Healthcare practitioners, including physicians and toxicologists, often request Osmolar Gap Tests. These tests are commonly ordered when toxic alcohol ingestion is suspected or in cases of uncontrolled diabetes or renal dysfunction.
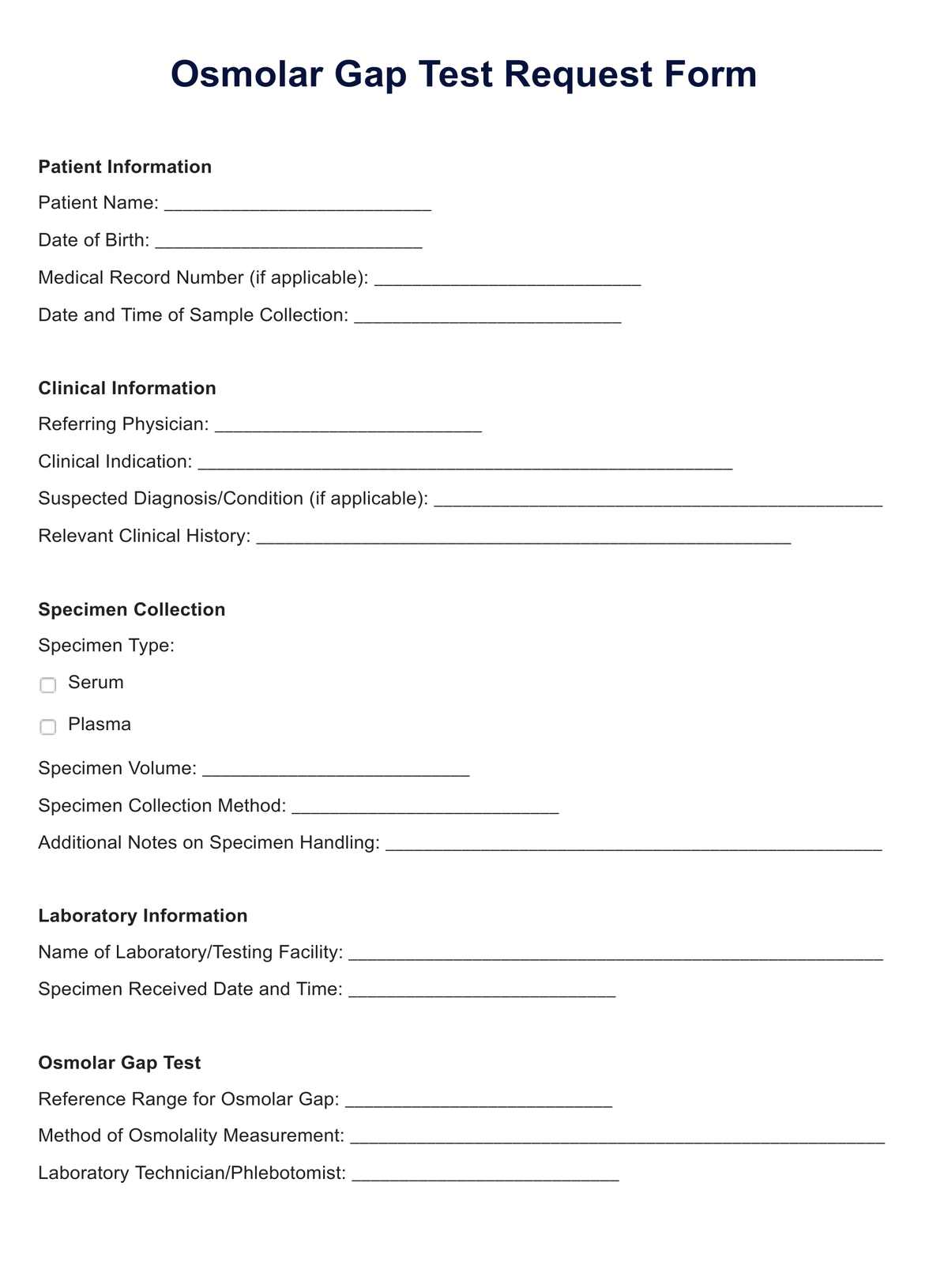
Efficiently request and document Osmolar Gap Tests with our comprehensive sample template. Simplify clinical assessment for timely patient care.
Healthcare practitioners, including physicians and toxicologists, often request Osmolar Gap Tests. These tests are commonly ordered when toxic alcohol ingestion is suspected or in cases of uncontrolled diabetes or renal dysfunction.
Osmolar Gap Tests are used in situations where there is a need to assess toxic alcohol poisoning, investigate uncontrolled diabetes, monitor renal function, or evaluate patients with unexplained altered mental status.
To perform an Osmolar Gap Test, a blood sample is collected from the patient, sent to a clinical laboratory for analysis, and the osmolality of the blood is measured. The test results are then compared to determine if there's an elevated or reduced osmolar gap.
EHR and practice management software
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments