PAD Test
Discover how to conduct a Peripheral Artery Disease (PAD) Test with our comprehensive guide and template. Ensure accurate medical assessments efficiently.


What is peripheral artery disease?
Peripheral artery disease (PAD), also known as peripheral arterial disease, is characterized by poor blood flow in the arteries of the lower limbs due to plaque buildup, which narrows and blocks the blood vessels.
This reduced blood flow can lead to various symptoms, including leg pain, particularly during physical activity (intermittent claudication), and shiny skin on the legs and feet. PAD shares risk factors with coronary artery disease, including high blood pressure, high cholesterol, diabetes, and smoking. Additionally, factors such as a family history of vascular or heart disease either, older age, and unhealthy lifestyle habits increase the risk of developing PAD.
Diagnosing PAD involves a combination of a medical history review, a physical exam or examination, and specific tests. One such test is the ankle-brachial index (ABI) test, which compares the blood pressure in the ankle with that in the arm to assess blood flow in the lower limbs. Other diagnostic tests may include Doppler ultrasound, magnetic resonance angiography (MRA), and blood tests to check for markers of inflammation and blood clotting.
Early detection of PAD is crucial for preventing complications such as cardiovascular events and limb amputation. Once diagnosed, treatment aims to manage symptoms, improve blood flow, and reduce the risk of complications.
This may involve lifestyle changes such as adopting a healthy diet low in saturated fats, regular physical activity, exercise training, and supervised exercise programs tailored to improve walking distance and cardiovascular health. Medications may sometimes be prescribed to lower blood pressure and cholesterol or prevent blood clot formation.
For severe cases of PAD, procedures such as angioplasty (to widen narrowed arteries) or bypass surgery (to reroute blood flow around blocked arteries) may be necessary. However, these interventions are typically reserved for individuals with significant symptoms or those at high risk of limb loss.
PAD symptoms and signs
Peripheral artery disease (PAD) is a peripheral vascular disease that manifests through various symptoms and signs, primarily affecting the lower limbs. Here are the key symptoms and signs associated with PAD:
Pain
Pain symptoms associated with peripheral artery disease (PAD) typically manifest as intermittent claudication, causing discomfort, cramping, or pain in the legs during physical activity. This pain subsides with rest but reoccurs upon resuming activity. Additionally, individuals may experience persistent leg pain, especially during exercise, significantly impacting mobility and daily activities.
Sensory
Sensory symptoms of PAD involve sensations of numbness or weakness in the legs and feet, particularly during physical exertion. These sensations may affect mobility and contribute to difficulties in walking or performing routine tasks.
Skin changes
Skin changes associated with PAD include skin texture, temperature, and coloration alterations. Reduced blood flow to the legs and feet can result in a shiny or smooth skin appearance and decreased hair growth. Additionally, affected limbs may feel colder to the touch due to inadequate circulation, and the skin may exhibit a pale or bluish hue, indicating reduced oxygen supply.
Physical examination findings
During a physical examination, healthcare providers may detect signs of PAD, such as weak or absent pulses in the affected limbs. The absence or diminishment of pulses indicates reduced blood flow to these areas, highlighting the vascular compromise associated with PAD. Identifying such signs is crucial for accurately diagnosing and appropriately managing the condition.
Wound healing
Impaired wound healing is a common sign of advanced PAD, as compromised blood flow hinders the body's ability to repair damaged tissue effectively. Slow-healing or non-healing wounds, particularly on the legs and feet, may develop into ulcers or sores. Monitoring wound healing and promptly addressing any delays or complications is essential for preventing infections and reducing the risk of further complications.
Advanced signs
In advanced stages of PAD, individuals may experience rest pain, characterized by discomfort in the feet or toes, even during periods of rest. This persistent pain can disrupt sleep patterns and significantly impact quality of life. Furthermore, the development of gangrene, resulting from tissue death due to severe ischemia, poses a serious threat to limb viability and necessitates urgent medical attention. Identifying these advanced symptoms is critical for timely intervention and prevention of limb loss.
