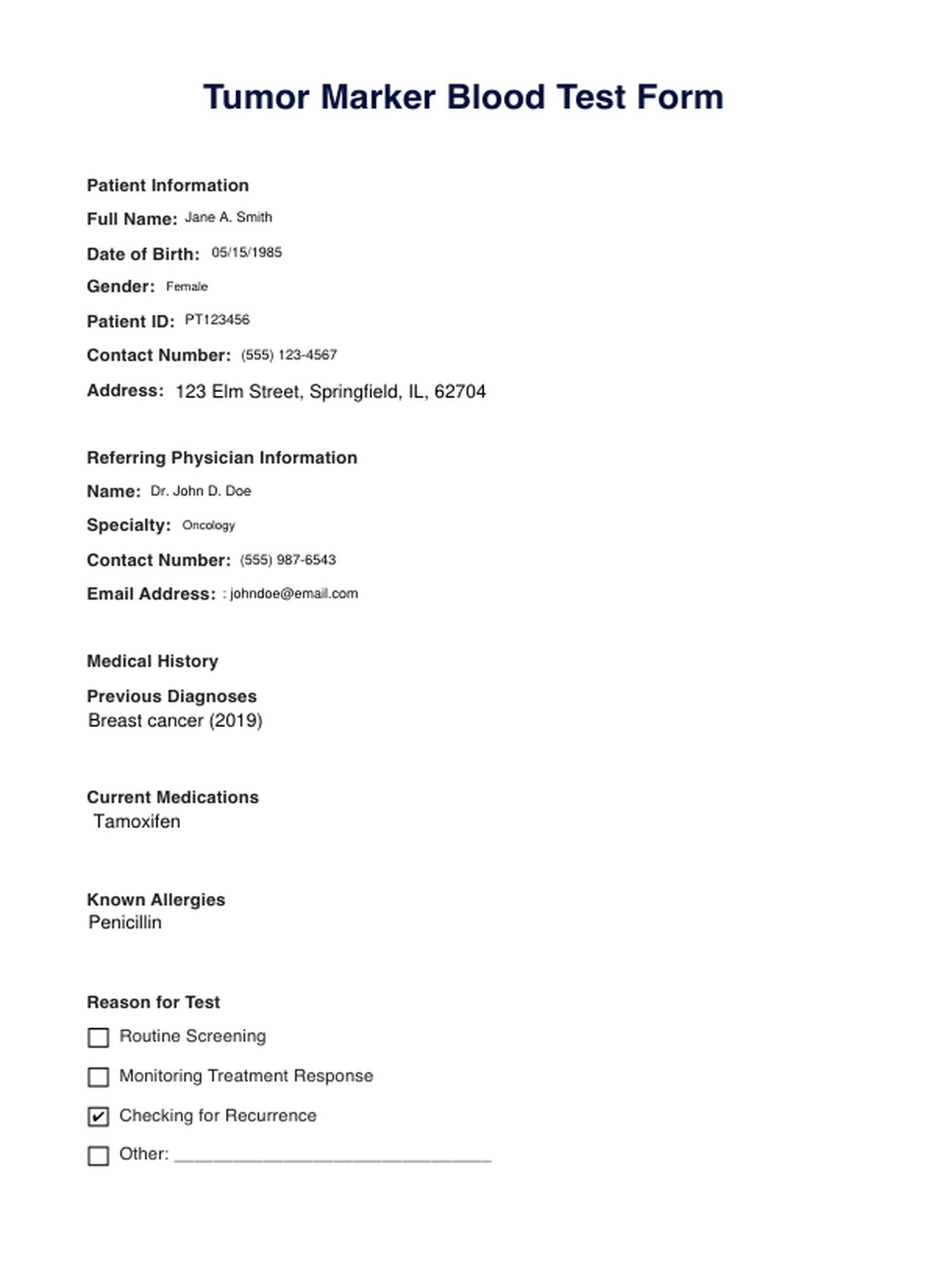
Tumor Marker Blood Example
How Does it Work?
