Nursing Assessment of Eye
Explore comprehensive guidelines for nursing eye assessments, including techniques, common disorders, and the benefits of using Carepatron.


What is an eye assessment for nursing?
An eye assessment in nursing is a critical component of a comprehensive health evaluation to identify potential vision problems, eye disorders, or symptoms of systemic diseases manifesting through the eyes. This assessment involves subjective and objective evaluations, where nurses gather information about the patient's vision and eye health history (subjective) and perform physical examination techniques (objective) to assess the current state of the eyes. This dual approach ensures a thorough understanding of the patient's ocular health, guiding further diagnostic testing or treatment as necessary.
Subjective assessment
The subjective part of the eye assessment involves interviewing the patient to gather information on any symptoms they are experiencing, such as poor balance, difficulty reading, or vision changes. Nurses also inquire about corrective lenses, a history of eye disorders, and recent use of medications like eye drops that could affect vision. This phase is used to identify when the patient displays behavioral cues that may indicate vision problems or discomfort.
Objective assessment
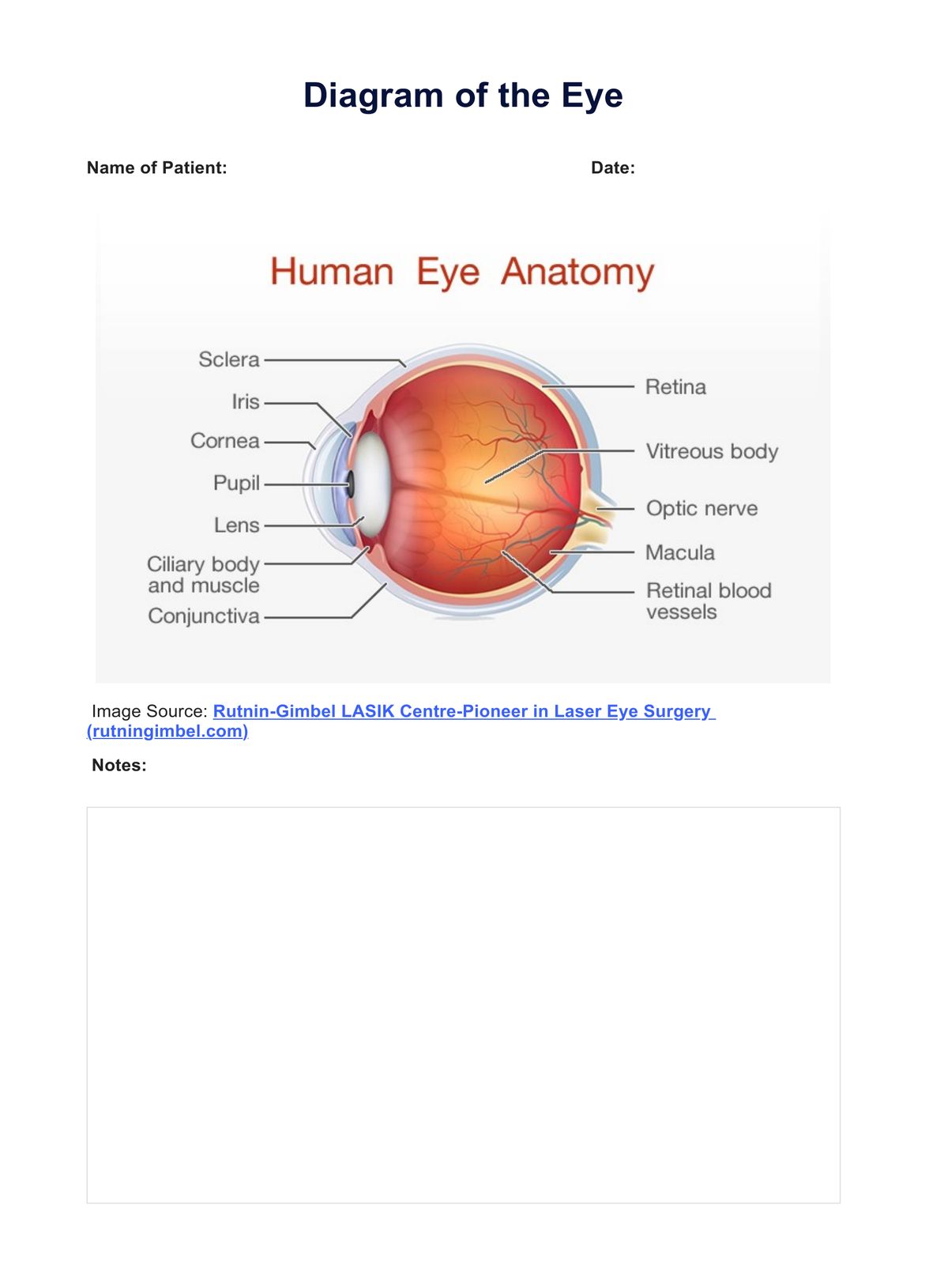
Objective assessment includes physical examination techniques performed to evaluate the health and function of the eyes. This can involve a vision screening test using an eye chart to measure visual acuity, examining the external and internal structures of the eye, and conducting specialized tests like the PERRLA (Pupils Equal, Round, Reactive to Light and Accommodation) exam. These assessments help determine if the patient demonstrates good balance, coordination, and overall eye health.