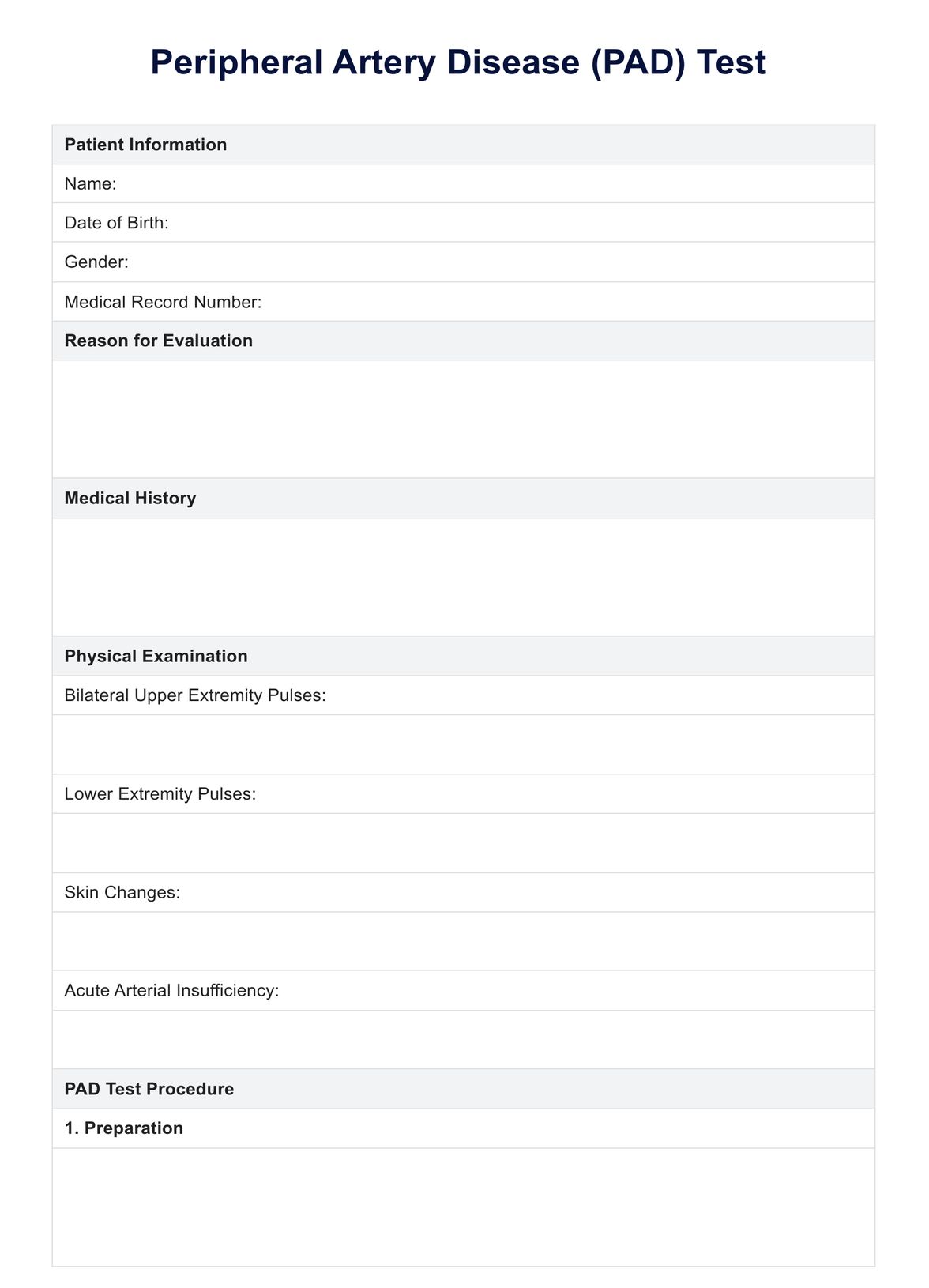
PAD Test Template
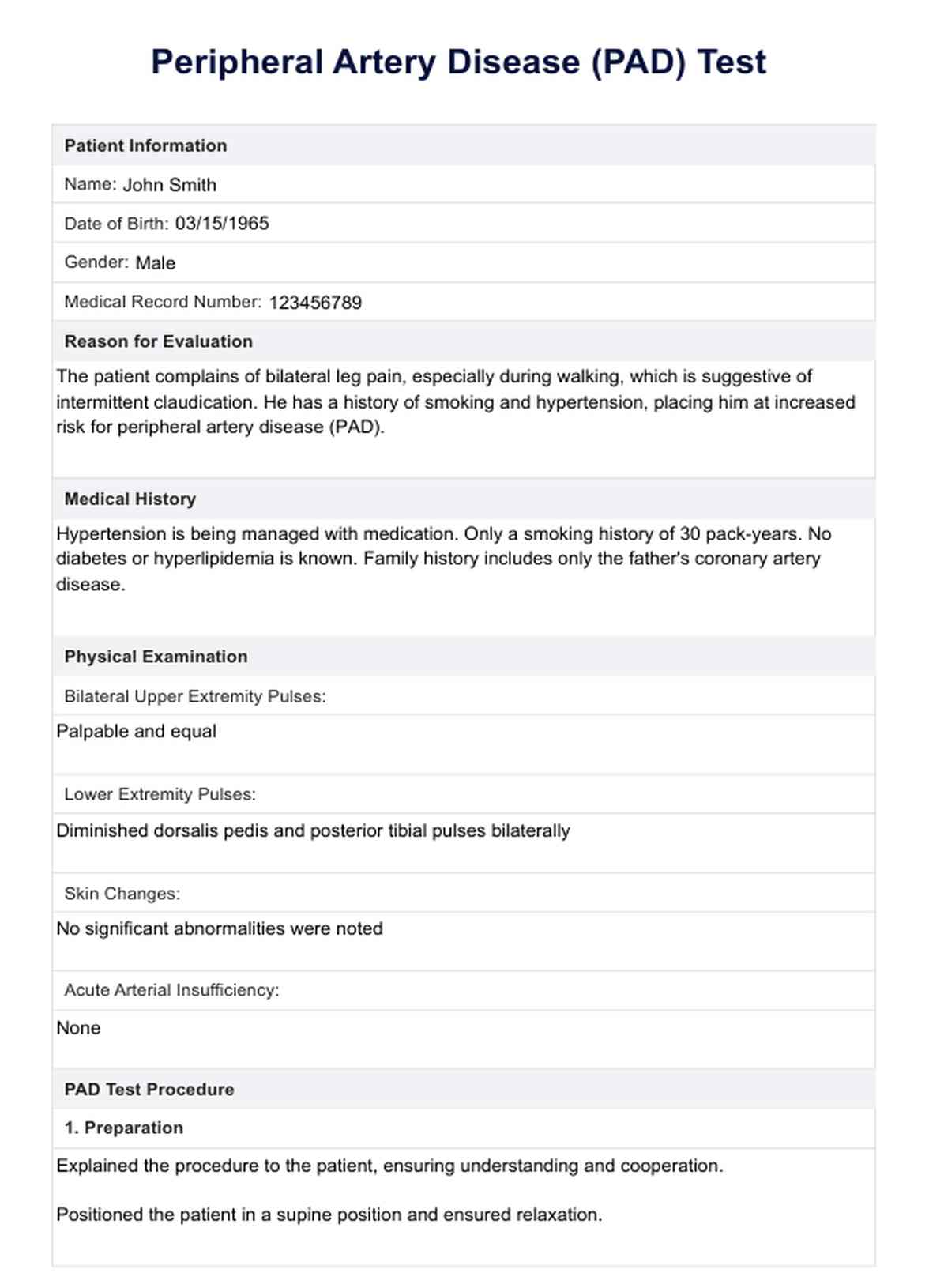
PAD Test Example
PAD risk factors
Peripheral artery disease (PAD) shares several risk factors with other cardiovascular conditions. Here are the key risk factors associated with PAD:
Behavioral and lifestyle
Unhealthy choices like smoking, inactivity, and poor diet can cause peripheral artery disease (PAD) through blood vessel damage and plaque buildup. To lower the risk of PAD and its complications, healthy habits like quitting smoking, being active, and having a balanced diet can help.
- Smoking: Tobacco use, including cigarette smoking, significantly increases the risk of developing PAD. Smoking damages blood vessels, accelerates atherosclerosis (plaque buildup), and reduces blood flow, contributing to the progression of PAD.
- Sedentary lifestyle: Lack of regular physical activity and a sedentary lifestyle increase the risk of PAD. Physical inactivity contributes to obesity, hypertension, and other cardiovascular risk factors, exacerbating the progression of PAD.
- Poor diet: Diets high in saturated fats, trans fats, cholesterol, and sodium can contribute to atherosclerosis and PAD. Conversely, diets rich in fruits, vegetables, whole grains, and lean proteins may help lower the risk of PAD by promoting cardiovascular health.