Tumor Marker Blood Tests operate on the principle of detecting specific substances, known as tumor markers, in the bloodstream. These markers can indicate the presence of cancerous cells in the body. Here's a step-by-step breakdown of how this diagnostic procedure works:
Step 1: Understanding Tumor Markers
Tumor markers are unique substances found in or produced by cancer cells. Healthy cells can also produce them in response to malignant cells in the body. These markers can be proteins, enzymes, biochemicals, or even specific gene mutations.
Step 2: Blood Sample Collection
A healthcare professional will draw a blood sample from the patient's arm using a needle. This procedure is relatively quick and may cause mild discomfort. The collected blood is then stored in a sterile vial or tube.
Step 3: Laboratory Analysis
The blood sample is sent to a specialized laboratory for analysis. Advanced equipment and techniques are used to measure the levels of specific tumor markers in the blood. The results are then compared to reference ranges to determine if they are within normal limits.
Step 4: Interpreting the Results
Elevated levels of tumor markers might suggest the presence of cancer. However, it's crucial to note that tumor markers are not definitive. Other non-cancerous conditions, such as inflammation, liver disease, or benign tumors, can also lead to elevated tumor marker levels. Therefore, results from Tumor Marker Blood Tests are typically used with other diagnostic tools for a more comprehensive understanding.
Step 5: Follow-up and Further Testing
Further diagnostic tests, such as imaging scans or biopsies, might be recommended if the test results indicate elevated tumor marker levels. Regular monitoring might be required to track changes in tumor marker levels over time, especially during cancer treatment or post-treatment surveillance.
While our printable Tumor Marker Blood Tests provide valuable insights into the potential presence of cancer, they are just one piece of the diagnostic puzzle. A holistic approach, considering the patient's overall health, symptoms, and other test results, is essential for accurate diagnosis and treatment.
When Would you use this Test?
Tumor Marker Blood Tests have become an integral tool in oncology, aiding healthcare professionals in various aspects of cancer care. Their versatility and specificity make them invaluable in several clinical scenarios:
- Diagnosis: While these tests alone cannot confirm the presence of cancer, elevated levels of certain tumor markers can indicate specific types of cancers. For instance, elevated levels of CA-125 might suggest ovarian cancer, while high PSA levels could indicate prostate cancer.
- Treatment Monitoring: Once a cancer diagnosis is confirmed, Tumor Marker Blood Tests can be used to monitor the effectiveness of the treatment. A decrease in the tumor marker level might indicate that the treatment is working, while an increase could suggest the need for a different therapeutic approach.
- Recurrence Surveillance: For patients who have undergone treatment and are in remission, these tests can be periodically conducted to check for cancer recurrence. Any unexpected rise in tumor marker levels might warrant further investigations.
- High-Risk Screening: Individuals with a family history of certain cancers or those with known genetic mutations that increase cancer risk might undergo routine Tumor Marker Blood Tests. This proactive approach helps in early detection, significantly improving treatment outcomes.
- Guiding Treatment Choices: In some cases, the type and level of tumor markers can guide oncologists in choosing the most appropriate treatment modality. For example, certain breast cancers that express high levels of HER2 protein might respond better to treatments targeting HER2.
It's essential to note that while Tumor Marker Blood Tests provide valuable insights, they should be interpreted in conjunction with other diagnostic tools and clinical findings. A comprehensive approach ensures accurate diagnosis and optimal patient care.
For more details on when and how to use this test, refer to our Tumor Marker Blood Test resource, which offers a deeper dive into its applications and benefits.
What do the Results Mean?
