To write a treatment plan summary, begin by clearly stating the patient's diagnosis and the goals of the treatment plan. Include a brief overview of the interventions implemented, the patient's progress toward the goals, and any modifications made to the original plan. Summarize the outcomes observed, such as improvements in symptoms or functionality, and conclude with recommendations for ongoing care or follow-up.
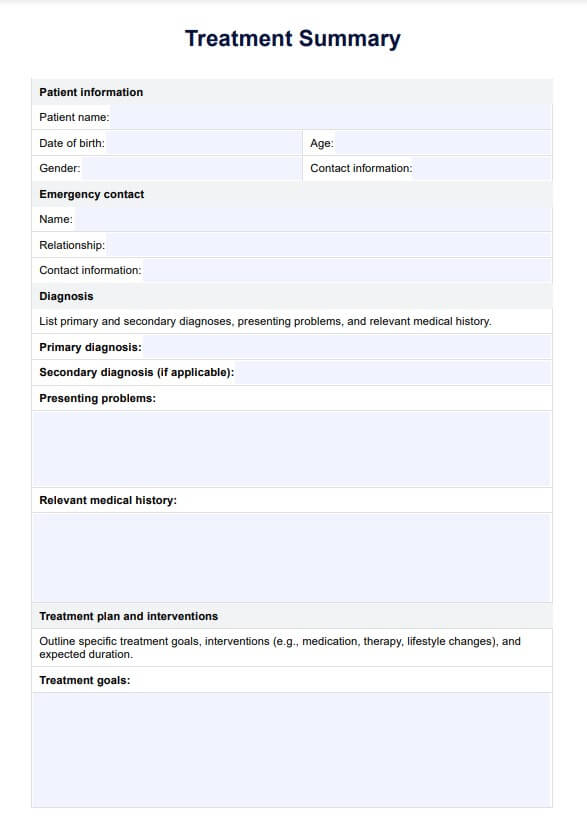
Treatment Summary Template
Unlock effective mental health documentation with our Treatment Summary Template guide – streamline progress tracking and enhance client care.
Treatment Summary Template Template
Commonly asked questions
The end-of-treatment summary is a comprehensive document that outlines the patient's progress and outcomes at the conclusion of a treatment program. It typically includes a review of the initial diagnosis, the treatment goals established, the interventions used, and the patient's response to those interventions.
To write a treatment summary for therapy, start by documenting the patient's presenting issues and the therapeutic goals established at the beginning of treatment. Include a detailed account of the therapeutic interventions used, such as specific techniques or modalities, and note the patient's engagement and progress throughout the sessions. Conclude with recommendations for ongoing support, future therapy sessions, or self-care strategies.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