Medical conditions
Medical conditions like diabetes, high blood pressure, and high cholesterol increase the risk of PAD. Proper management through medication, lifestyle changes, and medical monitoring is essential for reducing the risk and improving cardiovascular health.
- Diabetes: Individuals with diabetes have a higher likelihood of developing PAD due to elevated blood sugar levels that damage blood vessels and nerves. Diabetes also increases the risk of other cardiovascular complications associated with PAD.
- High blood pressure (hypertension): Hypertension is a significant risk factor for PAD as it places increased pressure on blood vessel walls, leading to endothelial damage and atherosclerosis. Uncontrolled high blood pressure further exacerbates the progression of PAD.
- High cholesterol: Elevated levels of cholesterol, mainly low-density lipoprotein (LDL) cholesterol ("bad" cholesterol), contribute to the formation of plaque within arteries, narrowing the blood vessels and impeding blood flow. This accelerates the development and progression of PAD.
- Obesity: Excess body weight, especially abdominal obesity, is associated with a higher risk of PAD. Obesity contributes to insulin resistance, inflammation, and dyslipidemia, all of which promote the development of atherosclerosis and PAD.
Genetic and age-related
PAD risk increases with age and genetics. A family history of cardiovascular disease also raises the likelihood. Be aware of these and other risk factors to assess and take preventive measures.
- Age: The risk of PAD increases with age, particularly in individuals over 50 years old. As people age, their blood vessels may become less flexible and more susceptible to atherosclerosis, leading to reduced blood flow and an increased risk of PAD.
- Family history: A family history of PAD or other cardiovascular diseases significantly elevates an individual's risk of developing PAD. Genetic factors can predispose individuals to high blood pressure, high cholesterol, and atherosclerosis.
Other medical conditions
Individuals with a history of other cardiovascular conditions, such as coronary artery disease or stroke, are at an increased risk of developing PAD. These conditions often share similar underlying mechanisms, including atherosclerosis and endothelial dysfunction. Managing these comorbidities effectively through medication, lifestyle changes, and regular medical care can help reduce the risk of PAD and its complications.
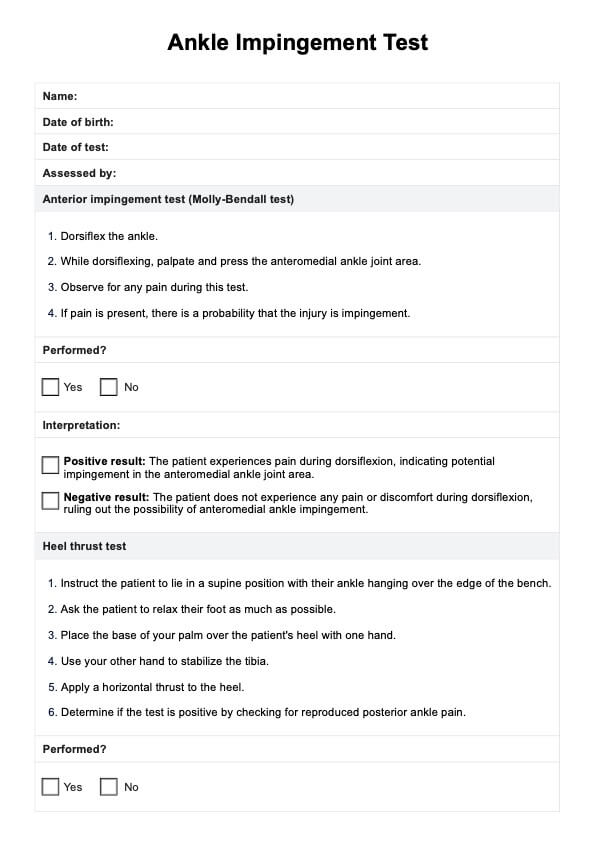
What is the PAD test?
The PAD test, also known as the ankle-brachial index (ABI) test, is a simple diagnostic procedure for assessing peripheral artery disease (PAD). PAD is a condition characterized by reduced blood flow to the lower limbs due to blockages or narrowing of the arteries.
Blood pressure measurements are taken at the ankle during the ABI test and compared to those at the arm. A lower ankle blood pressure cuff than the arm pressure indicates poor blood flow to the legs, suggesting the presence of PAD.