The Tumor Marker Blood Test results provide a snapshot of specific substances or markers in the blood that might be associated with cancer. However, interpreting these results is not always straightforward. Here's a deeper look into what these results might signify:
Elevated Levels
An increased level of a tumor marker might suggest the presence of a particular type of cancer. For instance, high levels of CEA might be associated with colorectal cancer, while elevated CA-125 levels could indicate ovarian cancer. However, it's crucial to understand that elevated levels don't confirm cancer. Various benign conditions, such as inflammation, infections, or even certain habits like smoking, can also lead to increased marker levels.
Normal Levels
A normal result can be reassuring but doesn't entirely rule out cancer. Some cancers might not produce elevated levels of tumor markers, especially in the early stages.
Decreasing Levels
If a patient is undergoing cancer treatment and the levels of the tumor marker decrease, it often indicates that the treatment is effective and the cancer is responding to it.
Increasing Levels
On the other hand, if the marker levels rise during treatment, it might suggest that the cancer is not responding to the treatment, or there could be a recurrence.
Stable Levels
Sometimes, the levels might remain stable, neither increasing nor decreasing significantly. In such cases, it might indicate that the cancer is stable.
Considering Tumor Marker Blood Test results as just one piece of the diagnostic puzzle is imperative. They should be combined with other tests, clinical examinations, and patient history for a comprehensive understanding. Moreover, slight variations in test results can occur due to differences in laboratory techniques, so it's always recommended to have the test done at the same lab if monitoring over time.
Always consult with a healthcare provider for a more detailed understanding of your results and what they might mean for your health. They can provide insights tailored to your situation and guide you on the next steps. For more information, refer to our Free Tumor Marker Blood Test resource.
Research & Evidence
Tumor Marker Blood Tests have a rich history in oncology and have played a pivotal role in advancing our understanding and management of cancer. The inception of these tests dates back to the mid-20th century when scientists began to identify specific proteins associated with tumors. Over the decades, as our understanding of cancer biology expanded, so did the list of detectable tumor markers.
Several landmark studies have underscored the importance of Tumor Marker Blood Tests. For instance, research has shown that markers such as PSA (Prostate-Specific Antigen) can be instrumental in detecting prostate cancer at an early stage, leading to better patient outcomes. Similarly, the CA-125 marker has been extensively studied for its role in diagnosing and monitoring ovarian cancer.
However, while these tests have proven invaluable in many scenarios, they have limitations. Some studies have pointed out that relying solely on tumor markers can lead to false positives, where elevated levels are detected in the absence of cancer. This has led to an emphasis on using Tumor Marker Blood Tests with other diagnostic tools, such as imaging and biopsies, to ensure accurate diagnosis and monitoring.
Furthermore, ongoing research continues to explore the potential of newer tumor markers and their role in predicting cancer prognosis, guiding treatment decisions, and monitoring disease progression. The evolution of personalized medicine, where treatments are tailored based on individual patient profiles, has further highlighted the significance of these tests.
While Tumor Marker Blood Tests have provided invaluable insights into cancer diagnosis and management, they are most effective when interpreted in the broader context of a patient's clinical picture. As research continues, it is anticipated that these tests will become even more refined, enhancing their utility in the ever-evolving field of oncology.
References
- Smith, A. J., & Paulson, E. K. (1998). Tumor markers in oncology: their role and relevance. Journal of Clinical Oncology, 16(2), 549-557.
- O'Brien, M. E., & Borthwick, A. (2006). The role of CA-125 in clinical practice. Journal of Clinical Pathology, 59(3), 232-236.
- Thompson, I. M., Pauler, D. K., & Goodman, P. J. (2004). Prevalence of prostate cancer among men with a prostate-specific antigen level ≤4.0 ng per milliliter. The New England Journal of Medicine, 350(22), 2239-2246.
Commonly asked questions
Oncologists, general practitioners, or specialists might request this Tumor Marker Blood Test.
Tumor Marker Blood Tests are used for diagnosing, monitoring treatment, and checking for recurrence of certain cancers.
Tumor Marker Blood Tests are used to measure the levels of specific substances in the blood that might indicate the presence of cancer.

.jpg)