Pelvic Binding Treatment Plan
Learn about Pelvic Binding treatment plans and download Carepatron's free PDF example to help you understand the process and treatment options available.


What is a pelvic fracture?
A pelvic fracture is a break in one or more of the bones comprising the pelvis, a complex structure that includes the sacrum, coccyx, and hip bones. Pelvic fractures often result from high-energy trauma, such as car accidents or falls from significant heights, making them common among trauma patients. These fractures can vary in severity from stable pelvic fractures, which are typically isolated and involve minimal displacement, to unstable pelvic fractures that disrupt the pelvic ring and pose significant risk to internal organs and blood vessels.
Pelvic injuries can lead to complications due to the rich vascular supply and proximity to major organs, making immediate and accurate diagnosis crucial. Unstable pelvic fractures are particularly concerning as they can cause significant internal bleeding and require urgent medical intervention. Pelvic ring fractures, involving multiple breaks in the pelvic ring, often necessitate the use of a pelvic binder to stabilize the injury and reduce hemorrhage during transport and initial treatment.
The use of pelvic binders, which are devices applied externally to compress and stabilize the pelvis, is a critical initial step in managing severe pelvic fractures. Proper application of a pelvic binder can significantly improve outcomes for trauma patients by minimizing further injury and controlling bleeding. Understanding the various pelvic fracture patterns and the appropriate use of pelvic binders is essential for effective treatment and recovery.
Pelvic Binding Treatment Plan Template
Pelvic Binding Treatment Plan Example
Common types of pelvic fractures
Pelvic fractures can be classified into several types, each with distinct characteristics and treatment considerations. Understanding these common types helps in recognizing the severity of pelvic injuries and the appropriate interventions, such as the use of a pelvic binder or other pelvic compression devices. Here, we explore the most frequently encountered pelvic fractures:
Stable pelvic fractures
Stable pelvic fractures involve a single break in the pelvic ring, typically without significant displacement of the bones. These fractures often result from low-energy trauma, such as minor falls, and generally do not pose a high risk for life-threatening injuries. Patients with stable fractures may experience discomfort and limited mobility, but the overall pelvic volume remains intact. Early application of a pelvic binder can provide support and reduce pain during the initial stages of recovery.
Unstable pelvic fractures
An unstable pelvic fracture are characterized by multiple breaks or a severe break that leads to pelvic ring disruption. These fractures often result from high-energy impacts, such as car accidents or falls from great heights, and are considered traumatic pelvic injuries. Unstable fractures can significantly increase pelvic volume, leading to massive hemorrhage and posing a threat to internal organs. In such cases, the early use of a pelvic binder is crucial to stabilize the pelvis, control bleeding, and improve patient outcomes.
Acetabular fractures
Acetabular fractures occur when the socket of the hip joint (acetabulum) is broken. These fractures often accompany other pelvic injuries and can significantly impact hip stability and function. They usually result from direct trauma to the hip area. Acetabular fractures may require surgical intervention and prolonged rehabilitation.
Open pelvic fractures
Open pelvic fractures are severe injuries where the broken bones puncture the skin, creating an open wound. These fractures are often associated with high-energy trauma and carry a high risk of infection and significant bleeding. Open pelvic fractures require immediate medical attention, including the use of pelvic compression devices to manage hemorrhage and stabilize the patient for transport to a surgical facility.
Lateral compression fractures
Lateral compression fractures occur when the pelvis is compressed from the side, often during vehicular accidents. Depending on the extent of the pelvic ring disruption, these fractures can range from stable to unstable. A pelvic binder can help stabilize these fractures and control bleeding, reducing the risk of complications.
Vertical shear fractures
Vertical shear fractures are caused by forces that drive one side of the pelvis upwards, such as a fall from a height. These fractures are highly unstable and often associated with significant blood loss and internal injuries. Immediate early pelvic binder use is critical to manage and prepare the patient for further surgical intervention.
Pelvic ring injuries
A pelvic ring injury involves multiple fractures or disruptions to the pelvic ring, which consists of the sacrum, coccyx, and hip bones. Such injuries are also caused by high-energy trauma and are associated with a high risk of hemorrhage and damage to internal organs. Proper stabilization of the pelvic ring is crucial for the effective treatment and recovery of patients with these types of pelvic fractures.