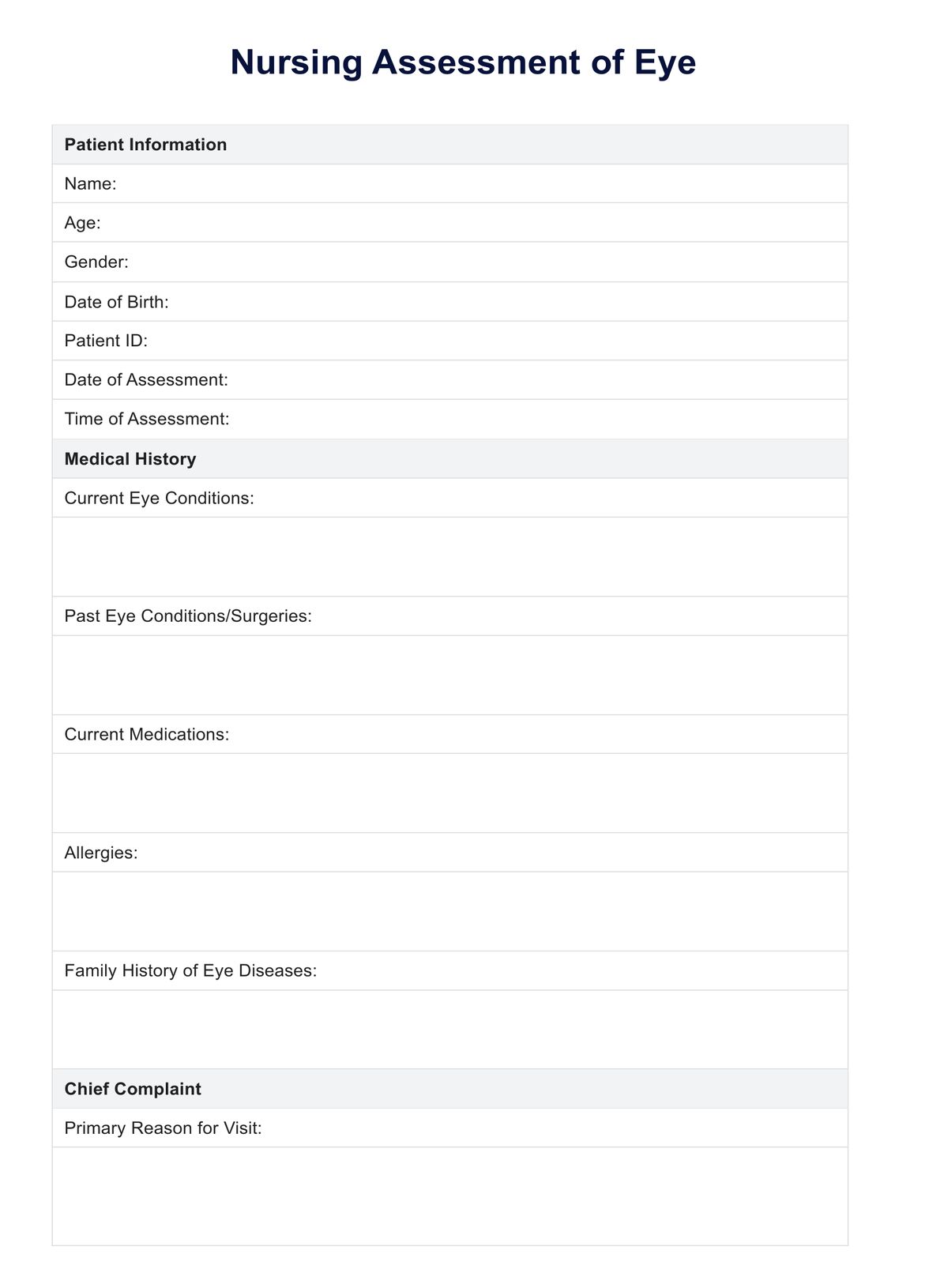
Nursing Assessment of Eye Template
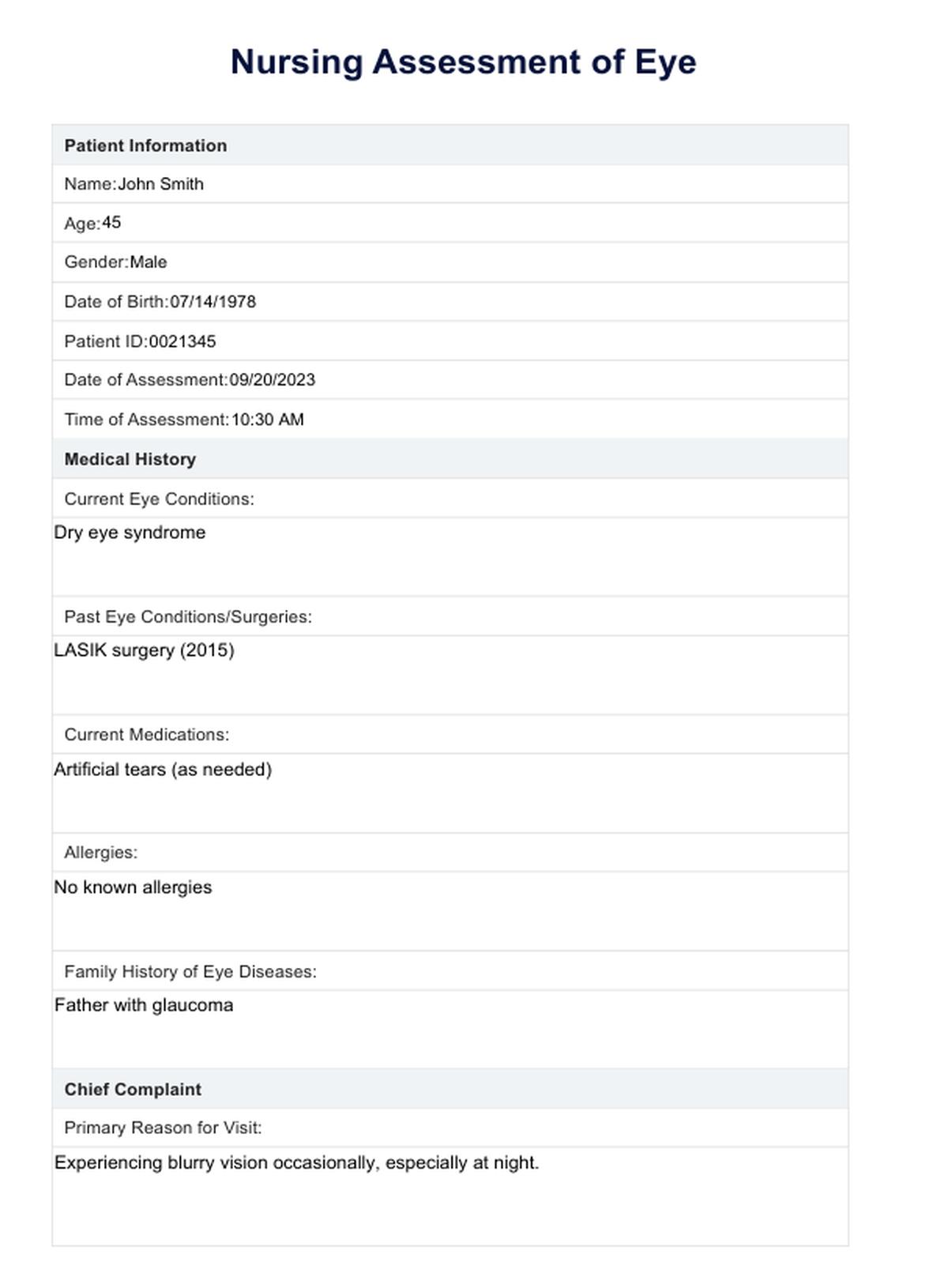
Nursing Assessment of Eye Example
Assessment findings
During a nursing eye assessment, several findings can be observed:
Normal assessment findings
Normal findings in an eye assessment include clear vision, with or without corrective lenses, pupils equal in size, round, and reactive to light and accommodation, and no signs of infection, inflammation, or structural abnormalities in one eye. Good balance, coordination, and the ability to follow objects smoothly with both eyes are also indicators of healthy eye function.
