The first line of treatment for PVD typically involves healthy lifestyle changes, such as quitting smoking, exercising, and adopting a more nutritious diet.
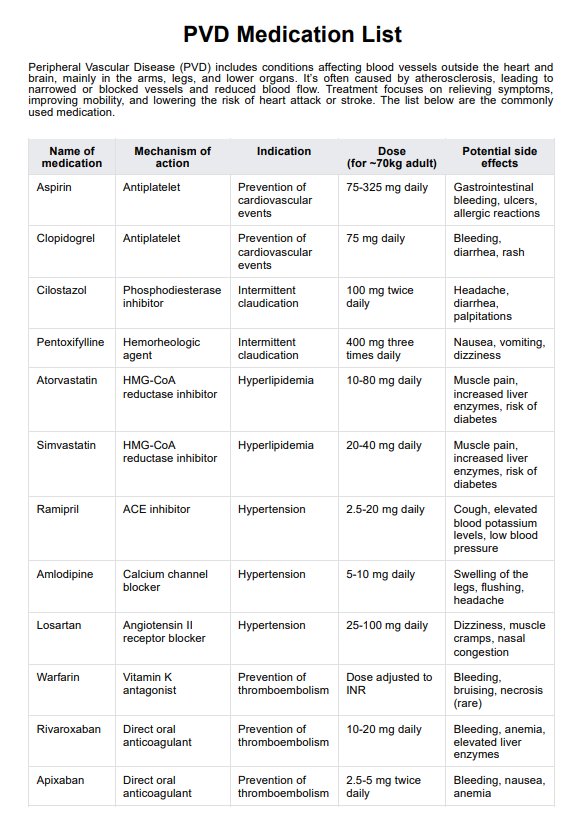
PVD Medication List
Use our PVD Medication List to refresh yourself on the various PVD medications you can provide or prescribe to patients with peripheral vascular disease.
Use Template
PVD Medication List Template
Commonly asked questions
Cilostazol is often the drug of choice for improving symptoms of claudication in peripheral artery disease (PAD) unless contraindicated.
Peripheral artery disease and coronary artery disease are similar because both are the result of atherosclerosis; however, the difference is, the former affects the peripheral blood vessels, and the latter affects the coronary arteries.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