What are the symptoms of a broken pelvis?
Recognizing the symptoms of a broken pelvis is crucial for timely and effective treatment. Identifying these signs can prompt early pelvic stabilization, vital for preventing further complications. Here are five common symptoms of a broken pelvis:
Severe pain
Severe pain in the pelvic region, hips, or lower back is a primary symptom of a broken pelvis. This pain can be exacerbated by movement and is often intense enough to impede walking or standing. Immediate assessment, including pelvic radiographs, is essential to diagnose the injury and avoid suboptimal pelvic binder placement.
Swelling and bruising
Swelling and bruising around the pelvic area are common symptoms due to internal bleeding and tissue damage. These signs indicate significant trauma and may accompany other injuries. Early application of a pelvic binder can help manage swelling and improve hemodynamic stability.
Difficulty moving or bearing weight
Patients with a broken pelvis often experience difficulty moving their legs or bearing weight. This is due to the instability and pain caused by the fracture. Advanced trauma life support protocols recommend immobilization and stabilizing the pelvic early to prevent further injury.
Numbness or tingling
Numbness or tingling in the groin or legs can occur if nerve damage accompanies the fracture. This symptom is particularly concerning and warrants immediate medical attention to assess and mitigate potential long-term damage.
Signs of shock
Signs of shock, such as rapid pulse, low blood pressure, and pale, clammy skin, indicate severe blood loss and are common in an unstable fracture. These symptoms necessitate urgent intervention, including the use of a pelvic binder and other measures to stabilize the patient.
Types of treatments for pelvic injuries
Treating pelvic injuries involves a combination of immediate interventions and long-term management strategies. Here are the primary types of treatments used for pelvic injuries:
Pelvic binder application
A pelvic binder is an essential tool in the initial management of pelvic injuries, particularly for unstable fractures. It helps stabilize the pelvis, reduce bleeding, and maintain hemodynamic stability. Proper placement is critical to avoid complications from suboptimal binder application and ensure effective early stabilization.
Surgical intervention
Surgery is often required for severe pelvic fractures, especially those involving significant displacement or open fractures. Surgical procedures may include internal fixation, where metal plates and screws are used to realign and stabilize the bones. This approach is crucial for restoring the integrity of the pelvic ring and promoting healing.
Pain management
Effective pain management is essential for patients with pelvic injuries. This can include the use of medications such as opioids, nonsteroidal anti-inflammatory drugs (NSAIDs), and regional anesthesia. Adequate pain control facilitates patient comfort and aids in the early stages of rehabilitation.
Physical therapy
Physical therapy plays a vital role in the recovery process following a pelvic injury. A tailored rehabilitation program helps restore mobility, strength, and function. Physical therapists work with patients to perform exercises that improve flexibility and reduce the risk of long-term complications.
Blood transfusion and fluid management
Severe pelvic injuries often result in significant blood loss. Blood transfusions and fluid resuscitation are critical to maintaining hemodynamic stability. These interventions are typically part of advanced trauma life support protocols and are administered as part of emergency care to stabilize trauma patients.
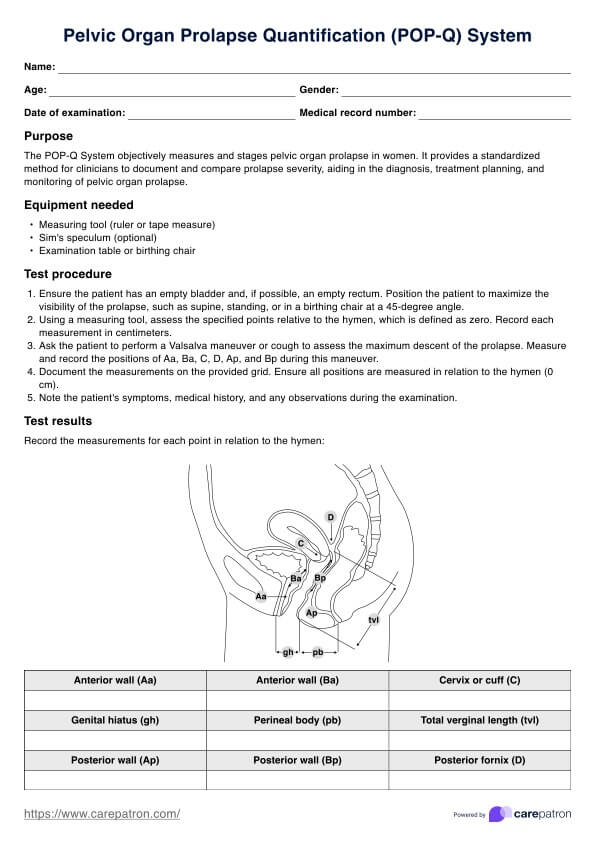
What are pelvic binders used for?
