When skin remains tented or elevated after pinching, it can indicate dehydration or, in some cases, issues related to aging or connective tissue disorders.
Skin Turgor Test
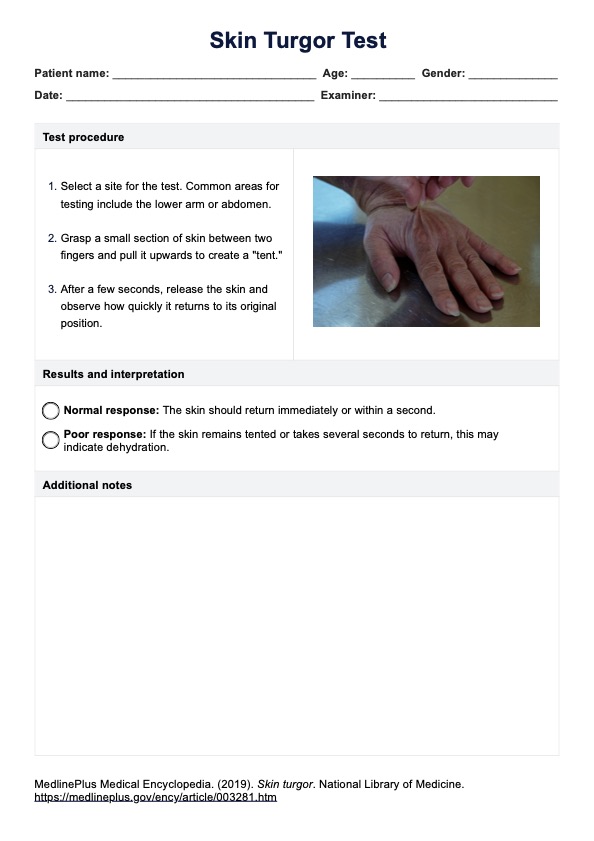
Learn about the Skin Turgor Test, a quick method to assess hydration and diagnose dehydration by observing skin elasticity.
Use Template
Skin Turgor Test Template
Commonly asked questions
Yes, dehydration often affects skin appearance and elasticity, leading to symptoms like dryness, dullness, and poor skin turgor. You can assess skin turgor using the skin pinch test, a very simple and quick skin dehydration test.
A decrease in skin turgor usually indicates dehydration or a loss of skin elasticity, which could be due to aging, certain medical conditions, or fluid imbalance.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











