MRSA
Discover the key to accurate MRSA testing and get the results you need. Find out how it works and why it matters to your health today.


What Is an MRSA Test?
An MRSA test, or Methicillin-Resistant Staphylococcus Aureus test, is a medical diagnostic procedure used to identify the presence of MRSA bacteria in a patient's body. MRSA is a strain of Staphylococcus aureus, a common bacterium that can cause various infections, including skin infections, pneumonia, and bloodstream infections. What makes MRSA particularly concerning is its resistance to many antibiotics, including methicillin, which is why it is termed "methicillin-resistant."
The primary purpose of the MRSA test is to diagnose MRSA infections in patients. This is essential because MRSA requires different treatment strategies than non-resistant staph infections. Identifying MRSA also allows healthcare providers to choose appropriate antibiotics. MRSA is often resistant to common antibiotics, so alternative medications are required.
Moreover, patients may be screened for MRSA before surgery to determine if they are carriers. This information can help prevent surgical site infections.
There are different methods for conducting an MRSA test, including swabbing the nose, throat, or wounds and culturing the samples to detect the presence of the bacteria. In some cases, molecular techniques like polymerase chain reaction (PCR) can be employed for quicker results.
Timely MRSA testing and accurate identification are crucial in preventing the spread of these drug-resistant bacteria and tailoring treatment plans to individual patients. The results of the MRSA test guide healthcare professionals in making informed decisions for the well-being of their patients and the overall public health.
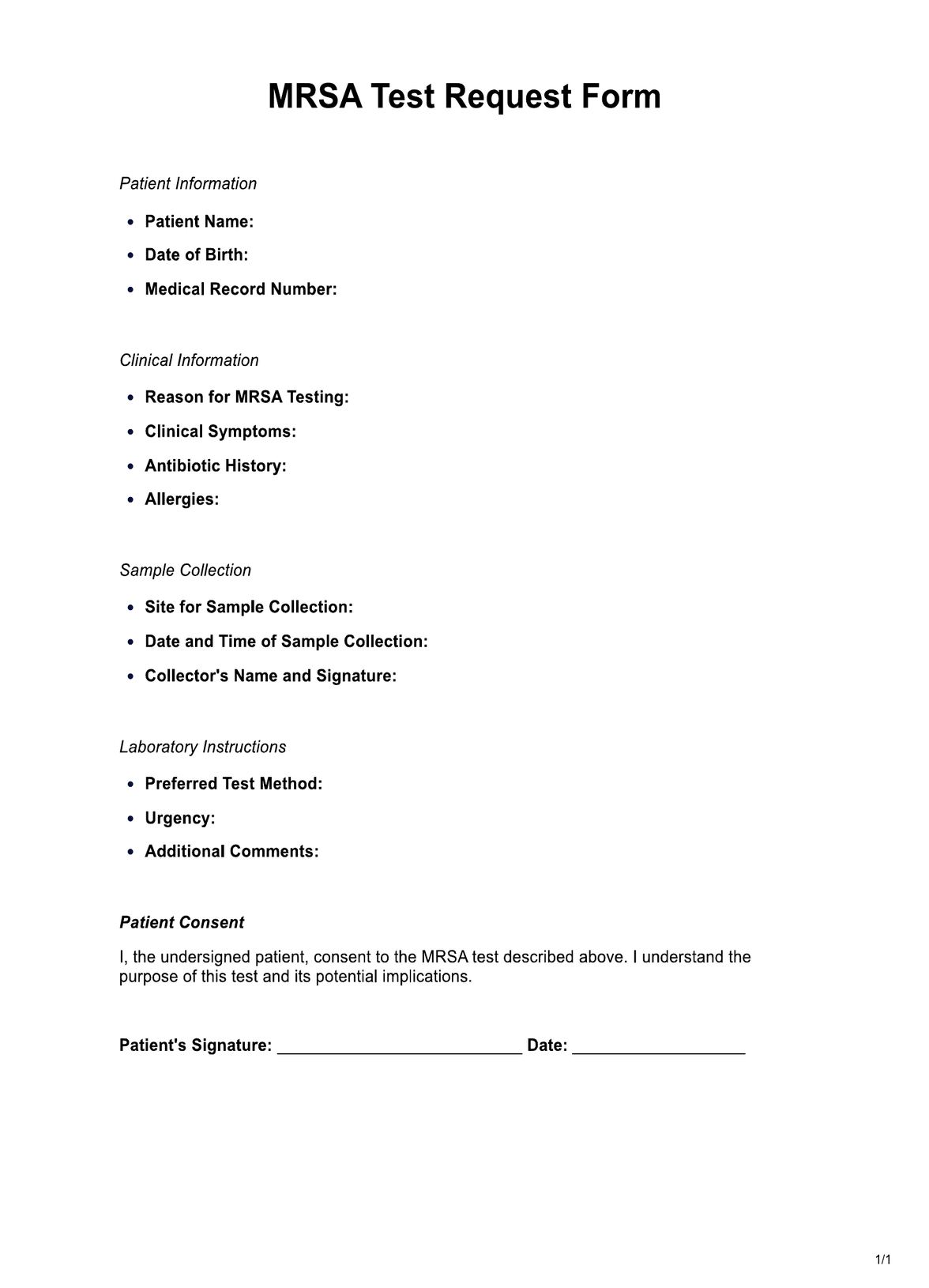
MRSA Template
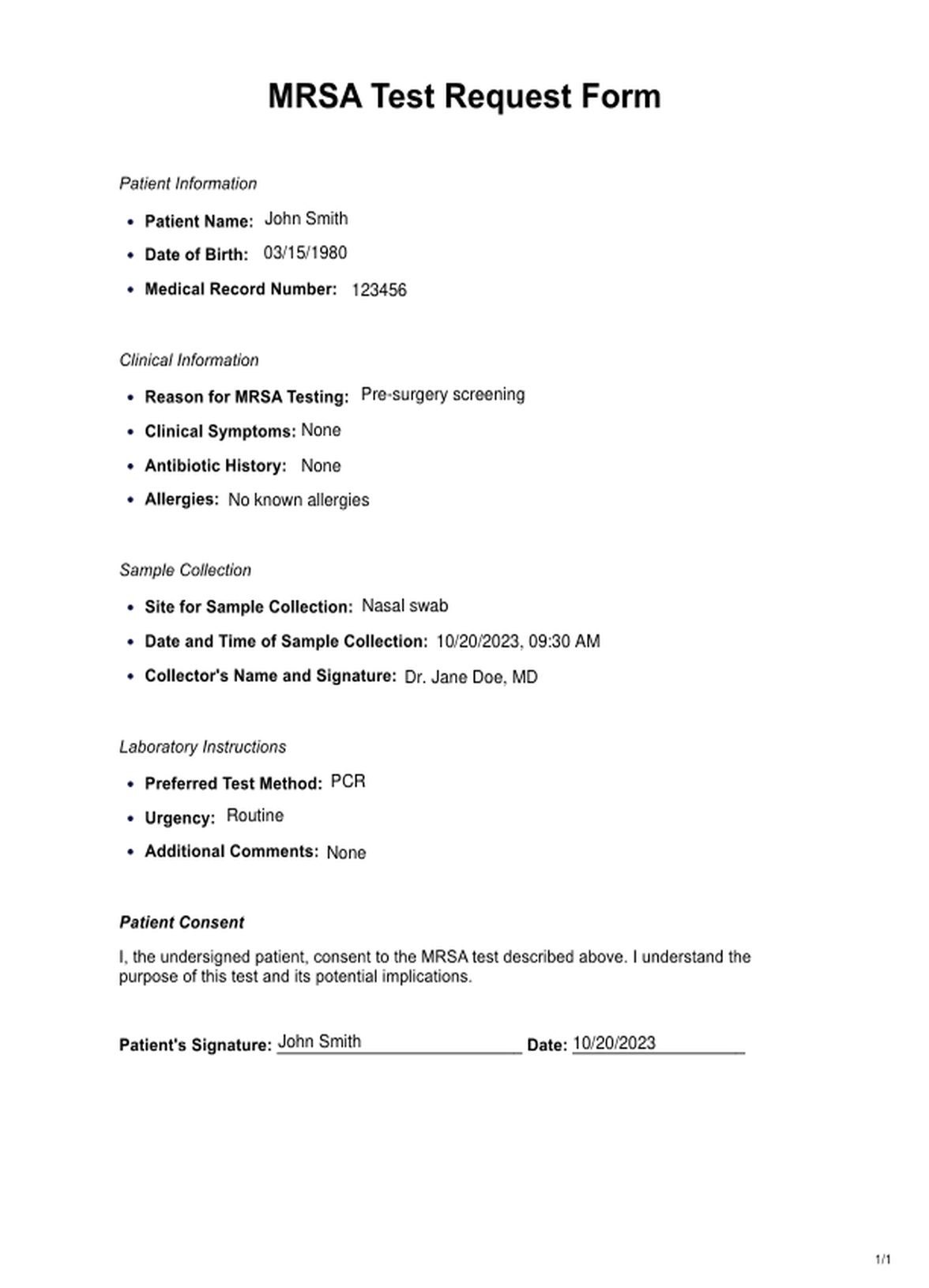
MRSA Example
How Does it Work?