Pelvic binders stabilize pelvic fractures, particularly in unstable fractures or pelvic ring disruptions. They provide external compression to the pelvis, reducing bleeding and preventing further bone displacement.
Moreover, pelvic binders are crucial in the initial management of pelvic injuries, helping to maintain hemodynamic stability and improve patient outcomes. Proper application of a pelvic binder is essential for minimizing complications and supporting the patient during transportation and treatment.
How to use our Pelvic Binding Treatment Plan
Like any treatment plan templates that increase the accuracy and efficacy of treatments, Pelvic Binding Treatment Plan is designed to streamline the management of pelvic injuries for healthcare practitioners. Follow these steps to utilize the Carepatron's Pelvic Binding Treatment Plan effectively:
Step 1: Access the treatment plan template
Access the Pelvic Binding Treatment Plan template in Carepatron's resource library. This template is designed to guide you through the key components of pelvic injury management, from initial assessment to long-term care.
Step 2: Complete patient information
The designated sections of the treatment plan template should contain the patient's information, including demographic details, medical history, and injury specifics.
Step 3: Assessment and diagnosis
Once you have the template, assess the patient's condition according to the template instructions. This includes conducting a thorough physical examination and obtaining relevant imaging studies, such as pelvic radiographs, to confirm the diagnosis.
Step 4: Determine treatment approach
Based on the assessment findings, determine the appropriate treatment approach for the patient. This may include the application of a pelvic binder, surgical intervention, pain management, and other supportive measures as needed.
Step 5: Document treatment interventions
Document the treatment interventions implemented for the patient, including the application of the pelvic binder, surgical procedures performed, medications administered, and any other relevant interventions.
Step 6: Monitor patient progress
Monitor the patient's progress and response to treatment regularly. Document any patient condition changes, including improvements or complications, and adjust the treatment plan accordingly.
Step 7: Collaborate with multidisciplinary team
Collaborate with a multidisciplinary team, including surgeons, nurses, physical therapists, and other healthcare professionals, to ensure comprehensive care for the patient throughout their recovery journey.
Benefits of using this template for patients with pelvic fractures
Utilizing our Pelvic Binding Treatment Plan template offers several advantages for pelvic fractured patients:
Streamlined care coordination
The template facilitates clear communication and coordination among healthcare providers involved in the patient's care, ensuring that all team members are on the same page regarding treatment plans and goals.
Comprehensive documentation
By documenting all aspects of the patient's treatment and progress in one centralized template, healthcare providers can ensure comprehensive and accurate documentation, which is essential for continuity of care and future reference.
Standardized approach to treatment
The template provides a standardized approach to managing pelvic fractures, ensuring that all patients receive consistent and evidence-based care regardless of the healthcare provider or setting.
Enhanced patient safety
Healthcare providers can minimize the risk of errors and complications through the structured treatment plan outlined in the template, ultimately enhancing patient safety and reducing adverse outcomes.
Improved patient outcomes
By facilitating timely and appropriate interventions, monitoring patient progress, and promoting interdisciplinary collaboration, the template ultimately contributes to improved patient outcomes and a smoother recovery journey for fractured patients.
Commonly asked questions
A pelvic binder stabilizes pelvic fractures by compressing the pelvis, reducing bleeding, and preventing further displacement of the bones.
When applying a pelvic binder, ensure proper placement around the pelvis at the level of the greater trochanters, tighten evenly, and reassess for any complications.
Pelvic binders are typically single-use devices that maintain sterility and effectiveness. They should be disposed of after use according to medical waste disposal guidelines.