This non-invasive test helps diagnose PAD and assess its severity. It is often performed as part of a comprehensive evaluation for individuals with symptoms such as leg pain, particularly during physical activity (intermittent claudication), or those with risk factors for PAD, including smoking, diabetes, high blood pressure, and high cholesterol.
Early detection of PAD through the ABI test enables healthcare providers to implement appropriate treatment strategies, such as lifestyle modifications, medications, supervised exercise programs, and, in severe cases, interventions like angioplasty or bypass surgery.
Regular monitoring of ABI can also help track the progression of PAD and the effectiveness of treatment over time, ultimately improving outcomes and quality of life for individuals affected by this condition.
How to treat peripheral artery disease?
Treating peripheral artery disease (PAD) involves a multifaceted approach aimed at relieving symptoms, improving blood flow, and reducing the risk of complications. Here are key treatment strategies for PAD:
Lifestyle modifications
PAD can be effectively managed through lifestyle modifications. Here are some key areas to focus on:
- Smoking cessation: Quitting smoking is crucial for improving circulation and reducing further damage to blood vessels.
- Regular exercise: Supervised exercise programs, such as walking or cycling, can improve symptoms of PAD and cardiovascular health. Exercise increases collateral circulation and improves muscle function.
- Healthy diet: Adopting a heart-healthy diet low in saturated fats, cholesterol, and sodium and rich in fruits, vegetables, whole grains, and lean proteins can help control cholesterol levels and blood pressure, reducing the progression of atherosclerosis.
Medications
In addition to lifestyle modifications, medications play a crucial role in managing PAD. Your doctor will develop a personalized treatment plan based on your needs and risk factors. Here's an overview of some commonly prescribed medications for PAD:
- Antiplatelet agents: Medications like aspirin or clopidogrel may be prescribed to reduce the risk of blood clots and cardiovascular events.
- Cholesterol-lowering drugs: Statins and other lipid-lowering medications help lower LDL cholesterol levels, slowing the progression of atherosclerosis.
- Blood pressure medications: ACE inhibitors, beta-blockers, or calcium channel blockers may be used to manage hypertension and improve blood flow.
- Symptom management: Medications like cilostazol or pentoxifylline may be prescribed to alleviate intermittent claudication and improve walking distance.
Interventional procedures
In some cases, lifestyle modifications and medications may not be sufficient to manage PAD effectively. Interventional procedures can offer a solution to restore blood flow and alleviate symptoms. Here's an overview of some common procedures used for PAD:
- Angioplasty and stenting: Minimally invasive procedures such as angioplasty with or without stenting can be performed to open blocked or narrowed arteries, restoring blood flow.
- Atherectomy: In some cases, atherectomy may be used to remove plaque buildup from the artery walls, improving blood flow.
- Bypass surgery: For severe cases of PAD, bypass surgery may be necessary to reroute blood flow around blocked arteries, typically using a vein or synthetic graft.
Wound care
Proper wound care is essential for individuals with PAD-related wounds or ulcers to prevent infection and promote healing. This may include regular cleaning, debridement, and application of dressings.
Diabetes management
Tight control of blood sugar levels is critical for individuals with diabetes and PAD, as elevated blood sugar levels can exacerbate arterial damage and impair wound healing.
Regular monitoring and follow-up
Individuals with PAD require regular monitoring of symptoms, their blood pressure readings, cholesterol levels, and overall cardiovascular health. Close follow-up with healthcare providers helps track disease progression and adjust treatment.
Education and support
Patient education plays a vital role in PAD management. Information about the condition, its risk factors, and the importance of adherence to treatment and lifestyle modifications empowers patients to take an active role in their health.
Commonly asked questions
Standard tests for PAD include the ankle-brachial index (ABI) test, Doppler ultrasound, magnetic resonance angiography (MRA), and computed tomography angiography (CTA). Blood tests and physical examinations are also performed to assess symptoms and risk factors.
While there's no substitute for a medical evaluation, you can check for PAD at home by monitoring symptoms like leg pain during walking, slow-healing wounds, or changes in skin color or temperature in the lower limbs. However, a severe healthcare provider or professional should confirm a diagnosis using appropriate tests.
The ankle-brachial index (ABI) test is considered the most sensitive test for PAD. It compares blood pressure in the ankles to that in the arms and helps assess the severity of arterial blockages or narrowing in the legs.