Step 1: Preparation
Gather necessary materials. This includes a sterile swab or culture collection kit. Wash hands and wear disposable gloves to prevent contamination.
Step 2: Sample Collection
Select the sampling site. Common sites for swabbing include the nose, throat, or skin wounds.
Using a sterile swab, gently rotate it in the selected area to collect a sample of secretions or bacteria. Place the swab in a sterile tube or container. Ensure proper labeling with patient information and the sampling site.
Step 3: Transportation
Keep the sample at the right temperature to preserve its integrity. Deliver the sample to a laboratory within the recommended time frame to avoid degradation.
Step 4: Culturing
The sample is streaked in the laboratory onto a culture plate containing a special medium that promotes MRSA growth. The culture plate is then incubated at a specific temperature for a prescribed time (usually 24-48 hours).
Step 5: Examination
Microbiologists examine the culture plate for MRSA colonies. Then, the bacteria's characteristics, such as appearance and specific antibiotic resistance patterns, are used to confirm MRSA's presence.
Step 6: Reporting
Results are reported to the healthcare provider, who then communicates the findings to the patient. Based on the test results, the healthcare provider can prescribe appropriate antibiotics if MRSA is detected.
Step 7: Infection Control
If MRSA is confirmed, infection control measures may be initiated, especially in healthcare settings, to prevent further transmission.
When Would You Use This Test?
The MRSA test is a crucial diagnostic tool used in various medical scenarios, primarily by healthcare practitioners, to determine the presence of Methicillin-Resistant Staphylococcus Aureus (MRSA) bacteria. Below are key situations and settings where the MRSA test is appropriately used:
- Pre-Surgery Screening: Patients scheduled for surgery are often tested for MRSA to identify carriers and implement infection control measures, reducing the risk of surgical site infections.
- Admission Screening: Hospitals may conduct MRSA tests on patients admitted to high-risk units (e.g., intensive care, neonatal) to prevent the spread of MRSA within the facility.
- Outbreak Management: During MRSA outbreaks in healthcare settings, the test identifies cases and implements control measures.
- Skin and Soft Tissue Infections: MRSA testing is appropriate for individuals with skin or soft tissue infections that are not responding to standard antibiotics.
- Respiratory Infections: Healthcare providers may order MRSA tests when patients risk pneumonia or respiratory tract infections.
- Resident Screening: MRSA tests screen residents and staff in nursing homes and long-term care facilities to prevent MRSA spread.
- Inmate Health: MRSA testing may be used to monitor and control MRSA in correctional facilities where close quarters facilitate transmission.
- Immunocompromised Patients: Individuals with weakened immune systems are more susceptible to MRSA, and testing helps in early detection and management.
- Close Contacts: Family members or close contacts of MRSA patients may be tested to prevent transmission.
- Schools and Sports Teams: In cases of MRSA outbreaks in schools or sports teams, testing may be recommended to identify carriers and control the spread.
- Surveillance Studies: Public health agencies and researchers may conduct MRSA tests to track the prevalence of MRSA in communities, helping to monitor trends and develop effective preventive strategies.
What do the Results Mean?
Interpreting the results of an MRSA test is crucial in guiding patient care and infection control measures. The test can yield various outcomes; understanding them is essential for appropriate management. Here are common results and their meanings:
Negative Result
No MRSA Detected: A negative result indicates that MRSA bacteria were not found in the sample. This is reassuring, as it means the patient is not currently carrying MRSA. However, it doesn't guarantee they will not become colonized or infected.