Abnormal assessment findings
Abnormal findings may include discrepancies in visual acuity between the two eyes, signs of infection (redness, discharge), structural abnormalities (irregular pupil shape), or cataracts or glaucoma. Behavioral cues such as squinting, frequent blinking, or difficulty focusing can also indicate vision problems.
Common eye disorders
Common eye disorders are a significant focus of nursing assessments due to their prevalence and potential impact on patient's quality of life. These conditions can range from refractive errors affecting the eye's ability to focus light correctly to more severe disorders that can lead to vision loss if not properly managed. Understanding these common disorders is crucial for nurses as they play a pivotal role in the early detection and management of eye health issues.
Refractive errors
Refractive errors are among the most common eye disorders, including myopia (nearsightedness), hyperopia (farsightedness), and astigmatism. Myopia occurs when the eye's shape causes light rays to focus in front of the retina, with impaired vision and making distant objects appear blurry. Conversely, hyperopia results from light focusing behind the retina, causing difficulty focusing on close objects. Astigmatism is characterized by an irregular curvature of the cornea or lens, leading to distorted or blurred vision at any distance. These conditions are typically corrected with eyeglasses, contact lenses, or refractive surgery.
Cataracts
Cataracts involve the clouding of the eye's natural lens, which lies behind the iris and the pupil. This clouding can lead to decreased vision and, if left untreated, blindness. Cataracts are most commonly related to aging but can also result from trauma, radiation exposure, or being present at birth. The primary treatment for cataracts is surgical removal of the cloudy lens, usually replaced with an artificial lens.
Glaucoma
Glaucoma is a group of eye conditions that damage the optic nerve, essential for good vision, and is often linked to abnormally high pressure in the eye. Without treatment, glaucoma can lead to vision loss or complete blindness. Early detection through regular eye exams is vital since the damage caused by the disease can be minimized with treatment options such as prescription eye drops, oral medications, or surgery.
Macular degeneration
Macular degeneration, specifically age-related macular degeneration (AMD), affects the macula, the part of the retina responsible for clear vision in your direct line of sight. This condition can result in a loss of central vision, affecting the ability to see fine details, read, or recognize faces. While there is no cure for AMD, treatments like medication injections, laser therapy, and lifestyle changes can slow its progression.
Diabetic retinopathy
Diabetic retinopathy is a diabetes complication that affects the eyes, caused by damage to the blood vessels of the light-sensitive tissue at the back of the eye (retina). It can lead to blindness if not diagnosed and treated promptly. Management of diabetes is crucial to preventing diabetic retinopathy, along with regular eye exams and treatments that may include laser treatment or surgical intervention.
Nurses play a critical role in the early detection of these common eye disorders through thorough assessments and patient education. By identifying signs and symptoms early, nurses can facilitate timely referrals to eye care professionals, significantly improving outcomes and helping to preserve patients' vision.
You can also use the Prescription Template to document and manage medication details effectively. This template helps in tracking prescribed drugs, dosages, and patient instructions. Additionally, the Vision Screening Test Template assists in evaluating and recording visual acuity and eye health, ensuring comprehensive patient assessments. Utilizing both templates can enhance your ability to provide thorough and accurate patient care.
Commonly asked questions
An eye assessment should include a detailed history, a vision test and screening, an examination of the eyelids, conjunctiva, sclera, cornea, iris, lens, fundus, pupil reactivity tests (PERRLA), and an assessment of ocular movements.
Eye assessments are conducted to identify any current vision problems, risk of future eye conditions, and signs of systemic diseases manifesting through ocular symptoms. Early detection and management of eye issues can prevent vision loss and improve overall health.
Steps in eye assessments include preparing the patient and environment, conducting a thorough history review, performing vision screening tests, examining the external and internal eye structures, assessing vision and pupil response, and evaluating eye movements and alignment.

.jpg)