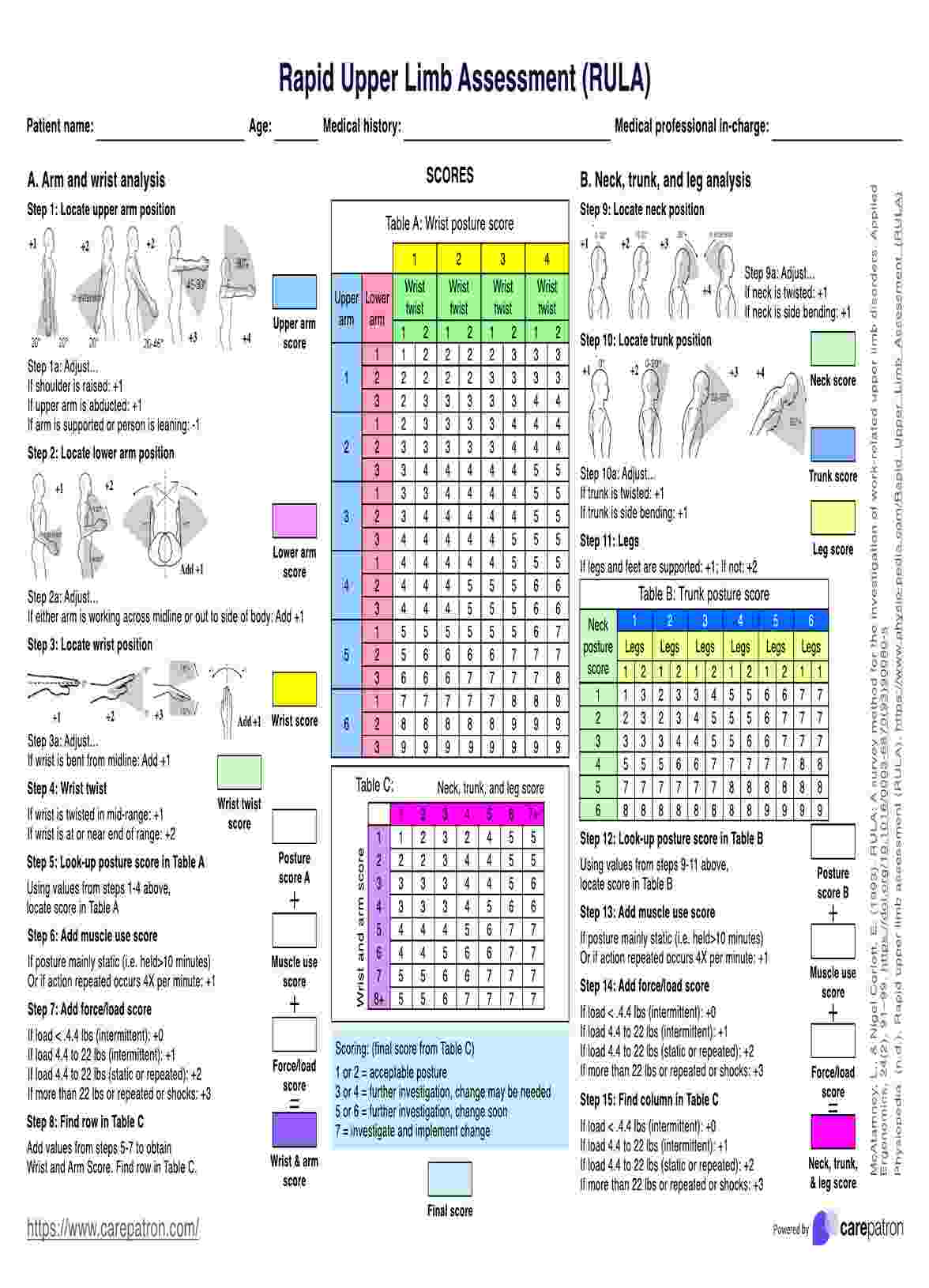
The Rapid Upper Limb Assessment (RULA) is an ergonomic tool used to evaluate and assess the risk of musculoskeletal disorders associated with upper limb tasks in the workplace.
Rapid Upper Limb Assessment
Learn about Rapid Upper Limb Assessment with examples on our site. Get Carepatron's free PDF download today!
Rapid Upper Limb Assessment Template
Commonly asked questions
To perform a Rapid Upper Limb Assessment (RULA), observe the worker's posture, movements, and equipment usage during the task, assign scores based on predefined criteria for various postures, and calculate the total RULA score to determine the ergonomic risk level.
While both Rapid Upper Limb Assessment (RULA) and Rapid Entire Body Assessment (REBA) are ergonomic assessment tools used to evaluate musculoskeletal risks, RULA focuses specifically on upper limb tasks. At the same time, REBA assesses the entire body posture during various tasks.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