Positive Result
MRSA Detected: A positive result signifies the presence of MRSA in the sample. This indicates the patient is carrying MRSA at the time of testing. In a clinical context, this result may lead to several actions:
- Isolation: In healthcare settings, the patient may be isolated to prevent MRSA transmission to others.
- Treatment: If the patient is symptomatic or at high risk of infection, treatment with specific antibiotics effective against MRSA may be initiated.
- Infection Control: Stringent infection control measures will be enforced to limit MRSA spread.
Indeterminate Result
Inconclusive: Sometimes, test results may be inconclusive due to various reasons, such as a low bacterial load or issues with the sample. In such cases, retesting may be necessary to obtain a definitive result.
Colonization vs. Infection
It's important to note that a positive MRSA test may indicate colonization (the bacteria are present but not causing an infection) rather than an active infection. Clinical judgment and further assessment are required to determine whether treatment is necessary.
Community Implications
Positive results in community settings, such as schools or sports teams, may prompt public health interventions, including education about hygiene, isolation, and treatment for affected individuals.
You can enhance your practice with the Medical Record Template. This template ensures thorough documentation of patient information, which is essential for accurate record-keeping and effective care planning.
Research & Evidence
Methicillin-resistant Staphylococcus Aureus (MRSA) was first identified in the early 1960s, soon after the introduction of synthetic antibiotic methicillin. MRSA strains were noted to resist methicillin and other penicillin-like antibiotics.
Early methods for identifying MRSA were culture-based, relying on laboratory techniques to isolate and identify the bacterium. These methods were time-consuming and required skilled technicians. Over time, as MRSA posed a growing threat in healthcare settings, there was a need for faster and more reliable testing methods.
In the 1990s, molecular techniques like Polymerase Chain Reaction (PCR) became a significant breakthrough in MRSA testing. PCR allowed for the rapid and accurate detection of MRSA genetic material, providing quicker results than traditional cultures. Evidence from research studies demonstrated the sensitivity and specificity of PCR-based tests, supporting their use as reliable diagnostic tools.
Extensive epidemiological studies have been conducted to understand the prevalence and transmission of MRSA. These studies have informed infection control strategies, emphasizing the importance of early detection and prevention.
The rise of MRSA is closely linked to antibiotic resistance. Extensive research on MRSA's antibiotic resistance mechanisms has deepened our understanding of how the bacterium evolves and spreads.
The development of clinical guidelines by healthcare organizations, such as the Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO), has been based on research and evidence. These guidelines recommend MRSA testing in specific clinical scenarios to ensure appropriate patient care and infection control.
Public health agencies conduct surveillance and research to monitor MRSA trends and develop strategies to reduce its impact on communities.
References
- County Durham & Darlington NHS Foundation Trust. (2017, January 31). MRSA screening at County Durham and Darlington NHS Foundation Trust [Video]. YouTube. https://www.youtube.com/watch?v=fkjO19i9Mzc
- Polisena, J., Chen, S., Cimon, K., McGill, S., Forward, K. R., & Gardam, M. (2011). Clinical effectiveness of rapid tests for methicillin-resistant Staphylococcus aureus(MRSA) in hospitalized patients: a systematic review. BMC Infectious Diseases, 11(1). https://doi.org/10.1186/1471-2334-11-336
- UpToDate. (n.d.). UpToDate. https://www.uptodate.com/contents/rapid-detection-of-methicillin-resistant-staphylococcus-aureus
Commonly asked questions
Healthcare professionals, including doctors and nurses, typically request MRSA tests. They may be ordered for patients before surgery, those with suspected infections, or in high-risk settings like hospitals, long-term care facilities, and correctional institutions.
MRSA tests are used in various situations:
- Pre-surgery screening to prevent surgical site infections.
- When patients have skin or respiratory infections that don't respond to standard antibiotics.
- In healthcare settings, to monitor and control MRSA outbreaks.
- For residents and staff in long-term care facilities.
- In community settings during outbreaks or among high-risk individuals.
MRSA tests involve taking a sample, often a swab from the nose, throat, or a wound. The sample is then cultured in a laboratory or tested using molecular techniques like PCR to detect MRSA bacteria.