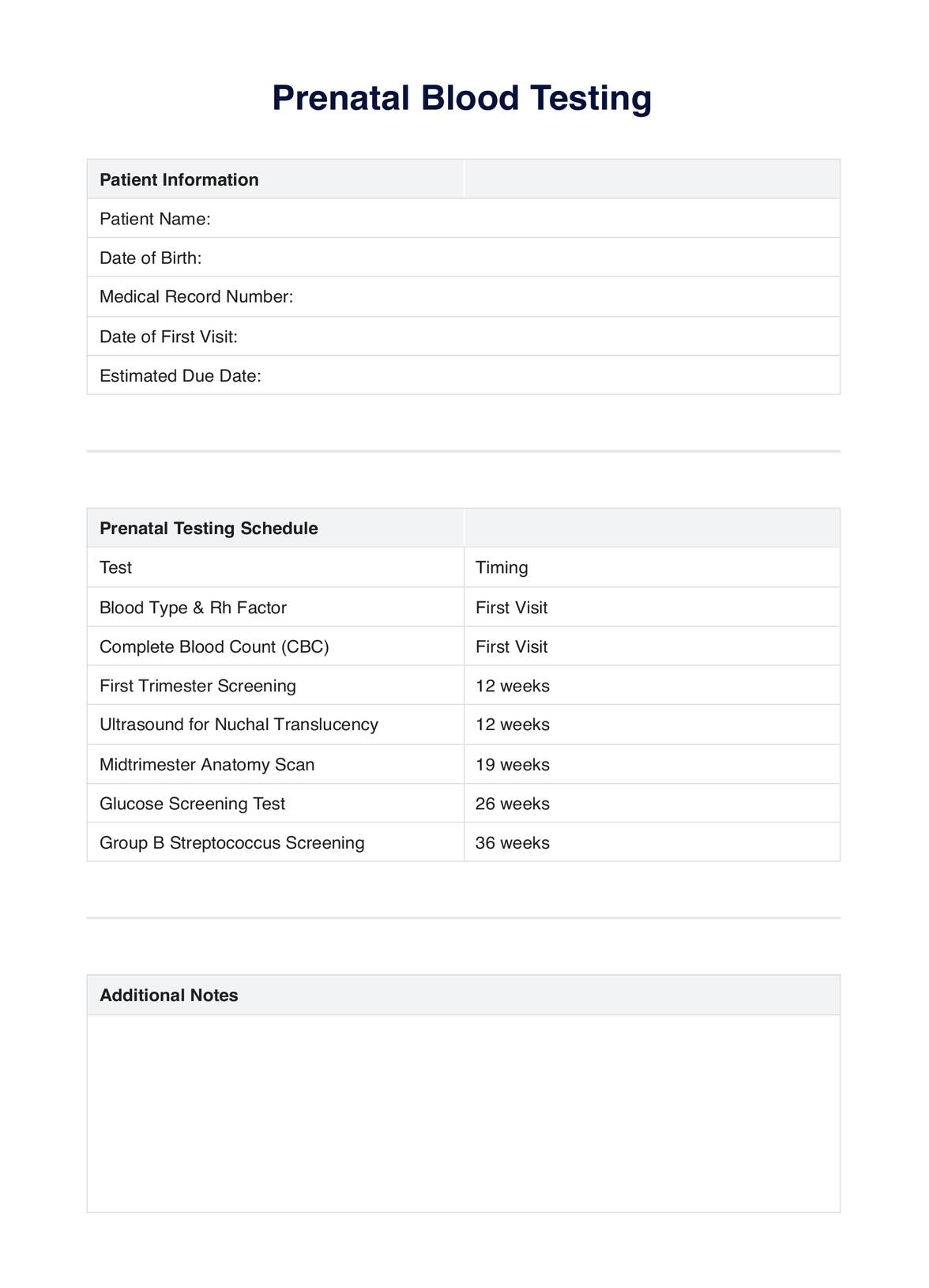
Prenatal blood testing is a series of blood tests conducted during pregnancy to assess the health of both the mother and the fetus. These tests can detect genetic conditions and potential issues, ensuring timely interventions.
Explore our comprehensive guide on prenatal blood tests and ultrasounds, offering vital insights for healthcare professionals. Download our free PDF now!
Prenatal blood testing is a series of blood tests conducted during pregnancy to assess the health of both the mother and the fetus. These tests can detect genetic conditions and potential issues, ensuring timely interventions.
The first ultrasound in pregnancy is typically performed between 6 to 12 weeks. This early scan is crucial for confirming the pregnancy, estimating the due date, and checking for multiple pregnancies.
Prenatal ultrasounds are generally considered safe and non-invasive. They use sound waves to create images of the fetus and do not involve radiation. However, it's essential to use them judiciously and under the guidance of a healthcare professional.
EHR and practice management software
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments